Strategic Options for the
Modernization of the
Indian Health Service
Health Information Technology
Final Report
October 2019
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
1
Table of Contents
Vision Statements 2
Executive Summary 3
People and Process 7
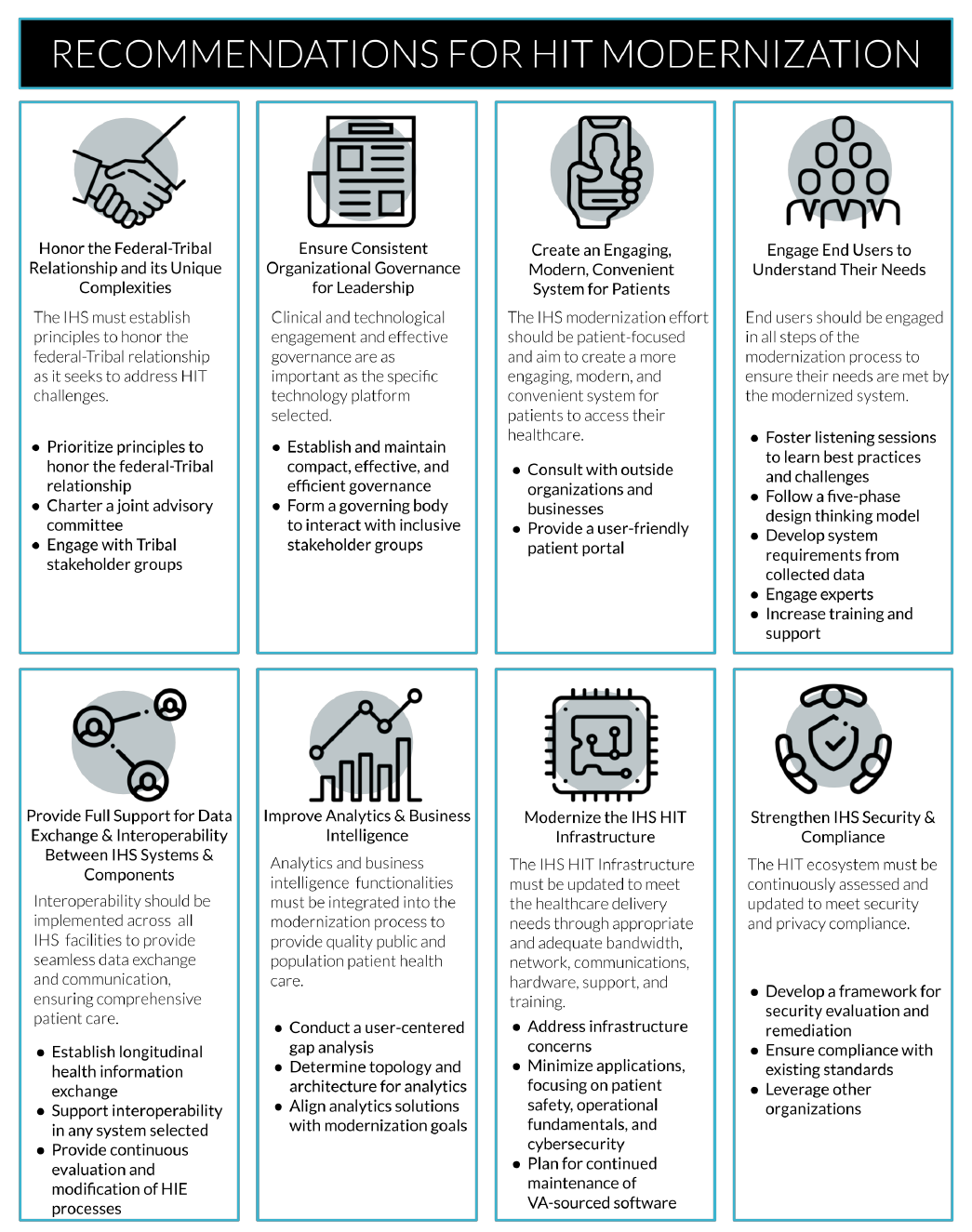
Honor the Federal-Tribal Government Relationship and its Unique Complexities 7
Create an Engaging, Modern, Convenient System for Patients 9
Ensure Consistent Organizational Governance for Leadership 11
Technology 12
Engage End Users to Understand Their Needs 12
Provide Full Support for Data Exchange and Interoperability Between IHS Systems and
Components 14
Improve Analytics and Business Intelligence 16
Modernize the IHS HIT Infrastructure 16
Strengthen IHS HIT Security and Compliance 19
Next Steps 20
References 21
Appendix A: Constraints and Mitigations to the HIT Modernization Effort 22
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
2
Vision Statements
IHS HIT Modernization Project Vision
Support the Indian Health Service (IHS) mission to raise the physical, mental, social, and spiritual health
of American Indians and Alaska Natives (AI/AN) to the highest level
1
through modern, innovative, and
practical health information technology.
IHS Vision
Healthy communities and quality healthcare systems through strong partnerships and culturally responsive
practices.
1
IHS Office of Information Technology (OIT) Vision
To meet customer needs by providing excellent, reliable, interoperable health information services that
protect privacy while connecting patients, providers, and payers, enabling improved patient outcomes and
controlled costs in support of the IHS mission.
2
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
3
Executive Summary
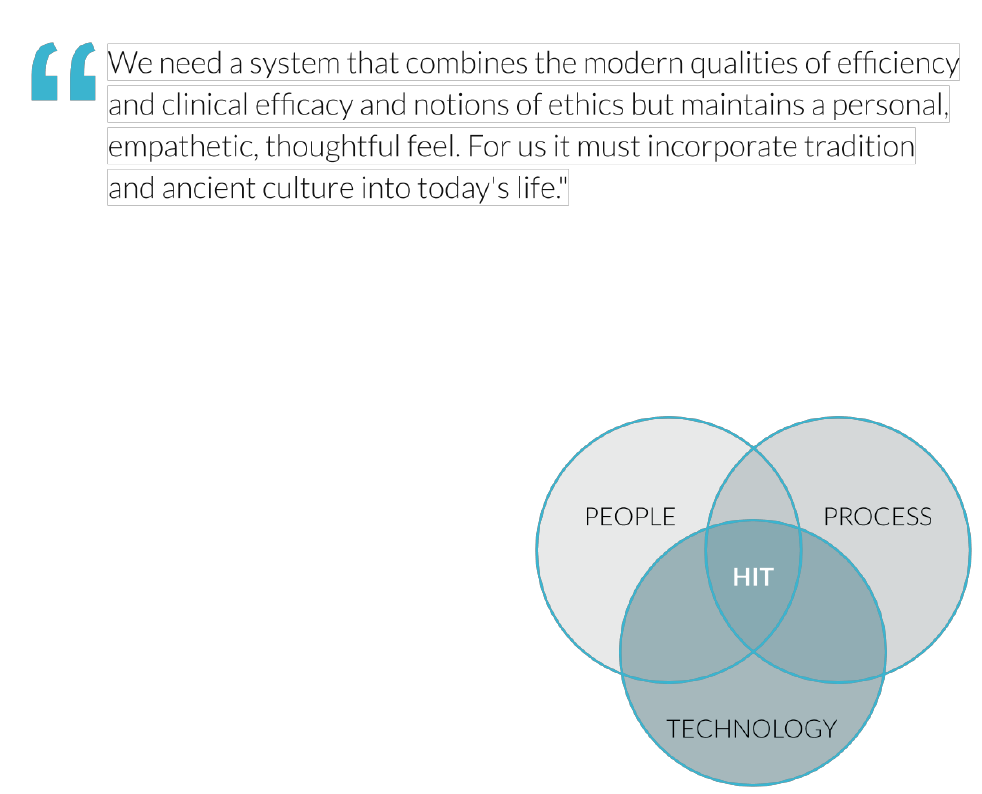
The Department of Health and Human Services (HHS) IHS Health Information Technology (HIT)
Modernization Project provides a comprehensive assessment of the people, process, and technology that
comprise the existing IHS HIT system, including the Resource and Patient Management System (RPMS).
From its inception, the Modernization Project embraced a human-centered design methodology and was
committed to the following principles:
● Honor and respect tribal communities and
stakeholders
● Be people-centered
● Utilize impactful, community-serving processes
● Be data-driven in all decision making
These principles provided the framework for the analysis
of HIT within the IHS ecosystem. IHS facilities provide
cradle-to-grave care that requires personal, family, and
community health data for informed clinical decision-
making. IHS and Tribal facilities have an additional
commitment to the inclusion of community care, public
and population health, and environmental health and
epidemiology, making IHS a unique federal healthcare
delivery model.
1
The pledge to respect AI/AN self-
determination, the increase in government regulation of
healthcare, and the transformation of HIT requirements and capabilities nationwide have resulted in an
ever-changing milieu for AI/AN healthcare delivery. Understanding this complexity is critical to the HIT
modernization effort.
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
4
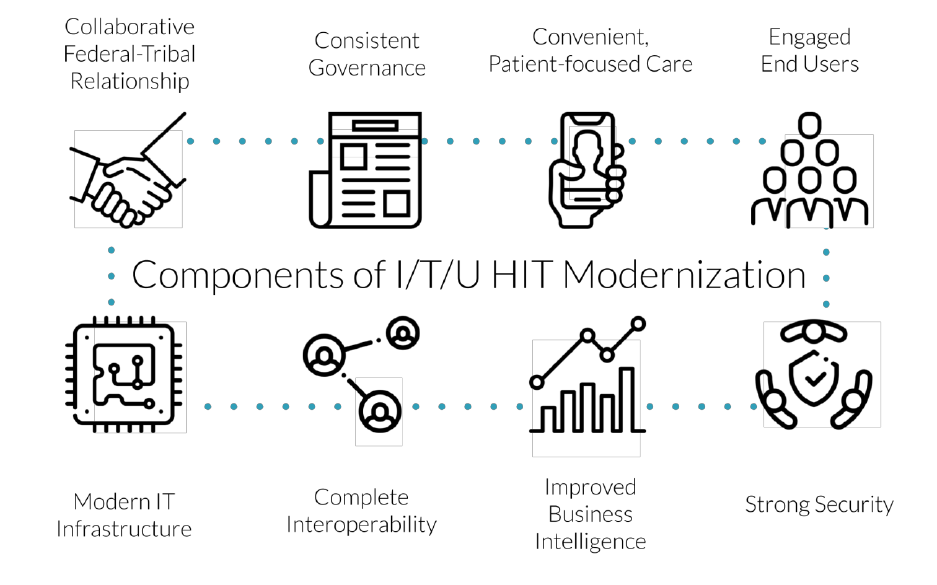
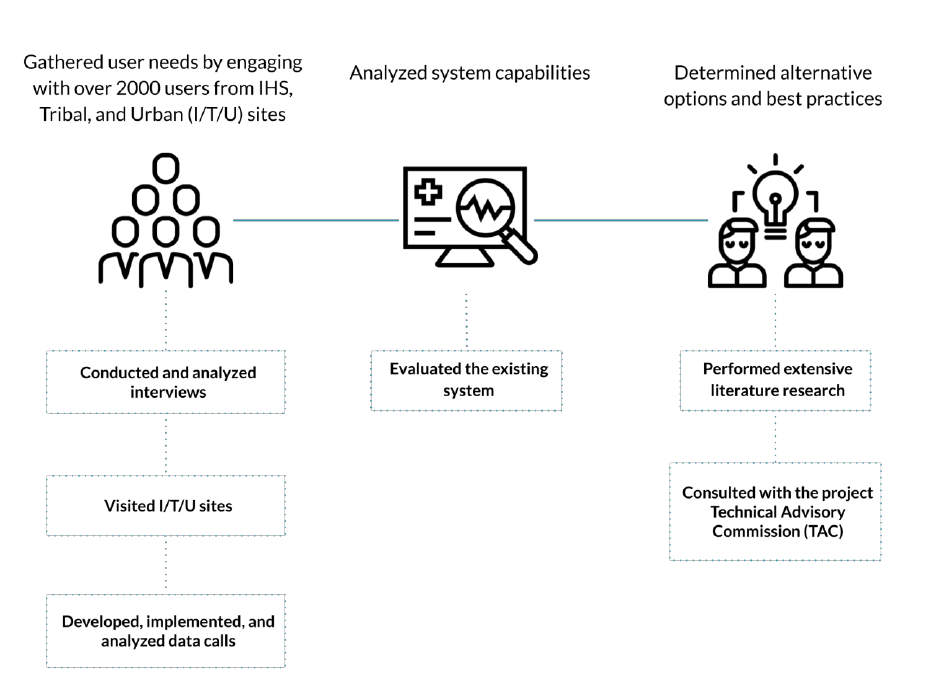
A Three-Pronged Approach
The project team developed and implemented the following three-pronged approach to better understand
the current state of the IHS HIT systems and the unique needs of the users that they serve.
To execute the project, the team:
The modernization roadmap work initiatives
6
address the insights identified over the course of the project
through multiple channels. These insights were transformed into the eight recommendations described
below. The recommendations address high-priority concerns identified during field visits and/or direct
contact with healthcare providers, leadership, and other users and consumers of HIT.
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
5
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
6
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
7
People and Process
Honor the Federal-Tribal Government Relationship and its
Unique Complexities
The IHS must establish principles to honor the federal-Tribal relationship as it
seeks to address health IT challenges.
The Challenge
Federally-recognized American Indian and Alaskan Native
tribes and villages have a government-to government
relationship with the United States. This unique
relationship has been given substance through the U.S.
Constitution, treaties legislation, Supreme Court decisions,
and Executive Orders.
Healthcare delivery has evolved due to Indian self-
determination, the increase in government regulation of
healthcare, and the transformation of HIT requirements and
capabilities nationwide. The mission has not changed,
however, and as the agency seeks to address deficiencies
and challenges in HIT, it must remain engaged with its partners in that mission. Understanding the
complexity of the policies and barriers affecting funding, unique challenges in Indian Health Service,
tribally operated, or urban Indian health programs (ITU) operations, reporting requirements imposed by
multiple funders, a history of research affecting Tribal policies on data ownership, and increasing health
compliance and accreditation standards demand that any HIT system address the need for commonly-
accepted performance standards and streamlined, more intuitive data capture and reporting. Failure to
address these systemic HIT deficiencies will result in future negative financial consequences for AI/AN
people and tribes.
The IHS is not just another HHS program; IHS’s mission which is to provide healthcare specifically for
AI/AN people, is consistent with the nation-to-nation relationship and the authority granted the agency by
Congress. A commitment to honor the Federal-Tribal partnership ensures that the process and outcomes
meet the needs of the federal government and the Tribal nations.
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
8
Recommended Approach
The following actions will help honor and strengthen the federal-Tribal relationship and improve trust
between tribes and the IHS.
● At the start of the HIT modernization planning and decision-making process, prioritize principles
which honor the federal-Tribal relationship at the highest levels of IHS
● Charter a HIT Modernization Advisory Committee to support the collaboration necessary to
advance innovation for technology improvements for the entire I/T/U health delivery system.
Representation should include members who are recognized subject matter experts and have a
collective working understanding of the I/T/U’s mission, business models, Self-Governance
policies, and the opportunities available to address unique intra- and interoperability and data
requirements
● HHS/IHS should formalize immediate and continuous engagement with the various key
stakeholder groups, including Direct Service tribes, Self-Governance tribes and Urban Indian
programs within the I/T/U ecosystem
10
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
9
Create an Engaging, Modern, Convenient System for Patients
The IHS modernization should be patient-focused and aim to create a more
engaging, modern, and convenient system for patients to access their healthcare.
The Challenge
The ability for patients and caregivers to easily access and understand medical information from wherever
they may be has become increasingly important and relatively standard practice in most healthcare
settings. Currently, facilities using the existing HIT system within the I/T/U network have the ability to
offer their patients a way to access some of their health information through a Personal Health Record
(PHR).
11
However, the PHR is not being well utilized and at many sites is not yet available for use by
patients.
Forty percent (40%) of respondents to
the Modernization Project Data Call
rated the electronic sharing of
information with patients through a
portal as “very poor” or “somewhat
poor.”
12
Staff who are familiar with the
PHR either as patients themselves at
the facility or through patient
comments have reported that the PHR,
in its current state, is difficult to
navigate, contains ineffective patient education material, and does not include relevant clinical
information. Additionally, patients may not always possess the necessary technology to access the PHR in
its current state. In these instances, it is vital for providers to be able to print and provide patients with
relevant, readable information, however this functionality is also lacking in the current system. Tribal
health directors who were surveyed for this project rated the increased ability to create and distribute
patient-centered care plans as one of their top desires.
13
Patients have expressed the desire to access their information, order their medications, schedule their own
appointments, and send messages to their care team.
12
Administrative personnel have noted that if patients
had the ability to access their own records to make updates to demographic and contact information, it
would improve accuracy and save time now spent in waiting rooms. Case managers and providers have
noted that if they had a more efficient way of communicating with their patients, they would feel more
confident that they are engaging more effectively with their patients.
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
10
Recommended Approach
● Improve patient engagement and satisfaction by providing a portal for patients to update their
information, view lab results, schedule appointments, communicate with their healthcare team,
refill prescriptions, and obtain culturally-relevant healthcare materials
● Embrace the concept of open notes for shared viewing by patients
● Consult outside organizations and businesses who frequently survey customer satisfaction to
understand how to create a convenient, intuitive, modern experience for their patients
● Develop appropriate continuous metrics to support quality and patient safety, including
longitudinal patient and healthcare team satisfaction

⠠⠠⠠⠠HHS/IHS HIT Modernization Project
11
Ensure Consistent Organizational Governance for Leadership
Clinical and technological engagement and effective governance is as important as
the specific technology platform selected.
The Challenge
Congress has recognized the right of tribes to direct the development and implementation of federal
programs and policies that directly impact their Tribal members by enacting two major pieces of
legislation. This legislation outlines the important concepts of Tribal self-determination and self-
governance: The Indian Self-Determination and Education Assistance Act of 1975, as amended (25 U.S.C.
450 et seq.)
14
and the Tribal Self-Governance Act of 1994 (25 U.S.C. 458aa et seq).
15
Through these laws,
Congress accorded Tribal governments the authority to administer programs and services usually
administered by the Indian Health Service (IHS) for their Tribal members. It also upheld the principle of
Tribal consultation, whereby the federal government consults with tribes on federal actions, policies, rules
or regulations that will directly affect them.
Recommended Approach
Literature and historical experiences support the conclusion that effective and representative governance
is more important than the specific technology platforms selected.
● Governance must be effective and efficient
● The governing body for a project of this complexity must remain small to balance effective and
efficient decision making and the need to be representative of a diverse collection of stakeholders
● Establish a multi-member governing body that interacts regularly with stakeholder groups, both
formally through Tribal Consultation policies and informally through leadership and subject
matter expert (SME) stakeholder user groups
○ The stakeholder groups should be inclusive to effectively represent the inherent diversity
of the ecosystem
10
○ Substantial clinical engagement must be continuous throughout the project
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
12
Technology
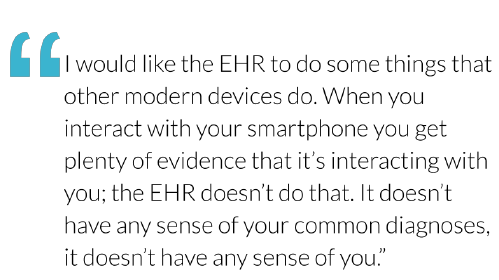
Engage End Users to Understand Their Needs
End users should be engaged in all steps of the modernization process to ensure
that their needs are met by the modernized system.
The Challenge
In the early stages of the existing HIT system, informal collaborative decision-making at the local level
allowed for easy customization to reflect Tribal culture and values. This permitted Tribal health
organizations to take ownership of their HIT configuration and ensure that it could be agile enough to
resolve needs as they came up.
16
However, long-standing underfunding of HIT within IHS coupled with a
series of mandates that were unsupported by recurring
funding (Meaningful Use and the ICD-10 transition,
for example),
17
has hindered the ability of IHS Office
of Information Technology (OIT) to keep pace with
the industry-wide explosion in HIT capabilities as well
as user needs.
End users are generally dissatisfied with the existing
HIT system, with 60% of Data Call respondents
believing that the system needs significant
improvements.
12
The current user experience (UX) is
disjointed across several applications; moreover, current user experience design (UXD) leads to frustration
and an increased risk of user error.
11, 18
The existing HIT system also has limited functionality across several areas of care, including, but not
limited to, obstetrics, behavioral health, emergency medicine, pharmacy, radiology, dental, women’s
health, laboratory, and pediatrics.
11
“Our health system currently includes Medical, Pediatrics, Visiting Nurses, Hep C Treatment
team, Mental Health, Chemical Dependency, Suboxone treatment, and Dental. RPMS cannot meet
the demands of all of these separate services.”
11
While training for the existing HIT system does exist, availability is scarce and occasionally too technical.
Users report that it is difficult to apply what they learn in training to their workflow. With limitations in
regular, formal training, staff often rely on their co-workers for direction and troubleshooting, which can
lead to incomplete information.
11
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
13
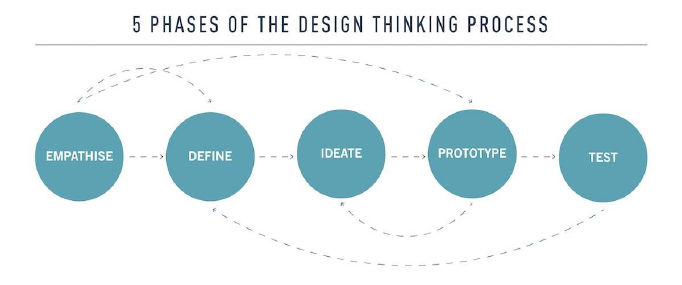
Recommended Approach
In order to efficiently manage programs, maximize revenue generation, and provide high-quality care for
patients, staff must have access to a comprehensive HIT system that seamlessly integrates into and
enhances their workflow.
● In the near term, use human-centered design practices and tools to foster facility-level listening
and ideation sessions with the goal of obtaining a better understanding of HIT best practices and
challenges across roles. Leverage existing models created by the Modernization Project, Centers
for Medicare and Medicaid Services (CMS), or the United States Digital Service (USDS) to
create event-in-a-box-style tools for sites
● Follow the design thinking model
18
when designing and implementing a new HIT system
● Use the data collected by the Modernization Project as the foundation for a list of user-identified
system requirements
● Provide resources, both human and financial, to continuously evaluate and evolve the system as
new technology and processes become available
● Aim to establish software configuration consistency when appropriate and customization when
essential
● Engage usability experts who understand the unique needs of the I/T/U network during the design
process
● Develop, adopt, and increase availability of user-centric training and support
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
14
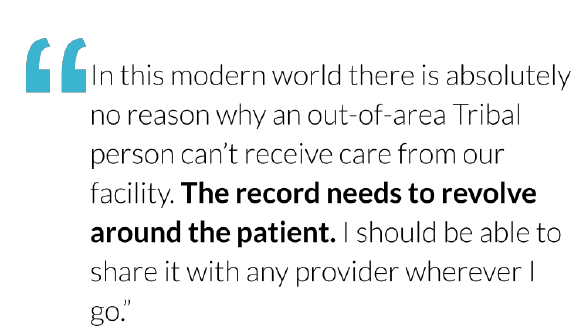
Provide Full Support for Data Exchange and Interoperability
Between IHS Systems and Components
Interoperability should be implemented across all IHS HIT facilities to provide
seamless data exchange and communication, ensuring comprehensive patient care.
The Challenge
Currently, the paucity of data sharing across IHS impacts patient care. Improving data sharing would reap
numerous patient benefits. Interoperability, or the ability for different systems and applications to
seamlessly exchange data, is essential to supporting comprehensive care. Interoperability and data sharing
improves care coordination and patient experiences, supports greater patient safety, privacy, and security,
and increases productivity.
The following technology gaps were
identified during the course of the
Modernization Project:
● Limited continuity of care within a
facility -- Manual transferal of
information between applications
is burdensome, error-prone, and
time-consuming
● Little automatic data capture from
biomedical equipment -- Data
generated from biomedical
equipment should be incorporated directly into the HIT system without the need for additional
data entry. Smart machines, such as thermometers, electronic blood pressure instruments, heart
monitors, glucometers, scales, EKG machines, and fetal monitoring equipment are available at
some sites, but in many cases the data must be entered into the system manually, which requires
additional time and increases the risk of data entry error and an absence of critical data at the
point of care
● Limited continuity of care between facilities/organizations -- Interoperability is critical for the
creation of a longitudinal health record that can be used to provide and improve care. There
currently is reliance on a patient’s self-reporting in the absence of interoperability. In an
environment where it is not uncommon for services for a single patient to be seek care at several
sites,
20
the necessity for inter-facility information exchange is paramount

⠠⠠⠠⠠HHS/IHS HIT Modernization Project
15
Recommended Approach
The following steps are recommended to move toward system data sharing and interoperability.
● Establish a roadmap that commits to a health information exchange that can provide a patient’s
longitudinal record across facilities. To be successful, the enterprise model and the heterogeneity
of the I/T/U system mandates evaluation of current models and the development of a
comprehensive action plan to meet this goal
● Establish governance for evaluation of HIT systems to have processes and policies that ensure
that systems developed or purchased support interoperability including current and future data
and messaging standards and open application program interfaces (APIs)
● Ensure that historical data is available and integrated into future solutions
● Provide continuous evaluation and modification of processes to help ensure consistency in data
quality, including data collection and data entry
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
16
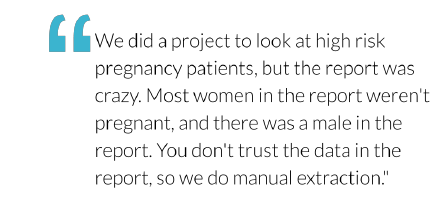
Improve Analytics and Business Intelligence
Analytics and business intelligence functionalities must be integrated into the
modernization process to provide quality public and population patient healthcare.
The Challenge
During the course of the Modernization Project, users commonly expressed frustration with the limited
ability to access the data or reports they needed, even though the existing HIT system offers the ability to
do so. It is important for clinicians, clinician leaders, and other managers at I/T/U facilities to have the
ability to initiate queries and conduct analytics. There is a
clear need and opportunity for improvement in the area of
analytics and business intelligence as IHS pursues HIT
modernization.
The generation of analytics in the existing HIT system has
significant issues and deficiencies. Reporting capabilities
are distributed across a wide range of applications and most
reports and queries can only be executed via menu-driven
character interfaces, even if the source applications are graphical. Institutional knowledge about the
reporting capabilities of the existing HIT system is waning, and available training is not accessed by or
targeted at those who would gain most value by knowledge of these features.
Recommended Approach
To ensuring successful continuation and evolution of facility-level analytics and business intelligence over
the course of the HIT modernization effort, the following recommendations are presented:
● Conduct a user-centered gap analysis to identify current barriers and needs for clinical and
administrative staff to conduct near real-time queries, both preconfigured and ad hoc, on locally
served patients and populations
● Determine the best approach to address the user needs
● Determine the appropriate topology and architecture for the systems supporting analytics, whether
it be locally- or centrally-deployed
● Ensure alignment with the overall HIT modernization goals to improve the systems supporting
direct care and public health, as well as the analytics needs of the agency
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
17
Modernize the IHS HIT Infrastructure
The IHS HIT Infrastructure must be updated to meet the healthcare delivery needs
through appropriate and adequate bandwidth, network, communications, hardware,
support, and training.
The Challenge
While the existing HIT system runs well within the capabilities of commodity servers, client hardware at
the local facilities is often under-provisioned and antiquated. Existing network infrastructure, software
maintenance, and database development and support are deemed inadequate. Limited support for system
maintenance and patches disrupts patient care and workflows. Sites are constrained by limited support
personnel. Some sites have custom modifications to support their needs, presenting a challenge to
receiving updates and potentially creating security issues. A modern HIT infrastructure is essential for the
future.
Recommended Approach
The following activities to achieve infrastructure modernization are recommended:
● Address technological infrastructure concerns and work with consultant groups for modernization
guidance
● Select the fewest possible technology suites to minimize integration and maintenance challenges
and maximize end-user satisfaction, focusing on three primary areas: patient safety, fundamental
operational functions, and cybersecurity
● Restructure the organization, guided by organizational change management (OCM) initiatives, to
facilitate IHS HIT infrastructure modernization
● If a commercially available off the shelf (COTS) solution is adopted, the IHS must sustain
responsibility for VA-sourced applications or contract for continued maintenance of these
applications with VistA-based companies until they are sunset
21
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
18
Begin HIT modernization with the following steps to allow time for training, evaluation, and adoption and
implementation of change processes:
● Establish a Program Management Office (PMO) to develop and oversee an implementation
strategy
● Develop and implement appropriate governance to ensure decisions are made jointly with clinical
and technical input
● Involve end users to ensure that critical requirements, such as the migration of historical data to
the new platform, are included in planning
● Establish a consistent software development life cycle including implementation and deployment
with the engagement of leadership and clinical personnel to foster transparency
● Complete an in-depth assessment and roadmap to address technical and infrastructure
requirements and develop an organizational readiness framework
● Review and modify the proposed roadmap to include a sustainability model and the use of
stabilization teams to ensure user needs are understood and prioritized appropriately
● Stabilize and consolidate current HIT infrastructure and processes
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
19
Strengthen IHS HIT Security and Compliance
The HIT ecosystem must be continuously assessed and updated to meet security and
privacy compliance.
The Challenge
As the healthcare industry increasingly adopts technology and embraces public cloud infrastructure as core
capabilities and competitive differentiators in delivery of healthcare services, the associated cybersecurity
risks proportionally increase. Innovations in healthcare technology usher in significant value to patients
along with cost-efficiencies and economies of scale to service providers. However, healthcare services
delivered electronically leave facilities vulnerable to cyber-attacks. These risks exponentially increase in
distributed, interconnected healthcare systems through which large volumes of healthcare data and
information are exchanged among disparate organizations.
Recommended Approach
The following steps, tasks, and activities will help to strengthen IHS’ HIT security and compliance posture
to enable the organization to detect and identify security risks in order to protect its HIT ecosystem, and
where necessary, respond to and recover from such attacks:
● Augment, implement, and document a framework for ongoing security evaluation and potential
remediation of the HIT system
● Utilize real-time security monitoring, application event logging, and security performance metrics
to continuously assess and improve HIT security practices
● Leverage other organizations to help identify and evaluate options for lightweight and appropriate
data governance and privacy practices
● Continue to support authentication and the principle of least privilege (PoLP) authorization in
application design, architecture, and implementation
● Integrate incorporation of security testing throughout the software development lifecycle (SDLC)
as well as quality assurance (QA) and quality control (QC) processes
● Continue to ensure compliance with existing and future cybersecurity standards and federal data
security and privacy regulations
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
20
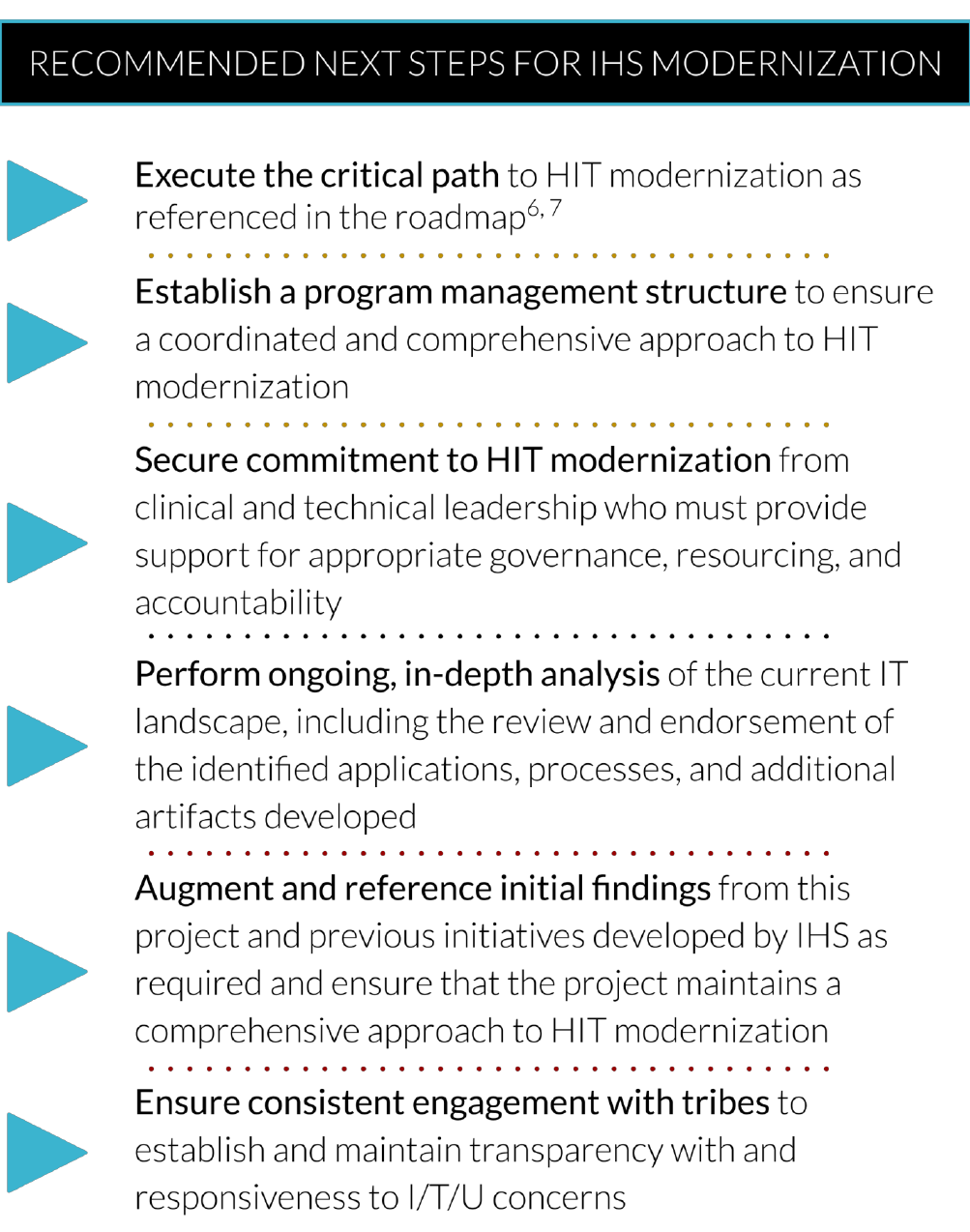
Next Steps
The IHS HIT Modernization Project was designed to identify and frame the initial critical path required to
achieve success; however, the proposed modernization program requires an immediate and long-term
commitment. This work is a launching point for IHS HIT modernization requiring active engagement,
iteration, and support to achieve the vision of HIT modernization within IHS. The recommendations in this
work provide guidance for subsets of subsequent actions. The roadmap provides a more detailed critical
path to HIT modernization.
6, 7
Establishing a program management structure, as well as ownership by an organizational entity, is an
essential next step. The organization should be responsible for the oversight and execution of a roadmap,
ensuring a coordinated and comprehensive approach to HIT modernization. The roadmap developed for
this project provides the initial substrate for the next phase of HIT modernization. Broad-based clinical and
technical leadership commitment is essential to the implementation and success of this endeavor.
Leadership must fully understand and establish a long-term commitment to the HIT modernization
program through engagement and support for appropriate governance, resourcing, and accountability.
Additional understanding and in-depth analysis of the existing IT landscape beyond the current project
artifacts are required, including the review and endorsement of the identified applications, processes, and
artifacts developed. While this project provides a comprehensive review of the HIT components, there is a
need for additional evaluation and endorsement of key findings by IHS.
The roadmap also includes multiple improvement opportunities identified through the human centered
design discovery process. Nine strategies and 18 work initiatives were identified that are reflective of the
recommendations in this final report. However, the overarching discovery process was not exhaustive.
Additional iterative evaluation and work is required to augment these initial findings and ensure that the
project maintains a comprehensive approach to this work.
The recommendations, coupled with the roadmap, provide an actionable path forward for HIT
modernization within IHS. The collaboration between tribes and federal agencies can show that innovative
and appropriate technology, along with streamlined policies and well-designed support, can advance
population health and patient-centered care for health systems nationwide. This contributes to the
improved health status and health outcomes for populations that remain at risk. Consistent engagement
with tribes and transparency and responsiveness to I/T/U concerns are integral components to the HIT
modernization enterprise initiative within IHS. The modernization effort belongs to tribes as well as to
HHS/IHS.
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
21
References
1. Indian Health Service. About IHS [Internet]. Rockville (MD): Indian Health Service; 2003 Mar 18
[cited 2019 Jul 22]. Available from: https://www.ihs.gov/aboutihs/.
2. Indian Health Service. About Us OIT [Internet]. Rockville (MD): Indian Health Services; [cited
2019 Aug 27]. Available from: https://www.ihs.gov/oit/aboutus/.
3. Ray K, Biondich P, Flowers J, Thomas J. IHS HIT communities of practice: modernizing methods
of peer support to enhance health information use. White Paper [Internet]. Indianapolis (IN):
Regenstrief Institute; 2019 July. 22 p. Supported by the U.S. Department of Health and Human
Services (HHS) Office of the Chief Technology Officer (CTO).
4. Capability Maturity Model Team Members. Strategic options for the modernization of the Indian
Health Service electronic health record: Capability Maturity Model [Internet]. Indianapolis (IN):
Regenstrief Institute; 2019 Aug 30. 20 p. Supported by the U.S. Department of Health and Human
Services (HHS) Office of the Chief Technology Officer (CTO).
5. Capability Maturity Model Team Members. Strategic options for the modernization of the Indian
Health Service electronic health record: Capability Maturity Model. Final Report [Internet].
Indianapolis (IN): Regenstrief Institute; 2019 Aug 30. 20 p. Supported by the U.S. Department of
Health and Human Services (HHS) Office of the Chief Technology Officer (CTO).
6. ERP Strategy Roadmap Tool [Internet]. London (ON): Info Tech Research Group; [cited 2019
June 25].
7. Roadmap Team Members Strategic options for the modernization of the Indian Health Service
electronic health record: Roadmap. Final Report [Internet]. Indianapolis (IN): Regenstrief
Institute; 2019 Aug 28. 15p. Supported by the U.S. Department of Health and Human Services
(HHS) Office of the Chief Technology Officer (CTO).
8. Seminole Nation v. United States (1942) 316 US. 286, 297.
9. About HHS [Internet]. Washington (DC): Health and Human Services; 2019 [cited 2019 Aug 20].
Available from: https://www.hhs.gov/about/index.html.
10. Technical Advisory Commission Members. Strategic options for the modernization of the Indian
Health Service electronic health record: TAC. Final Report [Internet]. Indianapolis (IN):
Regenstrief Institute; 2019 Aug 18. 23 p. Supported by the U.S. Department of Health and Human
Services (HHS) Office of the Chief Technology Officer (CTO).
11. Site Visits and Qualitative Data Team Members. Strategic options for the modernization of the
Indian Health Service electronic health record: Qualitative Data. Final Report [Internet].
Indianapolis (IN): Regenstrief Institute; 2019 Aug 21. 61 p. Supported by the U.S. Department of
Health and Human Services (HHS) Office of the Chief Technology Officer (CTO).
12. Data Call Team Members. Strategic options for the modernization of the Indian Health Service
electronic health record: Data Call. Final Report [Internet]. Indianapolis (IN): Regenstrief Institute;
2019 May 2. 26 p. Supported by the U.S. Department of Health and Human Services (HHS) Office
of the Chief Technology Officer (CTO).
13. User- identified Data Call Team Members. Strategic options for the modernization of the Indian
Health Service electronic health record: User-Identified Priorities Data Call. Final Report
[Internet]. Indianapolis (IN): Regenstrief Institute; 2019 Sept 12. 13 p. Supported by the U.S.
14. Indian Self-Determination and Education Assistance Act (2005 Jan 03) 25 UCS. 450. Available
from: https://www.usbr.gov/native/docs/25USC450.pdf.
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
22
15. Indian Self-Determination Act Amendments of 1994 (1994 July 27) Public Law No: 103-413.
Available from: https://www.congress.gov/bill/103rd-congress/house-bill/4842.
16. Literature Review/ Modernization Interview Team Members. Strategic options for the
modernization of the Indian Health Service electronic health record: Literature Review and
Modernization Interviews. Final Report [Internet]. Indianapolis (IN): Regenstrief Institute; 2019
Aug 19. 50 p. Supported by the U.S. Department of Health and Human Services (HHS) Office of
the Chief Technology Officer (CTO).
17. Bert JM, Beach WR, McIntyre LF, Sachdev R. Getting Ready for ICD 10 and Meaningful Use
Stage 2 [Internet]. Woodbury (MN): PubMed US National Library of Medicine National Institutes
of Health; [cited 2019 Aug 28]. Available from: https://www.ncbi.nlm.nih.gov/pubmed/27049227.
18. Legacy Assessment Team Members. Strategic options for the modernization of the Indian Health
Service electronic health record: Legacy Assessment. Final Report [Internet[. Indianapolis (IN):
Regenstrief Institute; 2019 May 14. 187 p. Supported by the U.S. Department of Health and
Human Services (HHS) Office of the Chief Technology Officer (CTO).
19. Design Thinking: What is design thinking? [Internet]. Aarhus (Denmark): Interaction Design
Foundation; 2009 [cited 2019 Aug 28]. Available from:
https://www.google.com/url?q=https://www.interaction-design.org/literature/topics/design-
thinking&sa=D&ust=1567018098073000&usg=AFQjCNEi9sEkxW5tunIB31mpW9WRTJEbmg/.
20. Norris T, Vines PL, Hoeffel E. The American Indian and Alaska Native Population: 2010
[Internet]. Suitland (MD): U.S. Department of Commerce Economics and Statistics
Administration U.S. Census Bureau; 2012 Jan [updated 2012 Mar 2, cited 2019 July 7]. 21p.
Report No.: C2010BR-10. Available from: https://www.census.gov/prod/cen2010/briefs/c2010br-
10.pdf.
21. Analysis of Alternatives Team Members. Strategic options for the modernization of the Indian
Health Service electronic health record: Analysis of Alternatives. Final Report [Internet].
Indianapolis (IN): Regenstrief Institute; 2019 June 6. 97 p. Supported by the U.S. Department of
Health and Human Services (HHS) Office of the Chief Technology Officer (CTO).
⠠⠠⠠⠠HHS/IHS HIT Modernization Project
23
Appendix A: Constraints and Mitigations to the HIT Modernization
Effort
The following constraints and mitigations were identified during the IHS HIT Modernization Project.
Constraints
Proposed Mitigations
Critical and unique system
capabilities currently
implemented in RPMS must
be persisted to the replacement
HIT solution or ecosystem
IHS must provide HIT systems that are attractive to Tribal and urban programs
through support for integrated, multidisciplinary care (behavioral health, dental,
etc.) as well as population health and individual patient care. Requirements and
resultant capabilities and functionality related to traditional medicine, AI/AN
population health, etc. must persist in the replacement HIT solution.
Funding and staffing levels
Noted as a foregoing operational issue but not assessed in detail; as such, this
report assumes that funding to improve infrastructure, to recruit, train, and
retain local and national support staff, and to address development and
implementation costs for new or updated systems will be available.
Organizational readiness for
change
Through an enterprise-wide organizational change management initiative, IHS
shall plan and execute the required strategic and operational changes required
for success of the Modernization program.
Site-specific infrastructure
constraints related to limited
bandwidth, poor cellular
signal, degraded or inadequate
telephony and wide area
network (WAN)
infrastructure, etc.
As a primary and critical initial step in IHS HIT Modernization program, IHS
must conduct a comprehensive infrastructure analysis and subsequent
infrastructure build-out to remediate critical infrastructure deficiencies.
Moreover, infrastructure constraints that are too costly to mitigate will
proactively inform and influence the selection, architecture, design, and
topology of the new HIT solution in order to achieve cost-efficiencies and
optimal system quality.
Security, confidentiality,
patient privacy
Through ongoing and augmented security practices, IHS shall identify, validate,
and prioritize external and internal security vulnerabilities and threats through a
security risk assessment (SRA). The results of this assessment will lead to
needed improvements in data security, confidentiality, and privacy, thereby
driving increased compliance and patient satisfaction.

⠠⠠⠠⠠HHS/IHS HIT Modernization Project
24
Interoperability requirements
The replacement HIT solution or ecosystem must be intrinsically
interoperable and must support data sharing, both within and external to the
I/T/U. The following recommendations will assist in meeting interoperability
goals:
● Conduct a gap analysis to identify and prioritize interoperability
deficiencies in IHS' HIT ecosystem
● Define IHS' interoperability strategy and communicate it broadly to
stakeholders
● Ensure interoperability needs are surfaced through the Requirements
Management (RM) and Enterprise Architecture (EA) artifacts
● Partner with the Acquisition Planning and Procurement (AP&P) office
to integrate interoperability needs into acquisition planning
● Adhere to open standards in the design and implementation of
interoperable systems
● Ensure strict security and privacy of data and information shared
across interoperable systems to drive wide-scale adoption
● Utilize efficient, cost-effective infrastructure to achieve
interoperability across distributed and external systems
● Implement unintrusive, value-added data governance practices
Regulatory compliance
Through an improved requirements management process, value-oriented
lightweight enterprise architecture (EA) practice, and outcome-driven
governance, the replacement HIT solution or ecosystem will need to meet or
exceed regulatory requirements, including the Office of the National
Coordinator for Health Information Technology (ONC) and the Centers for
Medicare and Medicaid (CMS) certification requirements and other
regulatory constraints, such as Clinical Laboratory Improvement
Amendments (CLIA).
Support for legacy
systems/subsystems/
components
Any approach that retains legacy systems/subsystems/components must plan
for ongoing operations and maintenance (O&M) or replacement of VistA-
derived packages. Moreover, there are associated cost and resource
implications as well as related risks.
