
Office of the
National
Coordinator
for Health
Information
Technology
(ONC)
Federal Health
Information
Technology
Strategic Plan
2011 – 2015
Table of
Contents
Introduction 3
Federal Health IT Vision and Mission 6
Federal Health IT Principles 7
Goal I: Achieve Adoption and Information Exchange through
Meaningful Use of Health IT 8
Goal II: Improve Care, Improve Population Health, and Reduce
Health Care Costs through the Use of Health IT 21
Goal III: Inspire Confidence and Trust in Health IT 28
Goal IV: Empower Individuals with Health IT to Improve their
Health and the Health Care System 36
Goal V: Achieve Rapid Learning and Technological Advancement 43
Appendix A: Performance Measures 49
Appendix B: Programs, Initiatives, and Federal Engagement 51
Appendix C: HIT Standards and HIT Policy Committees
Information Flow 65
Appendix E: Statutes and Regulations 67
Appendix F: Goals, Objectives, and Strategies 70
Appendix G: Acronyms 74
ONC 77
Acknowledgements 77
Notes 78

Federal Health IT Strategic Plan 3
Federal Health IT Strategic Plan 4
Introduction
he technologies collectively known as health
information technology (health IT) share a
common attribute: they enable the secure
collection and exchange of vast amounts of
health data about individuals. The collection and
movement of this data will power the health care of
the future. Health IT has the potential to empower
individuals and increase transparency; enhance the
ability to study care delivery and payment systems;
and ultimately achieve improvements in care,
efficiency, and population health.
However, these technologies – including electronic
health records (EHRs), personal health records
(PHRs), telehealth devices, remote monitoring
technologies, and mobile health applications – are
remarkably underutilized today. In 2010, only 25
percent of physician offices and 15 percent of acute
care hospitals took advantage of EHRs.
i
Even fewer
used remote monitoring and telehealth technologies.
While many consumers access their banking
information online daily, only 7 percent have used
the web to access their personal health information.
ii
Recent legislation has established an agenda and
committed significant resources for health IT. The
Health Information Technology for Economic and
Clinical Health (HITECH) Act, passed as part of the
American Recovery and Reinvestment Act of 2009,
allocated billions of dollars for the health care system
to adopt and meaningfully use health IT to improve
health. The Patient Protection and Affordable Care
Act of 2010, as amended by the Health Care and
Education Reconciliation Act of 2010, (referred to
collectively as the Affordable Care Act) builds on the
HITECH Act and recognizes health IT as a critical
enabler to broad transformations in health care. This
document is the Federal Health IT Strategic Plan,
developed under the leadership of the Office of the
National Coordinator for Health Information
Technology (ONC) and in close collaboration with
other federal partners, for working with the private
and public sectors to realize Congress and the
Administration’s health IT agenda.
The first Federal Health IT Strategic Plan was
published in June 2008. Section 3001(c)(3) of the
Public Health Service Act, as added by the HITECH
Act, requires the National Coordinator to update
and republish the Plan. This Plan updates the
previous version to take into account the rapidly
changing landscape of health IT and health IT
policy. In order to update the Plan, ONC leveraged
the strategic framework put forth by the HIT Policy
Committee and obtained additional input by
conducting interviews with representatives from
federal agencies/offices and the private sector.
ONC also engaged its federal partners, the private
sector and members of the public to provide
comments on multiple versions of the Plan.
Goal I, “Achieve Adoption and Information
Exchange through Meaningful Use of Health IT”
discusses the centerpiece of the government’s health
IT strategy over the next five years. “Meaningful
use” is aimed at widespread adoption and
information exchange in its first two stages, and will
then build to improve health outcomes in the third
stage. Activities are focused on two areas: defining
the meaningful use of certified EHR technology; and
encouraging the achievement of meaningful use
through the CMS administered Medicare and
Medicaid EHR Incentive Programs and the support
of meaningful use through grant programs, including
information exchange with public health
departments and laboratories.
Goal II, “Improve Care, Improve Population Health,
and Reduce Health Care Costs through the Use of
Health IT,” discusses the specific ways health IT is
contributing to the goals of health care reform:
improved care, improved population health, and
reduced per capita costs of health care. Widespread
adoption of EHRs, information exchange, quality
improvement initiatives, and health care reform
pilots are required to implement the Affordable Care
Act. As part of each of these activities, the
government is investing in and leveraging health IT
to transform the health care system.
Goal III, “Inspire Confidence and Trust in Health
IT,” focuses on government efforts to update its
approach to privacy and security issues related to
health IT, and build greater confidence and trust in
T
Federal Health IT Strategic Plan 5
EHRs and health information exchange among
providers and the public. The digitization of health
records will create a new set of challenges for
protecting the privacy and security of health
information, but it will also open new opportunities
for improving safeguards.
Goal IV, “Empower Individuals with Health IT to
Improve their Health and the Health Care System,”
discusses how the government is designing health IT
policies and programs to meet individual needs and
expectations, provide individuals with access to their
information, help facilitate a strong consumer health
IT market, and better integrate individuals’ and
clinicians’ communications through health IT. A
public that has a voice in designing national health
IT policies and programs and is empowered with
access to its health information through useful tools
can be a powerful driver in moving toward patient-
centered health care.
Goal V, “Achieve Rapid Learning and Technological
Advancement,” focuses on demonstrating ways
health IT and meaningful use can enable innovation
and appropriate use of health information to
improve knowledge about health care across
populations. In the long run, the government is
pursuing a vision of a learning health system, in
which a vast array of health care data can be
appropriately aggregated, analyzed, and leveraged
using real-time algorithms and functions.
iii
ONC will track national progress towards achieving
the goals laid out in this Plan. Ongoing
collaboration with federal agencies, states and
providers will be necessary in order to realize these
goals. The Plan is meant to be a living document
that will be updated based on experience with stage
one meaningful use and the implementation of a
robust evaluation program.
This
future will require technical innovation to build on
the foundation of meaningful use, as well as finding
new ways to use that foundation in the practice of
health care.
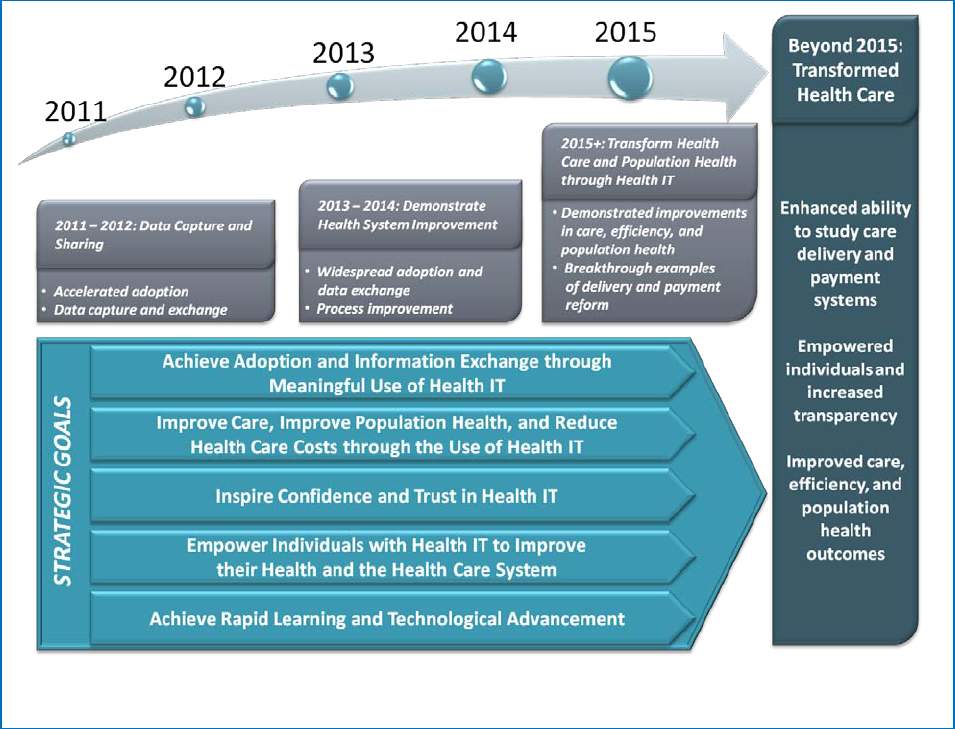
Figure 1; Federal Health IT Strategy Map
Federal Health IT Strategic Plan 6
Federal Health IT Vision and Mission
Vision
A health system that uses information to empower individuals and
to improve the health of the population.
Mission
To improve health and health care for all Americans through the
use of information and technology
.
Federal Health IT Strategic Plan 7
Federal Health IT Principles
In developing and executing the federal health IT strategy, the government strives to
Put individuals and their interests first. In order to enhance the health and well-being of all Americans, the
government must meet the needs and protect the rights of each individual.
Be a worthy steward of the country’s money and trust. The government seeks to use its resources
judiciously. This means relying to the extent possible on private markets to accomplish important societal
objectives, and acting to correct market failures when necessary. It also means developing governmental policies
through open and transparent processes.
Support health IT benefits for all. All Americans should have equal access to quality health care. This includes
the benefits conferred by health IT. The government will endeavor to assure that underserved and at-risk
individuals enjoy these benefits to the same extent as all other citizens.
Focus on outcomes. Federal health IT policy will constantly focus on improving the outcomes of care, so as to
advance the health of Americans and the performance of their health care system.
Build boldly on what works. The government will set ambitious goals and then work methodically to achieve
them, monitoring health IT successes, and looking for ways to expand upon programs that work. It will seek to
be nimble and action-oriented: evaluating existing government activities, learning from experience, and changing
course if necessary.
Encourage innovation. The government is working to create an environment of testing, learning, and
improving, thereby fostering breakthroughs that quickly and radically transform health care. The government
will support innovation in health IT.
Federal Health IT Strategic Plan 8
Goal I: Achieve Adoption and Information Exchange
through Meaningful Use of Health IT
he first priority in realizing the benefits of
health IT is to achieve nationwide adoption
of EHRs and widespread information
exchange. As patients and providers
experience the benefits of EHRs, they will demand
nothing less from their health care practices. The
Medicare and Medicaid EHR Incentive Programs
accelerate the realization of this future by offering
financial incentives to hundreds of thousands of
eligible professionals, eligible hospitals and critical
access hospitals for incorporating certified EHR
technology into their practices. “Meaningful use” is
much more than just adoption – these providers will
also be required to maintain data confidentiality,
share information securely with each other, engage
patients with their electronic health information, and
improve care.
There are a few well-defined barriers that have
slowed acceptance of EHRs and widespread
information exchange. Small- and medium-sized
providers often do not have sufficient capital to
implement EHR systems. There is a lack of skilled
health IT professionals to support providers as they
transition from paper records to EHRs. Using EHRs
may alter current provider workflows, and many
providers struggle to select systems, use them in
ways that will improve care, and make the necessary
changes to their processes. Finally, information
exchange, which is central to realizing the benefits of
EHRs, is not fully possible today – there is no
interoperable infrastructure to securely exchange
health information nationwide among providers,
between providers and patients, and between
providers and public health agencies (see Objectives
I.B and I.C).
Through the HITECH Act, the Department of
Health and Human Services (HHS) created a set of
far-reaching programs to help providers overcome
such barriers. For the Medicare and Medicaid EHR
Incentive Programs, the three progressive stages of
meaningful use will define what eligible professionals
and hospitals can and should accomplish through
the adoption and use of EHRs over the next five
years. Stage one objectives focus on adopting EHRs
and beginning to take advantage of basic electronic
data capture, medication ordering, and decision-
support tools. We expect future stages to become
more rigorous, for example, by requiring providers
not only to adopt the technology but to use it to
exchange health information and – ultimately – to
achieve improvements in care, efficiency, and
population health (see Goal II). We anticipate that
future stages of meaningful use will be aligned to
support advancing nationwide-wide health goals, as
defined in the HHS Strategic Plan, and the priority
areas identified in the National Quality Strategy.
In addition to incentive payments, the HITECH Act
programs provide significant support for providers
to achieve adoption and meaningful use, including
implementation support, workforce training, and
information exchange support. Programs are
focused on the providers that need the most help –
solo and small group practices, community health
centers, critical access hospitals, and providers
located in rural and underserved areas. In 2010, HHS
issued rules establishing the requirements of the
first stage of meaningful use. HHS expects to
articulate two further stages through rulemaking
over the next five years. Participation in the
Medicare and Medicaid EHR Incentive Programs is
voluntary, but beginning in 2015, eligible
professionals and hospitals under the Medicare EHR
Incentive Programs will face payment reductions if
they do not meet the meaningful use requirements.
In implementing the Medicare and Medicaid EHR
Incentive Programs, the government is taking
advantage of the experience of federal agencies that
deliver health care (Department of Veterans Affairs,
Department of Defense, and Indian Health Service)
that have already-developed EHR systems which
have been in place for over a decade. These agencies’
experiences in using EHRs can offer important
insights and best practices for the nationwide
adoption of EHRs.
T
Federal Health IT Strategic Plan 9
It is the government’s goal that such a large-scale
movement will create a tipping point – that the
adoption and meaningful use of EHRs will become
ubiquitous across the nation. To this end, the
government is seeking to encourage meaningful use
through other mechanisms in addition to HITECH
Act programs. This includes supporting the above-
mentioned federal agencies that deliver health care and
federal grant recipients (critical access hospitals,
community health centers, etc.) in meeting meaningful
use requirements. We expect that medical societies and
professional licensing and certifying bodies will also
help to encourage meaningful use among their
members. Some private insurers are already mirroring
the Medicare and Medicaid EHR Incentive Programs
and providing incentives for the achievement of
meaningful use among their provider communities. For
providers ineligible for incentive payments under the
Medicare and Medicaid EHR Incentive Programs (for
example, long-term and post-acute care facilities,
community mental health centers, and some behavioral
health providers), the government is developing
technology and policy solutions that will build on the
Department’s meaningful use efforts and fit their
unique needs (see Strategy I.C.3).
The government’s objectives to “Achieve Adoption
and Information Exchange through Meaningful Use
of Health IT” are:
A. Accelerate adoption of electronic health
records
B. Facilitate information exchange to support
meaningful use of electronic health records
C. Support health IT adoption and
information exchange for public health and
populations with unique needs
Spotlight on Health Outcomes
Use of health IT can improve health outcomes and enhance care coordination
These “Spotlight on Health Outcomes” are intended to highlight exemplary ways that widespread adoption and use of health IT and electronic health
information exchange could help transform and improve health care. Some of these examples are only aspirational today or only exist in select communities
or health systems. However, these examples illustrate the type of transformed health care that could be possible with the achievement of the goals of this Plan.
George is a 62-year-old man with diabetes, hypertension, and heart failure
who smokes one pack of cigarettes every day. George’s primary care provider
(PCP) is reviewing an EHR-generated listing of patients with an HbA1c test
result over 9. She notices that George is on her list with an HbA1c of 11.2
and that he missed his last appointment and has not yet rescheduled.
George’s PCP emails him via secure messaging to request he make an
appointment and get the following tests in advance of the visit: HbA1c and
cholesterol panel. She orders these tests via computerized provider order
entry (CPOE). George goes online to schedule his appointment. Prior to his
appointment, George’s PCP checks his lab results which are sent
electronically to the EHR and sees that his HbA1c and cholesterol are still
elevated. A nurse uses clinical decision support to determine that George
would benefit from diabetes self-management and smoking cessation
counseling, which she gives before his appointment. During his appointment,
George’s PCP talks to him about adding a new medication to better control
his diabetes and increasing the dose of his cholesterol medicine. She sends
the new prescriptions electronically to George’s pharmacy so that they will be
ready for pick-up when he leaves the office visit. Clinical decision support
also reminds the PCP that George is due for eye and foot exams. She
performs a foot exam and sends an electronic referral to the
ophthalmologist’s office, who will contact George via secure messaging to
schedule an appointment. The ophthalmologist has access to George’s record
and can input data and recommendations that are viewable by his PCP, thus
creating a “seamless care” model. To help him with his multiple conditions,
George is set up with a case manager who will work with George to develop
strategies to quit smoking and eat healthier/exercise more. The case manager
has access to the full EHR and can communicate directly with the rest of the
team to update them on George’s progress.
Jane is an 83-year-old woman with COPD,
hypertension, and peripheral vascular disease
who is admitted to the hospital with
pneumonia. As the admitting physician is
ordering an antibiotic for pneumonia, a
drug-allergy warning pops up on the screen
alerting the physician that Jane had an
anaphylactic reaction to penicillin in the past
and another antibiotic is preferred – saving
Jane from an adverse drug event. Jane is at
high-risk for developing a clot in her legs,
which can lead to a pulmonary embolism. As
part of the admissions order set, the
physician is prompted to choose a type of
prophylaxis for clots, which reduces her risk
of developing this complication and a
prolonged hospital stay. The nurse who
admits Jane notices a small decubitus ulcer
present on admission. She documents the
ulcer on her mobile device and monitors and
treats it with the aid of clinical decision
support

Federal Health IT Strategic Plan 10
OBJECTIVE A
Accelerate adopt
ion of electronic
health records
Strategy I.A.1: Provide financial incentive
payments for the adoption and meaningful
use of certified EHR technology.
Central to the HITECH Act is the establishment of
the Medicare and Medicaid EHR Incentive
Programs, which makes available incentive payments
that could total an estimated $27 billion over 10
years, to encourage eligible professionals and
hospitals to adopt and meaningfully use certified
EHR technology.
iv
Recording patient information into EHRs, such as
gender, race, preferred language, height, weight,
smoking status, and blood pressure
The programs generally require
providers to do the following:adopt EHRs that are
certified according to standards, implementation
specifications, and certification criteria adopted by
the Secretary, and meet certain objectives and
measures using certified EHR technology established
for progressive stages of meaningful use as defined
in CMS rules. CMS’ final rule for stage one
meaningful use was published in July 2010. Stage
one meaningful use objectives include:
Using a software application to inform clinical
decisions
Entering medical prescriptions electronically
Providing patients with a timely electronic copy of
their health information
Securing EHRs to protect the privacy of patient
data
Future stages of meaningful use are likely to include
a combination of new objectives, some of which
may require new EHR functionality, changes to
existing objectives, such as an increase in the
threshold or broadening of the definition. In the
future stages of the Medicare and Medicaid EHR
Incentive Programs, the government expects to
reward improvement against predetermined
thresholds that are associated with the adoption and
use of EHRs. Stages two and three are anticipated to
transition gradually away from further process
requirements like those included in stage one, to
requirements for improvement in outcomes and
quality of care. Any such improvement measures will
be in line with nationwide health goals as laid out in
the HHS Strategic Plan and with the national
priorities identified in the National Quality Strategy.
v
Strategy I.A.2: Provide implementation
support to health care providers to help
them adopt, implement, and use certified
EHR technology.
In order to receive incentive payments, eligible
providers must demonstrate that they can use
certified EHR technology to incorporate more
sophisticated uses of health IT, such as clinical
decision support (CDS), patient registries, reminder
systems, and changes to workflow and clinical care
redesign into their practices (see Goal II).
The Regional Extension Center (REC) Program,
established through the HITECH Act with more
than $720 million in grants over a four-year project
period, has set up 62 centers across the nation with
staff and resources dedicated to helping providers
implement and become meaningful users of certified
EHR technology. Additionally, HRSA’s Health
Center Controlled Network (HCCN) Program
provides resources to community health centers to
implement health IT, including EHRs. Further
support is provided by the Health Information
Technology Research Center (HITRC), which will
work to gather relevant information on effective
practices and help the RECs collaborate with one
another and with relevant stakeholders to identify
and share best practices in EHR adoption,
meaningful use, and provider support. Through its
regional offices and other outlets, CMS offers
support to states to encourage adoption of EHR
technology.
Strategy I.A.3: Support the development of a
trained workforce to implement and use
health IT technologies.
To meet the anticipated growth in demand for
health IT professionals, HITECH made available
$118 million to support the training and
development of more than 50,000 new health IT
Federal Health IT Strategic Plan 11
professionals. Four grant programs will prepare
qualified individuals to serve in 12 high priority roles
related to the implementation and maintenance of
EHR systems.
Three grant programs work together to prepare a
workforce in six of these priority roles for which
community colleges are the natural home for
training: Community College Consortia to Educate
Health Information Technology Professionals;
Curriculum Development Centers; and Competency
Examination for Individuals Completing Non-
Degree Training. A fourth program, Assistance for
University-Based Training, will prepare students for
six different roles, for which universities are the
natural home for training.
vi
Strategy I.A.4: Encourage the inclusion of
meaningful use in professional certification
and medical education.
The federal government will encourage meaningful
use to be incorporated into the U.S. medical
education and accreditation processes. To this end,
ONC and CMS are collaborating with various
professional certification and medical education
organizations to assist providers in adopting and
becoming meaningful users and to incorporate
meaningful use into the professional certification
and medical education organizations’ professional
requirements. The American Board of Medical
Specialties, a professional certification body, has
taken steps to assist and encourage physicians in the
adoption and meaningful use of EHRs, with the
ultimate goal that such EHR use and competencies
should become an element of professional
certification.
Strategy I.A.5: Establish criteria and a
process to certify EHR technology that can
support meaningful use criteria.
In order for eligible providers, eligible hospitals, and
critical access hospitals to qualify for the Medicare
and Medicaid EHR Incentive Programs, they must
first adopt certified EHR technology that meets
established criteria, which are aligned with the
Medicare and Medicaid EHR Incentive Programs
meaningful use requirements. The HHS Secretary
has adopted EHR standards, implementation
specifications and certification criteria, as well as a
process for EHR technology to gain certification.
These programs aid providers in selecting certified
EHR technologies that support them in becoming
meaningful users. ONC collaborated extensively
with the National Institute of Standards and
Technology (NIST) to establish the certification
processes.
Established through rulemaking in 2010 and 2011,
ONC’s certification programs specify how
organizations can become authorized by the
National Coordinator to certify EHR technology as
being compliant with the standards, implementation
specifications, and certification criteria adopted by
the HHS Secretary.
ONC published the Initial Set of Standards,
Implementation Specifications, and Certification
Criteria interim final rule in January 2010 and a final
rule in July 2010. The certification criteria establish
the required capabilities, standards, and
implementation specifications in EHR technology
that supports the achievement of meaningful use
stage one. The certification criteria will continue to
evolve with future rulemakings, as further stages of
meaningful use are established.
ONC, with its federal partners, will consider whether
to adopt certification criteria for health IT that is
used by non-eligible providers (such as long-term
and post-acute care facilities), and whether the
availability of certification for specific types of health
IT would be beneficial.
Strategy I.A.6: Communicate the value of
EHRs and the benefits of achieving
meaningful use.
HHS is conducting outreach to providers to increase
awareness of the HITECH Act programs that are
available to support efforts to attain meaningful use
and to share evidence and best practices on the use
of health IT to improve health. Primary care
providers are a primary audience for this strategy
(see Strategies III.B.1 and IV.A.2 for outreach
directed at individuals). The strategy will have four
aims:
Federal Health IT Strategic Plan 12
Raise awareness among providers about the
availability and benefits of EHRs and other health
IT
Educate providers about privacy and security
protections as they relate to EHRs and other
health IT
Encourage providers to participate in HITECH
Act programs and other federal initiatives (e.g.,
Medicare and Medicaid EHR Incentive Programs,
grants, contracts) in order to take full advantage of
EHRs and other health IT
Increase provider understanding of health IT
products and services, so that they may make
informed decisions and take full advantage of the
technologies’ benefits
The education and outreach strategy is being
developed by ONC, CMS, and the Office for Civil
Rights (OCR), and will be implemented over the
next two years.
Strategy I.A.7: Align federal programs and
services with the adoption and meaningful
use of certified EHR technology.
HHS is committed to encouraging providers that are
not eligible for the Medicare and Medicaid EHR
Incentive Programs to use EHR technologies to
improve the care they provide to patients. For future
stages of meaningful use, HHS plans to propose
more rigorous health information exchange
requirements which may encourage providers that
are not eligible for the incentive programs (e.g., long-
term and post-acute care facilities, community
mental health centers or substance use disorder
treatment providers) to adopt health IT and
participate in health information exchange. The
Federal Health IT Taskforce,
vii
consisting of the
National Coordinator for Health IT, administration
officials, and other federal agency leads for health
IT, is the key federal committee responsible for
coordinating federal health IT investments and
aligning programs to support meaningful use of
certified EHR technology.
Specifically, the Department of Defense (DoD),
Department of Veterans Affairs (VA), and Indian
Health Service (IHS) are developing plans for their
health care systems to align with meaningful use.
Similarly, the Health Resources and Services
Administration (HRSA) and the Federal
Communications Commission (FCC) are developing
plans to encourage their grantees and subsidy
recipients, respectively, to become meaningful users.
The Substance Abuse and Mental Health Services
Administration (SAMHSA) is working to foster
adoption and implementation of certified EHRs
among its providers that are ineligible for the
Medicare and Medicaid EHR Incentive Programs,
including community mental health centers and
substance use disorder treatment facilities. Finally,
the Office of Personnel Management (OPM) is
developing a strategy to encourage health plans that
provide coverage through the Federal Employee
Health Benefits (FEHB) Program to support EHR
adoption and meaningful use among their networks
of providers.
Strategy I.A.8: Work with private sector
payers and provider groups to encourage
providers to achieve meaningful use.
The federal government will support the efforts of
private payers and private provider groups to
encourage their networks of providers to achieve
meaningful use. Some major payers have begun to
implement incentive programs that will work in
parallel with the Medicare and Medicaid EHR
Incentive Programs and utilize meaningful use
objectives. These programs have the potential to
play a role in expanding the number of providers
who achieve meaningful use, and may also provide
incentives for providers who are not eligible for the
Medicare and Medicaid EHR Incentive Programs. In
addition, some private sector payers are
implementing new payment models that increasingly
rely on collaboration among health care providers to
coordinate patient care and achieve efficiencies.
These new payment models are helping to create a
business case for providers not eligible for incentives
under the Medicare and Medicaid EHR Incentive
Programs to adopt health IT and participate in
health information exchange.
Strategy I.A.9: Encourage and facilitate
improved usability of EHR technology.

Federal Health IT Strategic Plan 13
The government is collaborating with industry and
researchers to improve the usability of EHRs. The
usability of EHRs is considered a key barrier to
adopting health IT and achieving meaningful use.
NIST is conducting ongoing research and advancing
the development of standards and test methods that
can be used to evaluate and improve the usability of
EHRs. It has released a Common Industry Format
(CIF), a standard for developers to report usability
test findings and demonstrate evidence of usability in
their products in a format that allows for
independent evaluation of a single product and
comparison across multiple products. NIST is also
developing guidance and tools for RECs and
professional societies on available tools and
resources to incorporate concepts of usability in
selecting and implementing EHR systems. The Food
and Drug Administration (FDA), in collaboration
with NIST and the Agency for Healthcare Research
and Quality (AHRQ), will develop best practices to
address systematic evaluation of usability with regard
to patient safety to ultimately improve patient care.
AHRQ is developing toolkits that medical practices
can use to assess the usability of EHR systems and
assess the redesign workflow. In addition, AHRQ is
conducting research and convening industry
workgroups that provide perspectives on what
constitutes usability and how to systematically
improve the usability of EHRs.
ONC will explore ways to improve the ability of
providers to select or change EHR products by
improving data portability. Reducing the cost
associated with switching products while increasing
data fluidity and choice can help drive market
competition to improve the usability of EHR
products.
ONC has directed one of its four Strategic Health IT
Advanced Research Projects (SHARP) (see Strategy
V.B.2) to further EHR usability through the
identification and development of better cognitive
and user-centered design. In addition, ONC is
working with private sector groups to encourage the
collection of usability information and its
dissemination to vendors and consumers through
mechanisms they can trust.
OBJECTIVE B
Facilitate information exchange to
suppor
t meaningful use of electronic
health records
For future stages of meaningful use, the plan is to
propose health information exchange and
interoperability requirements that are more rigorous,
so that patient information follows patients to the
point of care and informs critical health decisions.
This will require overcoming barriers across
geographies and stakeholders (i.e. providers,
laboratories, hospitals, pharmacies, behavioral health
clinics, and patients), including insufficient demand
for electronic health information, lack of a business
model for facilitating exchange, and disparate
federal, state, and local policies that hinder exchange.
It will also require more rigorous standards to
support interoperability so that the data that is
exchanged can be used for multiple purposes.
Historically there have been significant barriers to
the adoption and use of EHRs to exchange
information, including their cost, low provider
demand, the perceived lack of financial return for
investing in them, and the technical and logistical
challenges involved in installing, maintaining and
updating them.
viii
But the Medicare and Medicaid
EHR Incentive Programs and the Affordable Care
Act payment reforms are sparking a paradigm shift
in the collection and use of health care data that
addresses some of these challenges head on. First,
the Medicare and Medicaid EHR Incentive
Programs reward eligible professionals and hospitals
who digitize health care information. We anticipate
that the requirements for sharing information
electronically across provider settings will grow
stronger in future stages. Second, ongoing payment
reforms initiated by the Affordable Care Act –
including accountable care organizations, medical
home models, and bundled payments – are an even
more important potential driver of provider
motivation to exchange information. Private sector
payers may also adopt similar payment reforms to
align with Medicare and Medicaid. To prepare for
such reforms, hospitals are already reaching out to
their surrounding community providers to share
Federal Health IT Strategic Plan 14
information and EHR systems. Eventually, as digital
health information becomes more widely available,
exchanging it will be more natural and incentives will
become less relevant. Several challenges also exist to
creating a national infrastructure whereby business
networks can connect to one another, including but
not limited to the development of consistent
standards to ensure interoperability and privacy and
security protocols to ensure trust that the network
will handle information appropriately. Health
information exchanges (HIEs) must be designed to
address legal, organizational, and technical challenges
that might otherwise impede their sustainability.
With demand increasing, the government is helping
to ensure that exchange standards and infrastructure
are in place to meet it. This does not mean
constructing significant new national infrastructure
from scratch. Rather, the federal government, in
close collaboration with state governments, is
helping evolve the various current exchange models,
so that – taken together – they may serve every
health care provider and meet a broader set of health
care needs. There are many examples of information
sharing that are already occurring in the health care
system, and the government will foster the growth
and development of these models. Where there are
gaps in exchange options, the government will
identify the specific barriers to exchange and develop
plans to address them. Finally, so that
communication and information sharing can take
place across various information exchange models –
both public and private – the government will
advance national adoption of key exchange
standards.
Strategy I.B.1: Foster business models that
create health information exchange.
Many sustainable exchange options already exist for
certain providers and certain types of health
information. Some hospital networks and group
provider practices have found a business case for
investing in information exchange within their
networks. Vendors of EHR systems are developing
“information networks” for their customers.
Communities are creating health information
networks to facilitate information sharing among
providers. Diagnostic lab companies and electronic
prescription companies are offering services that
enable exchange of specific pieces of health
information for providers able to pay for them. The
Nationwide Health Information Network standards,
services, and policies – including the Nationwide
Health Information Exchange and Direct protocols
– are being used by many health care organizations
as the preferred solution to exchanging information
across organizational and geographic boundaries.
Protocols such as Blue Button (see Strategy IV.B.2)
provide a method to electronically exchange health
information between providers and consumers. The
Blue Button is an initiative at DoD, VA, and CMS
that enables individuals to access a web-based portal
to download their personal health information and
share this information with health care providers,
caregivers, and others they trust.
For as many providers as possible, the first priority is
finding the right combination of already-available
exchange models that will enable them to
electronically exchange lab results, patient care
summaries, and medication histories. State-level
grantees in the State HIE Cooperative Agreement
Program are identifying, articulating, and promoting
adoption pathways that will help providers do just
that. RECs will work with individual providers to
identify and implement the right pathway.
ONC is also making it easier, faster, more secure,
and less expensive to transport health information.
The Direct project at ONC enables a simple, secure,
scalable, standards-based way to send authenticated,
encrypted information directly to known, trusted
recipients over the Internet. Direct helps some
providers satisfy the stage one meaningful use
requirements by allowing a secure method of
pushing content from a sender to a receiver. For
example, by leveraging Direct, a primary care
physician can send a secure email with a clinical
summary of a patient to a referring specialist. Direct
is a national solution to health information exchange
that can rapidly lower the cost and complexity of
local interfaces between providers, laboratories,
hospitals, pharmacies, and patients, in turn
substantially lowering the cost of providing
information exchange services. In some cases this
could make it possible for a small provider to
Federal Health IT Strategic Plan 15
connect to a lab company or a health information
exchange organization, where it may have been cost
prohibitive for them to do so otherwise. Federal
partners that provide health care services, including
the VA, are implementing Direct as a consistent,
national solution for directed exchange in local
communities. The RECs will promote EHRs that
already have the Nationwide Health Information
Network Direct interfaces built in, lowering the cost
of exchange for small providers. Continuing work to
simplify and extend the Nationwide Health
Information Network will continue to focus on
lowering the cost of exchange and improving the
interoperability of EHR systems.
ONC continues to work with the private sector and
federal health care organizations to further refine the
standards, services, and policies for securely
exchanging authorized health information between
providers through the Nationwide Health
Information Network Exchange protocols. For
example, the query/response protocols provide a
method of exchanging information, when
authorized, between a provider and another
authenticated entity that may have information on a
patient that is necessary for care. In this case, a
query is sent to providers with an authorization and
responses are sent with the needed information.
This model provides a high level of information
exchange potential and capability. It also requires a
robust electronic health record system and
investment. Currently, the Nationwide Health
Information Network Exchange is primarily used by
a group of federal agencies and private organizations
that have come together to securely exchange
electronic health information and are demonstrating
the capabilities of information exchange. Today,
select participants in the Nationwide Health
Information Network Exchange are: exchanging
summary patient records for Social Security
Administration (SSA) disability determination
purposes; exchanging summary patient records for
the Virtual Lifetime Electronic Health Record
(VLER); and participating in bio-surveillance and
case reporting with CDC. The Exchange protocols
and the pilot programs that are using them will help
pave the way for broader adoption of
query/response exchanges as envisioned by the
authors of the President’s Council of Advisors on
Science and Technology (PCAST) December 8, 2010
report, Realizing the Full Potential of Health Information
Technology To Improve Healthcare for Americans: The Path
Forward and many health information thought
leaders.
In addition to the exchange of health information
between providers, the exchange of information that
engages individuals and gives them access to their
health data is a top priority of the Medicare and
Medicaid EHR Incentive Programs. The best way to
empower individuals and reorient the health care
system to be more patient-centered is to give
patients access to their personal health information.
Information exchange protocols such as the Blue
Button format that was developed and adopted by
the VA, DoD, and CMS, is one way to put patients
at the center and give them control of their
information. ONC supports the exchange of
information with consumers and the re-use of such
information for themselves and with providers.
This portfolio of exchange mechanisms is part of a
broad national strategy to have an interconnected
health system through the Nationwide Health
Information Network. The Nationwide Health
Information Network is being developed by ONC to
provide the building blocks for a secure, nationwide,
interoperable health information infrastructure that
can connect providers, consumers, and others
involved in the health care system. Exchange, Direct
and evolving methods of health information
exchange create an infrastructure that is critical to
enabling health information to follow a patient and
be available for clinical decision making and uses
beyond patient care, such as measuring quality.
Finally, the government will also seek to remove
unnecessary regulatory barriers to sustainable
exchange options, helping them to develop. In
collaboration with the State HIE Cooperative
Agreement Program, for instance, state governments
will look for ways to align Medicaid policies to health
information exchange requirements.
Strategy I.B.2: Monitor health information
exchange options and fill the gaps for
providers that do not have viable options.
Federal Health IT Strategic Plan 16
Many providers – particularly those in areas with low
hospital and provider density – are not currently
supported by sustainable information exchange
models. A main focus of the State HIE Cooperative
Agreement Program is expanding existing networks
to help these providers. The program is investing
over $500 million in supporting state-level initiatives
to expand capacity for exchanging health
information both within and across states. It
encourages states to develop statewide HIE plans
which will align with the nationally recognized
standards and services and state Medicaid initiatives.
States will support providers by building on existing
exchange activities, providing critical shared services
and infrastructure such as provider directories,
record locator services, and master patient indices,
increasing the use of standards, services, and policies
needed for widespread information sharing, and
enhancing the information exchange capabilities of
key trading partners including clinical laboratories,
pharmacies, and public health agencies.
In order to exchange health information
electronically, providers must have broadband
Internet access. The FCC’s Rural Healthcare
Program subsidizes broadband access for health care
providers that are disadvantaged in meeting this
requirement. The program is authorized to spend up
to $400 million per year to ease the burden of costly
telecommunications services for rural health care
providers. The program is divided into two different
components: one that subsidizes ongoing monthly
costs, and one that helps providers build new
infrastructure where the existing infrastructure is
insufficient. In addition, the U.S. Department of
Agriculture (USDA)’s Broadband Technologies
Opportunities Program (BTOP) and Department of
Commerce’s Broadband Initiatives Program (BIP)
were collectively funded by over $4 billion through
the Recovery Act to support broadband grants
around the country. Health care was one of the
strategic priorities of these grant programs.
The government will also encourage consumers to
gather and exchange their own individual health
information. Informed and engaged consumers who
have access to their own interoperable health records
can be a powerful force for bringing that
information with them to the point of care. See Goal
IV for more detail on how the government will
accelerate consumers’ and caregivers’ access to their
electronic health information in a format they can
use and reuse.
Strategy I.B.3: Ensure that health
information exchange takes place across
individual exchange models, and advance
health systems and data interoperability.
Electronic health information can be a critical
element in the implementation of business models,
such as bundled payments and accountable care
organizations being implemented through the
Affordable Care Act. These delivery system reform
models will rely on richer and more timely
information to better align payments with the actual
costs of providing efficient care. These efforts, as
well as future proposals for subsequent stages of
meaningful use, will rely on these emerging models
for sustainable information exchange and will likely
require greater capacity for connecting the various
models – so that providers may securely send health
information to any other authorized provider
through the Internet. HHS recognizes that the
government has a duty to help ensure that health
information can flow where needed and follow
patients where they go, consistent with patient
preferences. CMS recently reinforced this policy in
its proposed regulations on accountable care
organizations
ix
Nationally, the government is developing a standards
and interoperability framework (S&I framework) to
harmonize existing standards and improve sharing of
standards across different organizations and federal
agencies, making it easier to broaden interoperability
through shared standards for data and services. In
order to support exchange and advance
interoperability, there are three types of standards
that the S&I framework will support.
. ONC is putting in place the
standards, services, and policies to support the
infrastructure needed to connect these emerging
models for exchange.
First, the S&I framework will focus on identifying
transport standards. These standards enable one
provider to exchange data with another provider, or
Federal Health IT Strategic Plan 17
one system to another system, securely. A second
type of standards is necessary for the data to be
interoperable between different providers, or
systems. These are known as content standards,
which allow data to be packaged or “read” in a way
that is useful for the provider. For example, the
Medicare and Medicaid Incentive Programs’ stage
one criteria require that an eligible professional
generate and transmit prescriptions electronically.
The S&I framework ensures that standards are
available that enable certified EHR technology to
view data in a way that is usable to the provider in
ordering the prescription and usable to the
pharmacist receiving the prescription. Lastly, the
S&I framework will identify vocabulary and
terminology standards and value sets in order to
achieve semantic interoperability at the level of
individual data elements. ONC will work to reduce
variability in vocabulary and terminology standards
which will help to reduce costs and to move toward
more semantically interoperable health information
exchange. ONC will work with its federal partners
and standards development organizations to
harmonize the existing standards and vocabularies
they produce to create the building blocks and
implementation packages in support of national
priorities, including meaningful use.
The S&I framework is intended to be flexible, so
that it can be used to establish meta-data standards,
or “data about data,” that include additional
information about the context in which the data has
been collected. The S&I framework will provide
tools, data and meta-data standards, value sets, and
service descriptions in an integrated and harmonized
way to support meaningful use and interoperability,
and focus these efforts on the highest priority kinds
of information exchange. ONC is leading this effort
in close collaboration with other federal agencies.
The S&I framework will support not only existing
specifications for the Nationwide Health
Information Network, but also support new meta-
data tagged approaches recommended by the
President’s Council of Advisors on Science and
Technology (PCAST) December 8, 2010 report,
Realizing the Full Potential of Health Information
Technology To Improve Healthcare for Americans: The Path
Forward.
ONC, and its federal partners, will continue to use
the HIT Policy and HIT Standards Committees
(ONC’s federal advisory committees) to provide
recommendations on priorities for standards. ONC,
and its partners, will promote the adoption of
standards through the Medicare and Medicaid
Incentive Programs and other federal programs.
In establishing and maintaining the S&I framework,
ONC will leverage the National Information
Exchange Model (NIEM) processes. NIEM is a
government collaborative of the U.S. Department of
Justice, the U.S. Department of Homeland Security,
and HHS designed to develop, disseminate, and
support enterprise-wide information exchange
standards and processes to enable jurisdictions to
effectively share critical information. NIEM
processes will help ensure that existing applicable
standards are re-used when possible, creating
efficiencies in the government standards work. ONC
will work with its federal partners to leverage the
NIEM processes where possible and add to it as
necessary.
This strategy recognizes the experience and
leadership of federal agencies and offices – including
National Institutes of Health/National Library of
Medicine (NIH/NLM), Centers for Disease Control
and Prevention (CDC), CMS, AHRQ, FDA, and the
Office of the Assistant Secretary for Planning and
Evaluation (ASPE) – and private sector standards
development organizations and aims to leverage
existing standards and standards development
processes where possible. The federal government
has a role in ensuring that standards designated for
U.S. health information exchange are readily
available and are regularly maintained and enhanced
in response to feedback from implementers and
users. Federal agencies encourage the adoption and
use of standards, participate and coordinate actively
in standards development organizations, and direct
and support specific standards development projects
to address implementation problems and fill gaps. In
the case of some terminologies and code sets, federal
agencies, including NIH, CDC, CMS, and FDA,
support the development and ongoing maintenance
and free dissemination of designated standards and

Federal Health IT Strategic Plan 18
promote their use across the spectrum of health
care, public health, and research.
Using the integrated set of specifications developed
in the S&I framework and shared services and
infrastructure (e.g., provider directories, record
locator services, and master patient indices), the
Nationwide Health Information Network will be the
preferred solution to securely exchange information
nationwide to support meaningful use. Health care
organizations using the Nationwide Health
Information Network to share health information
can serve as innovators, creating a pathway to more
advanced health information exchange and
interoperability.
In order to engender trust and interoperability and
facilitate broad participation in the Nationwide
Health Information Network, ONC will establish a
governance mechanism through rulemaking that
seeks to include accountability and oversight of
nationwide information exchange. The Nationwide
Health Information Network governance rules will
be established as a voluntary solution to health
information exchange. The government will pursue
various options to encourage participation in this
preferred solution to nationwide information
exchange.
In carrying out its assigned duties, ONC is tracking
standards activities in other countries and learning
from their experiences with health IT and health
information exchange. Currently, ONC is working to
identify whether there are internationally recognized
standards that should be endorsed for use in the
United States. To further this effort, ONC intends to
participate in international efforts to identify
interoperability standards and implementation
specifications for EHR technologies that will
facilitate data and systems integration. ONC’s input
into these international standards activities should
ensure that U.S. standards will work with the
international community in the event of global
public health emergencies.
OBJECTIVE C
Support health IT adoption and
information exchange for public
health and populations with unique
needs
Strategy I.C.1: Ensure public health
agencies are able to receive and share
information with providers using certified
EHR technology.
CDC, CMS, FDA, NIH, HRSA, the Assistant
Secretary for Preparedness and Response (ASPR),
and ONC are working together to ensure that
meaningful use of certified EHR technology
supports the needs of public health agencies.
Meaningful use stage one currently includes an
objective on the menu set to submit electronic
syndromic surveillance data, immunization registries,
and electronic lab reporting to public health
agencies. This will pave the way for EHRs to
exchange information with local, state, and federal
public health agencies and will set the stage for two-
way communication between providers and these
public health agencies prior to, during, and after an
incident. Eventually, information exchange between
providers and public health entities can be expanded.
It can include routine and emergency public health
preparedness and response, and many-ways
exchange of information (i.e., between different
providers, public health agencies at different
jurisdictions, and public health reference
laboratories) for immunizations, public health case
reports, and situational awareness reports. CDC is
helping local and state public health agencies prepare
their systems and processes for such changes.
Through the State HIE Cooperative Agreement
Program, state governments and state Medicaid
agencies will play a key role in building the public
health infrastructure to support meaningful use. As
with clinical data, public health departments require
public health standards to effectively exchange
information. CDC’s Public Health Informatics and
Technology Program Office (PHITPO) at the Office
of Surveillance, Epidemiology and Laboratory
Services (OSELS) is leading the development of
public health standards in coordination with FDA,
NIH and other agencies, that align with certified
EHR technology.
Federal Health IT Strategic Plan 19
Strategy I.C.2: Track health disparities and
promote health IT that reduces them.
In order to achieve nationwide adoption and
meaningful use of certified EHRs, it is critical that
providers who face unequal challenges in adopting
and using EHRs be included in the government’s
initiatives. The RECs are providing outreach and
technical assistance to support providers who serve
underserved communities and resource-poor
settings, including small practice settings, rural
hospitals/clinics, community health centers, and
Critical Access Hospitals. The RECs will work
through community-based organizations and will
develop tailored solutions and best practices to reach
these providers. RECs will also collaborate with
groups representing underserved and minority
providers on the national and local levels.
ONC is also investing in better ways to monitor and
identify disparities in health IT adoption. This effort
can enable ONC to measure health IT adoption
disparities and focus resources on areas of greatest
need to mitigate disparities.
HHS is evaluating approaches for using health IT to
collect and analyze data about disparities (on the
bases of race, ethnicity, gender, primary language,
and disability status) in health and health care
provision, and using this data to improve the care of
underserved populations. Beacon Community
grantees are acting as test sites for using health IT
for this purpose. RECs will disseminate best
practices identified by Beacon Communities to
providers and other organizations serving
underserved communities. NIST will provide
technical guidance for EHR design and
development, in order to help prevent the creation
or exacerbation of health care disparities with the
adoption and utilization of EHRs.
Through efforts underway related to the Medicare
and Medicaid EHR Incentive Programs, the
Children’s Health Insurance Program
Reauthorization Act (CHIPRA) of 2009, and other
initiatives authorized by the Affordable Care Act,
HHS is developing electronic clinical quality
measures that enable providers and hospitals to
gauge the health status of their communities. Also,
standards developed to support meaningful use will
strengthen data collection and quality measurement,
enabling quality improvement efforts that reduce
health disparities.
Existing health IT applications such as telehealth can
be used to address gaps in access and quality of
health care services. Telehealth uses electronic
information and telecommunications technologies
such as videoconferencing and wireless
communication to support long-distance care. The
HRSA Health Disparities Collaboratives (HDC)
were created to assist in the transformation of
primary health care practices in order to improve the
care provided to everyone and to eliminate health
disparities. HDC now continues as a private
endeavor. HRSA’s Telehealth Network Grant
Program supports established telehealth networks
that are looking to expand the number of sites that
are receiving clinical services. HRSA’s Telehealth
Resource Program funds Centers of Excellence,
which provide technical assistance on telehealth to
any HRSA grantee in the country. In addition, IHS,
VA, CMS, and USDA all take advantage of
telehealth technologies to meet the needs of
disparate populations. In order to improve access to
quality health care services through telehealth, ONC
is working with states to increase medical licensure
portability by streamlining licensure application and
credentials verification processes so providers can
more easily apply for a license in multiple states.
ONC is also working with HRSA on developing a
report to Congress for the use of health information
technology in underserved communities.
Strategy I.C.3: Support health IT adoption
and information exchange in long-term/
post-acute, behavioral health, and
emergency care settings.
Providers working in long-term and post-acute care
(LTPAC) and behavioral health settings are essential
partners in patient care coordination. ONC, CMS,
and ASPE will collaborate to address quality
measures and evolving clinical decision support
opportunities that will promote appropriate
exchange of health information in LTPAC and
behavioral health care settings for optimal
coordination of care.
Federal Health IT Strategic Plan 20
HHS will build on meaningful use to adopt
electronic standards for the exchange of clinical data
among facilities and community-based LTPAC
settings, including, where available, standards for
messaging and nomenclature. ONC will leverage the
State HIE and Beacon Community grant programs
in demonstrating methods for which the electronic
exchange of information with LTPAC entities can
improve care coordination. In addition, HHS will
identify opportunities in the Affordable Care Act to
support the use of health information exchange
technologies by LTPAC and behavioral health
providers to improve quality of care and care
coordination.
SAMHSA, in collaboration with ONC, will explore
approaches to support adoption of certified EHR
technology within the behavioral health community.
ONC is working with SAMHSA and HRSA to
address the policies and standards concerning the
unique needs of behavioral health IT adoption and
information exchange. This includes work on data
and meta-data standards that can provide additional
clinical context such as patient preferences and
sources of data to help enable data segmentation and
secure exchange of sensitive health information. The
ability to integrate mental health data into the
primary care and related safety net system is essential
for coordinating care.
Recognizing that emergency care settings are
essential places for patient care coordination, ONC
and ASPR will explore ways to address the need for
clinical data to be available in emergency care
situations and identify policies and standards that are
necessary to support these needs.
Federal Health IT Strategic Plan 21
Goal II: Improve Care, Improve Population Health, and
Reduce Health Care Costs through the Use of Health IT
he recently passed Affordable Care Act will
transform American health care from a
system that emphasizes transactions to a
system that emphasizes improved care,
improved population health, and reduced per capita
costs of health care. The widespread adoption and
meaningful use of certified EHR technology is a
necessary interim step in this transformation. It will
be essential to build upon this health IT
infrastructure and use the information made
available by EHRs in order to move toward HHS’
three overarching aims. But while health IT is
necessary to affect such changes, technology by itself
is insufficient. For this reason, federal health IT
investments are being made in lockstep with other
reform efforts, many of which were initiated and
funded by the Affordable Care Act.
Programs underway at ONC and AHRQ are looking
at ways to combine more sophisticated uses of
health IT and clinical care redesign to achieve better
health outcomes and improve health system
performance. The HITRC and REC programs will
make these best practices – such as using clinical
decision support tools,
patient registries, and
reminder systems – a
vailable to providers
throughout the country. The CHIPRA Quality
Demonstration grants are also expected to
demonstrate promising new ways that health IT can
be used to improve pediatric health care. CMS
expects that for future stages of meaningful use, the
financial incentives will encourage providers to use
more sophisticated health IT to achieve higher level
improvement measures. HHS will leverage both
the
Medicare and Medicaid EHR Incentive Programs
and the implementation of administrative
simplification requirements under Section 1104 of
the Affordable Care Act to create cost savings
through increased standardization and automation of
health care administrative functions.
A key part of the Affordable Care Act is the
development of quality and outcome measures. E-
measures can facilitate the electronic capture, reuse
and reporting of health data. E-measures will
support federal and state quality improvement
efforts and enable providers to assess their own
performance with their patients.
Central to both the HITECH Act and the
Affordable Care Act is fostering and learning from
breakthrough examples of health care delivery
system change, which can then serve as models for
more widespread changes. The Beacon Community
grants from the HITECH Act have created 17
demonstration communities in which clinicians,
hospitals, payers, and patients will show how
advanced uses of health IT can achieve
improvement goals in care, efficiency, and
population health. The new CMS Center for
Medicare and Medicaid Innovation will test a range
of innovative payment and service delivery models,
many of which will require advanced uses of health
IT to achieve their objectives. These examples may
employ the latest health IT – remote monitoring,
telehealth, mobile health (mHealth) applications, and
the most advanced means of information exchange –
and could become achievable, sustainable, and
replicable examples of how the government can
build upon the nationwide adoption and meaningful
use of EHRs.
Finally, the Affordable Care Act directs HHS to
develop a national strategy for prevention and health
promotion. Health IT will play a fundamental role in
supporting this national strategy, providing the
necessary infrastructure for disease prevention, early
detection, and condition management before an
illness becomes severe. CDC, in collaboration with
state, local, and other federal public health agencies,
leads federal efforts to provide and improve the core
capacities of the public health IT infrastructure.
Health IT facilitates coordination across public
health entities and other organizations, improves
identification of at-risk populations and their
adherence to public health guidelines, expedites
responses to threats, notifiable conditions, and
adverse population events, and promotes consumer
T
Federal Health IT Strategic Plan 22
participation in public health by encouraging healthy
behaviors and behaviors that screen for, detect, and
effectively manage disease.
The government has four objectives to “Improve
Care, Improve Population Health, and Reduce
Health Care Costs through the Use of Health IT”:
A. Support more sophisticated uses of EHRs and
other health IT to improve health system
performance
B. Better manage care, efficiency, and
population health through EHR-generated
reporting measures
C. Demonstrate health IT-enabled reform of
payment structures, clinical practices, and
population health management
D. Support new approaches to the use of
health IT in research, public and population
health, and national health security
Spotlight on Health Outcomes
Health IT and information sharing can improve medical decision-making
These “Spotlight on Health Outcomes” are intended to highlight exemplary ways that widespread adoption and use of health IT and electronic health
information exchange could help transform and improve health care. Some of these examples are only aspirational today or only exist in select
communities or health systems. However, these examples illustrate the type of transformed health care that could be possible with the achievement of
the goals of this Plan.
See endnotes for citations.
Meaningful use of EHRs can result in more effective
management of the risk factors associated with heart disease.
George’s PCP works within a patient-centered medical home
model that provides the organizational infrastructure and
support so that she can best manage George’s care. This
model helps to improve coordination of George’s care by
enabling any specialists George sees and PCP to
electronically access and share critical information to make
better informed, appropriate and timely care decisions.
Through electronic information exchange, all the providers
on George’s care team are able to seamlessly review George’s
most recent blood pressure reading, smoking status, labs,
diagnostic tests, and clinic visit notes. George’s cardiologist is
able to make recommendations using information in real
time, and his PCP can view the care plan in the EHR. All of
these providers can share in the reward for providing better
value health care and keeping George healthy.
While in the hospital, Jane’s physician notices she is slurring
her speech and exhibiting some slight right arm weakness. He
believes she is having a stroke and instructs the care team to
start the appropriate treatment protocol. To confirm the
diagnosis, Jane’s phycian consults her health record that is
shared by all the providers on her care team. He notices that
in a visit with her PCP last week, there is no indication of a
problem with Jane’s speech or strength in either arm, which
suggests these symptoms are new. The physician discusses
with Jane and her family that she is likely having a stroke.
With the patient’s and her family’s consent, the medical team
performs a CT scan of Jane’s head and starts medication
immediately to break up the clot and save Jane from a
potentially
debilitating stroke. Without the shared
information on hand, Jane’s symptoms may not have been
noticed.

Federal Health IT Strategic Plan 23
OBJECTIVE A
Support more sophisticated uses of
E
HRs and other health IT to improve
health system performance
Strategy II.A.1: Identify and implement best
practices that use EHRs and other health
IT to improve care, efficiency, and
population health.
Goal I of this plan describes the Medicare and
Medicaid EHR Incentive Programs’ payments
available to providers who become meaningful users
– the centerpiece of the government’s health IT
strategy. The success of the meaningful use program
will create the fundamental health IT adoption
within the health system necessary to support the
health reform efforts outlined in the Affordable Care
Act. The Medicare and Medicaid EHR Incentive
Programs, as established by the HITECH Act,
represent a significant step in enhancing the
performance of the health system. The Medicare and
Medicaid EHR Incentive Programs also create a
basic health IT and information exchange
foundation that can support further improvement
interventions that are either not possible or too
difficult and burdensome on providers without this
foundation.
The HITRC program makes tools and best practices
available to providers as they implement clinical care
redesign and more sophisticated health IT into their
offices. HITRC will identify ways to build on EHR
use by changing clinical workflows and integrating
EHR software, patient registries, and medication
reminder systems. The use of these tools can
support better decision-making at the point of care
and increased adherence to treatment regimens,
helping move health care from a reactive system to
one that focuses on prevention and improved care
management.
Clinical decision support (CDS) systems are tools
that leverage EHRs to improve clinical processes.
Broadly, these software systems build off of EHRs,
giving providers helpful information and analytical
support at the point of care. Various clinical decision
support rules can help providers analyze patient
information, supply them with performance reports
against quality measures, and assist them with
diagnoses.
AHRQ and CDC will continue their critical role in
assessing and promoting best practices related to
how health IT can be utilized to improve quality of
care, patient engagement in self-care, management of
chronic diseases, and management of public and
population health.
Promising practices and lessons learned from the
CMS CHIPRA Quality Demonstrations will be
communicated on a regular basis to State Medicaid
and CHIP programs to further promote successful
HIT and EHR initiatives important to vulnerable
populations.
With the establishment of the REC program, the
government now has a way to disseminate tools and
best practices to providers that need the most help
in implementing them into their practices. The RECs
will build on their existing relationships with these
providers to help them achieve improved health
outcomes through more sophisticated uses of EHRs
and other health IT.
Strategy II.A.2: Create administrative
efficiencies to reduce cost and burden for
providers, payers, and government health
programs.
For future stages of meaningful use, HHS expects to
propose measures that simplify administrative
processes and help lower costs in the clinical setting.
In January 2009, HHS adopted modifications to two
HIPAA Administrative Simplification medical data
code set standards for medical diagnosis and
inpatient procedure coding. Under these regulations,
covered entities will be required to transition from
using the International Classification of Diseases,
Ninth Revision, Clinical Modification (ICD-9-CM)
in HIPAA-covered transactions to using the
International Classification of Diseases, Tenth
Revision, Clinical Modification (ICD-10-CM/PCS),
Procedure Coding System in October 2013. ICD-10-
CM/PCS code sets will enable a more granular
understanding of health care treatments and
outcomes, and more complete analyses of treatment

Federal Health IT Strategic Plan 24
costs, ultimately allowing for better disease
management and more efficient health care delivery.
In expanding coverage to as many as 32 million new
Americans, the Affordable Care Act called for some
specific technology-enabled improvements in the
government’s administration of health care. These
include: standards and protocols for streamlining
eligibility and enrollment into federal and state health
and human services programs; a consumer portal for
accessing health insurance information online; and
the creation of new health insurance exchanges by
2014. To fulfill the requirement under Section 1561
of the Affordable Care Act to develop interoperable
and secure standards and protocols to facilitate
enrollment of individuals in federal and state health
and human services programs, ONC organized a
workgroup, under the auspices of the HIT Policy
Committee and HIT Standards Committee, that
produced recommendations to those committees,
which were approved by the full committees to
facilitate more seamless enrollment processes. The
government will incorporate standards and criteria as
a condition for receiving federal grant funding for
these systems, and will employ other mechanisms to
further the development of efficient eligibility and
enrollment systems. ONC will support the
implementation of these health information
technology improvements where mandated by law,
and in all cases will ensure that the Affordable Care
Act technology implementation efforts are
synchronized with federal priorities for meaningful
use and health IT privacy and security. HHS will also
reduce the burden for providers when reporting
required data to federal agencies through use of data
standards and efficient and effective information
exchange planning and design.
OBJECTIVE B
Better manage care, efficiency, and
po
pulation health through EHR-
generated reporting measures
Strategy II.B.1: Identify specific measures
that align with the National Quality
Strategy.
In March 2011, HHS established the National
Quality Strategy, as required by the Affordable Care
Act. The Plan initially focuses on six priorities that
have great potential for rapidly improving health
outcomes and increasing the effectiveness of care for
all populations. As the National Quality Strategy is
implemented in 2011 and beyond, HHS will work
with stakeholders to create specific quantitative goals
and measures for each of these priorities. A part of
these activities will be the development of e-
measures that can collect and report data through
EHRs. HHS agencies will work together to ensure
the development of e-measures that are aligned
across reporting programs to reduce the burden on
providers and that can be supported by the
implementation of the Medicare and Medicaid EHR
Incentive Programs.
Strategy II.B.2: Establish standards,
specifications, and certification criteria for
collecting and reporting measures through
certified EHR technology.
Based on the measures defined in II.B.1, ONC, in
collaboration with others in HHS, VA, and DoD will
establish standards, specifications, and certification
criteria for EHRs that facilitate the collection and
reporting of e-measures. Using the S&I framework,
these e-measures will be harmonized with other
standards used to support data collection and
information exchange. The development of e-
measures will lead to more cost efficient and timely
assessments of health care performance.
Building e-measures into EHRs will allow providers
to assess and monitor their health care performance.
ONC will make available open source tools that help
providers submit quality measures to government
agencies, better understand their patient populations,
and identify opportunities for improving the health
of their patients.

Federal Health IT Strategic Plan 25
OBJECTIVE C
Demonstrate health IT-
enabled reform
of payment structures, clinical
practices, and population health
management
Strategy II.C.1: Fund and administer
demonstration communities to show how
the advanced use of health IT can achieve
measurable improvements in care,
efficiency, and population health.
ONC is funding 17 Beacon Communities with the
specific mission to identify and show improvement
on care, efficiency, and population health outcomes
through the use of health IT. VA and HRSA are
partnering with ONC to support these Beacon
Communities. By 2014, Beacon communities are
expected to demonstrate that their advanced uses of
health IT, and associated outcome improvements,
are both possible and replicable. By 2015, they are
anticipated to show how these efforts can be
expanded to other communities and how they can
be sustained over time. Key findings from these
communities will be incorporated into guidance for
RECs, State HIE programs, and meaningful use
proposed objectives, and thus, will be expanded to a
national scale.
Strategy II.C.2: Align health IT initiatives
and clinical and payment reform pilots and
demonstrations.
The Affordable Care Act authorized a wide range of
innovative programs using payment reforms to
promote quality, efficiency, and equity of care. These
include bundled payment pilots, medical home
pilots, and others. CMS will have the charge to
quickly and effectively translate knowledge from
these innovative programs into wider CMS policy.
Health IT will be an important tool to support many
of these demonstration projects. The federal
government will work to assure that, when
appropriate, health IT is properly leveraged for these
innovative programs, and that proven outcomes
associated with defined uses of health IT are
encouraged in the wider health care community.
O
utside of ONC and CMS, there are many other
examples of health IT-enabled reform being
implemented today. Private sector technology
companies, provider networks, payers, and public
providers such as VA, IHS, and DoD, are funding a
wide range of initiatives that experiment with health
IT in clinical settings, including the expanded
potential for open source electronic health record
systems that will complement private sector
proprietary systems. These initiatives offer an
important opportunity for capturing best practices
and applying them to the wider health care system.
The federal government will monitor and study such
efforts around the country and seek to expand on
already-successful programs.
OBJECTIVE D
Support new approaches to t
he use of
health IT in research, public and
population health, and national health
security
Strategy II.D.1: Establish new approaches
to and identify ways health IT can support
national prevention, health promotion,
public health, and national health security.
The Affordable Care Act included significant
resources for improving public health and
prevention. These new strategies will influence the
way public health is administered across the country
and health IT will be a fundamental part of that
change. Public health IT infrastructure investments,
such as those discussed in Strategy II.D.2 below, will
be updated and aligned with these approaches to
public and population health.
The Prevention and Public Health Fund has
supported a new program entitled Strengthening
Public Health Infrastructure for Improved Health
Outcomes, to increase the performance management
capacity of public health departments and ensure
that public health goals are being met. Health IT and
communications infrastructure is one of the four
areas of improvement sought through the program.
In FY 2010, CDC awarded a total of $42.5 million to
Federal Health IT Strategic Plan 26
projects at state and local public health
departments.
x
Health IT is critical in supporting new approaches to
national health security. The use of health IT during
a public health emergency can facilitate continuity of
care for the impacted population by enabling
electronic health information to flow for emergency
care. In the event of a natural disaster, having health
records in an electronic form can help avoid the
impact of destroyed paper records and ensure that
the affected population’s health information can be
accessed in the event of displacement.
Strategy II.D.2: Invest in health IT
infrastructure to support the National
Prevention and Health Promotion Strategy.
CDC, in collaboration with public health agencies at
the federal, state, and local levels, will invest in
public health IT infrastructure to improve a number
of the public health agencies’ core capacities. These
capacities include:
Anticipating, preventing, and responding to health
threats, reportable diseases, and adverse
population events
Identifying populations with specific health care
needs (e.g. at risk populations, children, etc.) and
promoting their adherence to public health
guidelines
Preparing for and responding to emergencies
Communicating with consumers and encouraging
their participation in public health
For instance, CDC programs support information
exchange across jurisdictional boundaries by
integrating with the Nationwide Health Information
Network, and provide agencies with common tools
for disease detection, monitoring, and real-time
situational awareness. The National Electronic
Disease Surveillance System (NEDSS) advances the
transition to standards-based electronic data
exchange for reportable disease surveillance,
improving agencies’ capabilities in detecting and
responding to reportable diseases. The National
Environmental Public Health Tracking Network
melds data from environmental hazard monitoring
and human exposure and health effect surveillance
into a network of standardized electronic data
systems. Continued investments in these and other
programs will support the National Prevention and
Health Promotion Strategy.
Strategy II.D.3: Ensure a mechanism for
information exchange in support of research
and the translation of research findings
back into clinical practice.
In order to support information exchange vital for
research, information in an EHR, with the
appropriate privacy protections, should be accessible
by researchers, research systems, biorepositories,
registries, and other types of research databases. In
turn, adopted health IT interoperability standards
should be used in research studies – and enhanced to
cover unique research needs – in order to facilitate
both the use of health care data in research and the
translation of research results into clinical practice.
This two-way interaction between research and
clinical care, facilitated by health IT, has the potential
to accelerate the generation of important new
information on medical interventions, personalized
treatments and public health initiatives utilizing
population-based knowledge as well as the
development of new tools for medicine, such as
computerized decision support systems. For
example, the Electronic Medical Records and
Genomics (eMERGE) Network has developed and
applied approaches to research that combine DNA
biorepositories with EHR systems for large-scale,
high-throughput genetic research such as genome-
wide association studies on a variety of diseases. The
consortia, like the NIH-supported Clinical and
Translational Science Award (CTSA) programs, are
maximizing the ability of researchers to leverage the
wealth of existing data to strengthen knowledge
building and evidence creation, and ultimately
improve clinical and preventive care through a more
rapid progression of knowledge from the laboratory
to clinical care implementation. Another example is
The Cancer Biomedical Informatics Grid (caBIG),
an information network sponsored by the National
Cancer Institute (NCI), which provides tools, data,
and services to enable researchers, providers, and
Federal Health IT Strategic Plan 27
patients throughout the oncology community to
collaborate and share expertise and data.
Meaningful use of certified EHR technology in
clinical research presents an opportunity to use data
collected through routine operations in a clinical
practice to generate and test hypotheses about the
relationships among patients, diseases, therapies,
prevention, treatment and recovery, and clinical
outcomes. It can improve the understanding of the
correlations between genotypes and phenotypes and
genomic and epigenetic interactions and
interrelationships, improve the identification and
tracking of medical events such as epidemics and
adverse events related to treatment, and facilitate
surveys of the health of the public at speeds
approaching real time. Data from EHRs are crucial
for patient-centered research and can provide
insights for researchers and benefits for patients and
providers in terms of improved care and
personalized treatments. These efforts will be
consistent with the privacy and security activities
outlined in Goal III of this Plan. Using EHRs may
eliminate redundant data entry, thus improving data
quality and processing speed; may stimulate a
learning health system in which the translation of
research findings into clinical care supports continual
improvement in knowledge, treatment and health;
and may increase opportunities for patients to
participate in research, particularly in underserved
communities and public health settings.
The efficient collection and exchange of EHR data
for research purposes, coupled with the use of
applicable EHR interoperability standards in
research studies, would also ensure that key findings
that lead to improvements in population and
individual health are rapidly translated back into
clinical practice. This will help to create the learning
health system envisioned in Goal V of this Plan.
Federal Health IT Strategic Plan 28
Goal III: Inspire Confidence and Trust in Health IT
rotecting the privacy and security of health
care information, and ensuring the safe use
of health technology, have long been core
responsibilities of the government. These
responsibilities have needed to evolve constantly
with the development of new technologies and the
adoption of new health care practices. Health IT –
with its potentially dramatic impact on the practice
of medicine – requires the government to further
evaluate and update policies and programs in privacy
and security areas over the next five years. In
evaluating and updating its policies and programs,
the government will rely on the Fair Information
Practice Principles
xi
and the Nationwide Privacy and
Security Framework for Electronic Exchange of Individually
Identifiable Health Information
.
xii
EHRs and other health IT will enhance the quality
and value of health care, but only if there are
appropriate protections in place to keep health
information private and secure. Privacy and security
are the bedrock of building trust, a must-have
component that is essential to achieving meaningful
use and realizing the value of health IT. Patients and
providers must feel confident that laws, policies, and
processes are in place to keep their health
information private and secure, and that they will be
enforced when violations occur.
To that end, the HHS Office for Civil Rights (OCR)
is fulfilling new obligations under the HITECH Act
to modify the Privacy and Security Rules under the
Health Insurance Portability and Accountability Act
of 1996 (HIPAA) to strengthen the privacy and
security protections for health information and the
enforcement of and penalties for violating the
HIPAA rules.
These added privacy and security protections are an
integral piece of the government’s increased efforts
to broaden the use of IT in health care. ONC is also
exploring areas beyond HIPAA that are necessary to
ensure trust in widespread health information
exchange, including governance of the Nationwide
Health Information Network. Through the health IT
certification program and ONC’s partnership with
other federal entities, ONC is working to enhance
privacy and security features in EHRs and to work
with HITECH grantees to make sure appropriate
privacy and security strategies are in place.
ONC is collaborating with OCR on a
comprehensive communications plan to reach out to
providers, consumers, and other stakeholders to
educate and inform them of the importance of
health IT security and ways they can help to keep
protected health information secure.
In addition to added privacy and security
protections, ONC and OCR recognize the
importance of increasing efforts to inform
individuals and providers of patients’ rights with
regard to their protected health information and to
increase public transparency regarding the potential
uses of protected health information. Individuals
must understand their rights, be aware of the federal
government’s efforts to protect those rights, and be
notified of any breaches of unsecured protected
health information that occur.
In addition to the HIPAA Privacy and Security
Rules, which provide a set of national standards for
the protection of certain health information, other
federal laws afford additional protections for
information which may be particularly sensitive, such
as that related to individuals who are treated for
alcohol and/or drug abuse. SAMHSA, working with
ONC and OCR will address issues of behavioral
health privacy and confidentiality in the health IT
environment.
EHRs and other health IT offer tremendous
potential to improve patient safety and to help health
care providers practice safer and more effective care.
ONC took a key first step toward thoroughly
assessing health IT patient safety concerns through
the commission of a report by the Institute of
Medicine (IOM). In addition, ONC is engaged in an
ongoing effort to disseminate best practice resources
to providers to help equip them with the latest
information, so as to avoid common challenges to
safe and effective implementation and use of EHRs
and other health IT.
P
Federal Health IT Strategic Plan 29
The government’s objectives to “Inspire Confidence
and Trust in Health IT” are:
A. Protect confidentiality, integrity, and availability
of health information
B. Inform individuals of their rights and
increase transparency regarding the uses of
protected health information
C. Improve safety and effectiveness of health
IT
Spotlight on Health Outcomes
Use of health IT can enhance patient trust and care management
These “Spotlight on Health Outcomes” are intended to highlight exemplary ways that widespread adoption and use of health IT and electronic health
information exchange could help transform and improve health care. Some of these examples are only aspirational today or only exist in select
communities or health systems. However, these examples illustrate the type of transformed health care that could be possible with the achievement of
the goals of this Plan.
Three years ago, George’s PCP’s practice was flooded during
a hurricane. Fortunately, George’s provider had an EHR
system that backed up all of George’s medical information on
a remote, secure server. When George was displaced after the
storm, his new PCP was able to retrieve his entire medical
record, rather than George having to reconstruct his medical
history from memory. George’s provider was able to see
what medications, allergies, coexisting conditions, and risks
she must manage to ensure that George’s care is continued.
When Jane has concerns about her ability to manage her
COPD and especially when she is concerned about
developing an infection, she is able to exchange secure
messages with her PCP to get feedback without requiring a
trip to the provider’s office. When Jane describes to her
provider some early warning signs of an infection, her
provider electronically prescribes antibiotics that she is able
to take immediately to stem the possibility of an infection.
Jane enjoys being able to log into her online portal and show
her children that she is indeed managing her blood pressure
well and can answer their questions regarding what
medications she is taking and her latest lab test results. Jane’s
PCP is able to proactively address Jane’s questions about the
correct dosage of her medications in real time and without
the added delay of having to wait until her next appointment.

Federal Health IT Strategic Plan 30
OBJECTIVE A
Protect confidentiality, integrity, and
ava
ilability of health information
Strategy III.A.1: Promulgate appropriate
and enforceable federal policies to protect
the privacy and security of health
information.
It is HHS’ policy that the privacy and security of
individually identifiable health information should be
protected wherever it is electronically transmitted,
maintained, or received. While the HIPAA Privacy
and Security Rules are key safeguards, they are not
the only means available for affording this
protection. HHS will work with other federal
agencies, states and other stakeholders to ensure that
appropriate policies are in place.
The means for collecting, managing, storing, and
transmitting electronic health information are rapidly
advancing. ONC, along with its federal partners, will
strive to ensure that federal privacy and security
policies, including regulations and guidance, keep
pace with this evolving field.
As a first step, OCR is crafting rules to implement
the modifications to the HIPAA Privacy and
Security Rules as required by the HITECH Act.
Among other changes, these rules will:
Impose direct liability on business associates for
compliance with certain provisions of the HIPAA
Privacy and Security Rules
Establish new restrictions on the sale of protected
health information
Establish stronger restrictions on disclosing health
information for marketing and fundraising
purposes
Provide increased transparency regarding how
health information is shared
Strengthen individuals’ rights to access their health
information electronically
OCR has also issued rules required by the HITECH
Act that specify the conditions under which covered
entities must notify individuals, HHS, and in some
cases the media, of breaches of unsecured protected
health information.
HHS has commenced the process of exploring
broader privacy and security policies that may be
necessary to ensure trust in electronic health
information exchange. In exploring these topics,
ONC will be guided by the Nationwide Privacy and
Security Framework for Electronic Exchange of Individually
Identifiable Health Information, a set of privacy and
security principles grounded in the fair information
practice principles (FIPPs) released in 2008. The
process of updating HHS’s approach to privacy and
security policies begins with input from ONC’s
federal advisory committees – the HIT Policy
Committee and HIT Standards Committee – which
identify, assess and recommend solutions to evolving
privacy and security issues. These recommendations
are considered by ONC in light of other policies and
activities and are brought by ONC to an HHS Inter-
Division Task Force that is charged with establishing
policy direction in this area. ONC then gathers
broader Federal feedback through the Federal
Health IT Task Force. The goal is to resolve federal
policy direction on this first set of privacy and
security issues by the end of 2011.
HHS will address, at a minimum, the following key
policy areas:
Individual choice to participate in health
information exchange
Access limitations and transparency for electronic
health information exchange
Security, including provider and patient
authentication and de-identification of personal
health information
Integrity of health information
Secondary uses of health information for the
purposes of quality improvement, public health,
and research
In consultation with the Federal Trade
Commission (FTC), potential regulation models
with respect to personal health records (PHRs)
There are a number of potential levers for instituting
any new privacy and security policies that develop
Federal Health IT Strategic Plan 31
out of this process, including formal rulemaking
where authorized, which would provide the
opportunity for public comment. It is expected that
privacy and security will be components of ONC’s
anticipated regulations to establish a governance
mechanism for the Nationwide Health Information
Network. Concerns with exchanging digital
information over the Internet are not confined to
the health care sphere. ONC is collaborating with
other federal agencies to learn from and implement
consistent approaches to privacy and security. For
example, ONC is working with the Presidential
workgroup formulating the National Strategy for
Trusted Identities in Cyberspace. In addition, as a
participant in the National Science and Technology
Committee’s Subcommittee on Privacy and Internet
Policy, ONC is working with other agencies to
address privacy issues arising from the evolving
means of collecting and analyzing data, including
health information, as it flows over the Internet.
Strategy III.A.2: Enforce existing federal
privacy and security laws and maintain
consistency with federal policy.
In order for providers and patients to have trust in
health IT and information exchange, they must be
confident that privacy and security laws are in place
and will be enforced. OCR is charged with civil
enforcement of the HIPAA Privacy, Security, and
Breach Notification Rules, the primary federal
regulations protecting health information. The
HITECH Act strengthens OCR’s civil enforcement
of the HIPAA Rules by establishing four categories
of violations that reflect increasing levels of
culpability; four corresponding tiers of penalty
amounts that significantly increase the minimum
penalty amount for each violation; and a maximum
penalty amount of $1.5 million for all violations of
an identical provision during a calendar year. OCR
also plans to conduct periodic audits that will assess
covered entities’ and business associates’ compliance
with the HIPAA Privacy and Security Rules. OCR
will employ all of its enforcement tools – including
imposing the increased penalty amounts for HIPAA
violations, conducting compliance reviews, entering
resolution agreements that are satisfactory to HHS
for informally resolving indications of
noncompliance, and conducting periodic audits – to
improve compliance with the Privacy and Security
Rules.
Strategy III.A.3: Encourage the
incorporation of privacy and security
functionality into health IT.
The use of appropriate technology can greatly
enhance the privacy and security of health
information. ONC, working with NIST and other
federal partners, will encourage the incorporation of
privacy and security functions into EHRs and other
health IT. ONC and OCR seek to ensure that
certified EHRs facilitate health care providers’
compliance with the requirements of the HIPAA
Security Rule. ONC’s Final Rule on Standards and
Certification Criteria for EHRs, issued in
conjunction with the Medicare and Medicaid EHR
Incentive Programs’ stage one meaningful use
requirements, requires that certified EHRs be
capable of:
Encrypting health information to keep it secure
Establishing access controls that permit only
authorized users to access the system
Generating audit logs to record certain actions
related to electronic health information
Automatically logging off a user after a set time of
inactivity
O
NC will continue to identify additional security
features that may be incorporated into EHR
certification and standards in future stages of
meaningful use.
Strategy III.A.4: Assess technical solutions
that could support more granular patient
choice and data segmentation.
Some individuals may want to give consent for
some, but not all, of their personal health
information to be exchanged (often called “data
segmentation”). For example, an individual may not
want information about his/her substance abuse
treatment shared, but may still want to take
advantage of the benefits of sharing the remainder of
his/her health information electronically. Today,
many EHR systems do not have the capability to
Federal Health IT Strategic Plan 32
support more granular patient consent and data
segmentation. In accordance with the HITECH
Act, ONC is investigating, through research and
potential demonstration projects, innovative means
for protecting the privacy of health information,
such as data segmentation and consent management
tools. ONC will work closely with its SHARP
grantee that is conducting research in this area.
In addition, ONC and SAMHSA are pilot testing the
development of service specifications and reference
models that can segment personal, electronic health
care records into more or less sensitive parts and
share sensitive parts only with appropriate
authorization. This pilot will be broadly applicable,
but particularly useful in the context of exchanging
behavioral health information.
Strategy III.A.5: Identify health IT system
security vulnerabilities and develop strategic
solutions.
ONC will conduct analysis and research to identify
the security vulnerabilities of existing and emerging
health IT systems in order to identify where to best
target its resources. As part of this effort, ONC will
analyze health information breaches that are
reported to HHS in order to identify the most likely
sources of vulnerability. In addition, ONC will
participate in the President’s cybersecurity initiative
and work with other federal partners, including the
Federal CIO Council, to identify large-scale security
threats and to develop strategic solutions. ONC will
also conduct research to identify best practices for
ensuring electronic health information remains
available in the event of a system failure, cyber-
attack, or other emergency event.
ONC is aware of the potential for the use of EHRs
to facilitate fraud and will consider how to address
the potential for fraud through its existing policies
and programs. For example, ONC, following the
leadership of the White House, is developing a
national framework for high assurance physician
identity management. The framework is intended to
provide a simple but highly trustworthy means of
assuring that physicians are who they claim to be in
health information exchange. This framework, which
will be piloted by key federal stakeholders such as
CMS and VA, should have a major impact on
reducing medical identity theft and fraud. In
addition, ONC will support the efforts of other
federal agencies, including CMS and OIG, to explore
a variety of options to improve efforts to combat
fraud.
Strategy III.A.6: Identify health IT privacy
and security requirements and best
practices, and communicate them through
health IT programs.
ONC, OCR, and SAMHSA will seek to ensure that
privacy and security policies and recommended best
practices remain aligned with advancements in
technology. Privacy and security requirements and
priorities will be identified based on analyses of
security incidents and vulnerabilities, and best
practices will be developed and disseminated. Where
necessary, OCR will update guidance to reflect
evolving privacy and security threats, for example
the 2006 guidance on securing remote and mobile
access, which has its basis in OMB memorandum
M-06-16. ONC will work with OCR and SAMHSA
to develop educational and guidance materials on
privacy and security best practices for organizations
implementing health IT. OCR will continue to issue
guidance on complying with the HIPAA Privacy and
Security Rules, and SAMHSA will continue to issue
guidance on complying with 42 CFR Part 2.
Additionally, State HIE Cooperative Agreements,
Beacon Communities grants, and SHARP grants will
demonstrate how privacy and security best practices
can be identified, implemented, and brought to scale.
Similarly, information on these privacy and security
requirements and best practices will be channeled
through the HITRC and the RECs, which offer
opportunities to disseminate best practices to
providers working to achieve meaningful use.
Some stakeholders have identified the variance in
state health privacy laws as an impediment to
exchanging health information among states. ONC
will work with state governments and State HIE
grantees to identify and develop best practices to
exchange health information electronically among
states with varying privacy laws. In addition, ONC is
exploring technology solutions to aid
implementation in a computable format of patient

Federal Health IT Strategic Plan 33
consent and to enable information exchange among
states.
State HIE grantees are required to incorporate
privacy and security strategies into their
implementation plans. ONC will work with the
grantees to ensure that these privacy and security
strategies are strong as part of its evaluation of the
states’ overall implementation plans. This work will
be further informed by VA and DoD’s experience
with the VLER program, that facilitates information
exchange of a Veteran’s health record among
different systems and states that may have differing
privacy laws.
Privacy and security are key components in ONC’s
workforce education program as well as the materials
being produced by the workforce curriculum
development centers. ONC will review and evaluate
these materials to help ensure that future health IT
professionals are well educated on privacy and
security requirements and best practices to ensure
compliance with these policies.
OBJECTIVE B
Inform individuals of t
heir rights and
increase transparency regarding the
uses of protected health information
Strategy III.B.1: Inform individuals about
their privacy and security rights and how
their information may be used and shared.
As part of its health IT education and outreach
strategy, HHS will inform providers and individuals
about the privacy and security rights and protections
that are in place to safeguard their electronic health
information. See Strategies I.A.6 and IV.A.2 for a
more detailed discussion of this strategy. To support
the goals of the HITECH Act (Sec. 13403(b),
Education on Health Information Privacy), OCR
and ONC are working in partnership to execute this
education and outreach strategy over a two-year
period in order to inform individuals about how
their information is safeguarded, how their
information may be used and shared, and how
individuals can exercise their rights under the
HIPAA Privacy Rule. This education and outreach
will also inform individuals about best practices that
they can use to protect the privacy of health data
they generate or maintain in consumer health IT
tools. In order to accommodate the needs of non-
English speaking individuals, these campaign
materials will be available in multiple languages.
In an effort to help individuals easily access
information about existing HHS privacy efforts
and the policies supporting them, HHS launched
an online resource center. The site provides
transparency about HHS policies on the
collection, use, and exchange of personally
identifiable health information, and the privacy
and security requirements for entities that collect
and maintain health information.
Strategy III.B.2: Increase transparency
regarding the development of policies and
standards related to uses and sharing of
protected health information.
ONC will engage with a wide range of consumer
organizations and diverse communities in an effort
to increase transparency of privacy and security
issues and to develop policies and standards to
address the consumer organizations and diverse
communities’ interests. The HIT Policy Committee
and the HIT Standards Committee each have a
Privacy and Security Workgroup that holds public
meetings and makes recommendations to its parent
federal advisory committee (FACA) related to
privacy and security requirements, which in turn
considers the workgroup’s advice and may submit
related recommendations to the National
Coordinator. To date, these federal advisory
committees have made recommendations on various
privacy and security issues, including meaningful use
criteria, certification criteria, individual consent,
provider authentication, patient identification and
use of intermediaries or third party service providers
in arrangements to exchange individually identifiable
health information. The Committees will explore
new issues as they arise. ONC will actively seek
public input into the development of these policies
and standards through its federal advisory
committees.

Federal Health IT Strategic Plan 34
Strategy III.B.3: Maintain strong breach
notification requirements.
To maintain consumer trust in EHRs and other
health IT, individuals must be adequately informed
of the use and sharing of their health information
and appropriately notified when their personal health
information has been compromised. OCR has
issued an interim final regulation on breach
notification that improves transparency and acts as
an incentive to the health care industry to improve
privacy and security by requiring HIPAA-covered
entities to promptly notify affected individuals, the
HHS Secretary, and, in some cases, the media, of a
breach of unsecured protected health information, as
well as requiring business associates to notify
covered entities of a breach of unsecured protected
health information. OCR is in the process of issuing
a final breach notification regulation that responds
to comments on the interim final breach notification
rule. Similar breach notification provisions
implemented and enforced by the FTC apply to
non-HIPAA covered entities, such as vendors of
certain PHRs and their third party service providers.
OBJECTIVE C
Improve safety and effectiveness of
he
alth IT
Strategy III.C.1: Provide implementation
and best practice tools for the effective use
of health IT.
AHRQ’s Health IT Portfolio supports health
services research grants and contracts that create
new knowledge, synthesize and disseminate best
evidence and provide tools for implementation
addressing health IT’s impact on the quality of
health care. Current initiatives address clinical
decision support, patient safety, patient centered
care, quality measurement, and usability and
workflow issues. In addition, ONC is actively
working to make resources available to providers
that allow them to maximize the value of using
health IT by avoiding common challenges and legal
issues associated with adoption, implementation, and
use of EHRs and other health IT. Professional
societies, licensing boards, and continuing education
programs are developing best practice resources
related to issues such as workflow redesign, the need
for ongoing maintenance and upgrades, and legal
concerns related to vendor contract clauses. There
are important legal issues that providers should be
aware of when entering into agreements with EHR
and other health IT vendors. ONC will work to
equip providers with information and help address
potential barriers they may face in achieving
meaningful use, including improved usability of
EHR technology (see Strategy I.A.9). ONC and RECs
will ensure that appropriate best practice resources
about these issues are distributed to the providers
that need them.
Strategy III.C.2: Evaluate safety concerns
and update approach to health IT safety.
ONC has commissioned the Institute of Medicine
(IOM) to conduct a formal study of health IT
patient safety concerns and to recommend additional
actions and strategies to address those concerns, as
well as to define the role of public and private
sectors in ensuring safety of health IT-assisted health
care services.
Strategy III.C.3: Monitor patient safety
issues related to health IT and address
concerns.
While developing an updated overall approach to
health IT safety, HHS agencies are monitoring
patient safety issues and addressing immediate
concerns. ONC is exploring mechanisms to improve
data integrity, including an assessment of existing
and emerging technologies that may allow for
automated resolution of inaccurate or questionable
data in EHRs and PHRs.
AHRQ, in conjunction with FDA and ONC,
developed a new protocol for reporting patient
safety events involving HIT devices. This protocol
was developed as part of the AHRQ Common
Formats for reporting patient safety events and is
available on the AHRQ Web site. AHRQ and FDA
collaborated in order to harmonize HIT event
reporting not only with Common Formats for other
event types but also with FDA’s MedSun system for
reporting adverse events associated with devices. It
is the goal of AHRQ, FDA, and ONC that providers
Federal Health IT Strategic Plan 35
experiencing adverse events involving HIT will be
able to report such events once and have the
information flow to those interested in and
authorized to receive it, e.g., Patient Safety
Organizations, state reporting systems, accrediting
bodies, and the FDA. It is expected that by
providing standardized Formats for reporting HIT
events efficiently, information can be aggregated,
learning accelerated, and care made safer.
Federal Health IT Strategic Plan 36
Goal IV: Empower Individuals with Health IT to
Improve their Health and the Health Care System
ndividual participation is a critical, yet currently
underutilized, component in improving health
and the overall health care system. Health care,
which often means initiating medical solutions after
something has gone wrong, can only go so far in
improving health. Individuals’ behaviors, and the
ways in which communities foster healthy behaviors,
are much more powerful forces for improving
population health. But medical solutions, too, can
become more centered on the individual: by arming
people with knowledge and by giving them and their
loved ones greater control over their own care.
xiii
Health IT, which encompasses a broad category of
tools and services, is critical in both empowering
individuals to manage their health and shifting care
to be more patient-centered so patients can be more
active in health decisions and treatments. Existing
and emerging technologies allow data to flow
directly to and from the individual, wherever the
individual may be. As a result, patient interactions
with the health care system are no longer confined
by the walls of the clinical setting and may occur
frequently in between visits. PHRs allow patients to
capture their own health observations and in some
instances, to access their health information from
providers. Mobile phones with glucometers allow
individuals to track their blood sugar levels through
their mobile devices. Mobile phones and related
applications are also being used to send reminders to
take medications or to send free health tips to help
during a pregnancy. In mental health, mobile apps
are being utilized to track moods and provide
therapeutic interventions with personalized
messages, exercises, and coaching. Using these tools
and others, individuals can become more attuned to
healthy behaviors, monitor their health, make
informed personal health decisions, and receive
preventative care. Patients managing illnesses or
other ailments can use health IT to connect with
other patients that share a similar condition, keep
better track of their health care, receive health care
solutions remotely, and participate in their care
coordination.
However, only 7 percent of Americans have used a
web site to access their health information online.
xiv
For individuals to become empowered they need to
be included in the policymaking process. This means
both understanding the government’s approach to
health IT and being able to shape the direction of
policies and programs. An HHS-led health IT
education and outreach strategy will seek to engage
the public in dialogue about health IT and provide
an opportunity to shape its future and the public’s
own expectations.
Even fewer have used mobile health (mHealth)
applications and remote monitoring technologies.
These low rates are the result of multiple dynamics:
most consumers are not aware of nor able to afford
the technologies, do not have access to their health
information, or do not expect to take as active a role
in their health and health care as they might in other
aspects of their lives. As a result, they have not
created a robust marketplace for technology
innovation. To truly empower consumers and move
the health care system to become more patient-
centered, the government will need to help change
these dynamics.
The single biggest lever to individual empowerment
is access to data. Individual access to data can
augment and improve patient-provider
communications. It is not meant to replace this
relationship, but rather to enhance it. Such data
liquidity will make health IT meaningful for
individuals, promote technological innovation, move
care to center more on the individual, and ultimately
have a direct effect on population health. Right now,
there are too many barriers to individual and
caregiver access to personal health care information.
Engaging individuals with health data is a top
priority of the Medicare and Medicaid EHR
Incentive Programs. Other policies and regulations,
such as the HIPAA Privacy Rule, will work in
concert with meaningful use efforts to facilitate
improved individual access to data. And the
government intends to continue to develop tools
I
Federal Health IT Strategic Plan 37
and serve as a model for exchanging data with
individuals, as reflected in the Blue Button initiative
at VA, DoD and CMS (see strategy IV.B.2 below for
more information).
Consumer health IT is an emerging industry – it is
new, fast-growing, and on the cutting edge of
technology innovation. While the government will
not lead the innovation that is likely to take place
over the next five years – that is the role of the
private sector – it will remain an active partner to
address a number of key steps to collaborate with
the industry and foster health IT research and
innovation. If the government makes more of the
data it collects available—as well as encouraging
others to do the same--technology companies can
develop applications and business models that make
the information relevant and marketable to
individuals. NIH and other government institutions
directly fund research and development. HHS
launches contests and challenge grants to focus
innovation on specific areas that will benefit health
care and the public good. These strategies to
promote health IT innovation are discussed in more
detail in Goal V Objective B, “Broaden the capacity
of health IT through innovation and research.”
As consumer technologies evolve and become more
prevalent, and as individuals grow more accustomed
to interacting with their health information using
health IT, there will be a need to better integrate
clinical practices with individual use of health IT
outside of the care environment. Through ONC’s
EHR certification program, the government will
facilitate the creation of clinical EHR systems that
can accept information from consumer applications.
The government will also help clinicians empower
individuals with technology, and will encourage
clinical practices to take advantage of consumer-
generated health information, both of which are
steps in achieving the ultimate aim of moving to
more patient-centric care.
The government’s objectives to “Empower
Individuals with Health IT to Improve their Health
and the Health Care System” are:
A. Engage individuals with health IT
B. Accelerate individual and caregiver access to their
electronic health information in a format they can
use and reuse
C. Integrate patient-generated health information
and consumer health IT with clinical applications
to support patient-centered care
Federal Health IT Strategic Plan 38
Spotlight on Health Outcomes
Empowering patients with health IT can improve care management and quality of life
These “Spotlight on Health Outcomes” are intended to highlight exemplary ways that widespread adoption and use of health IT and electronic health
information exchange could help transform and improve health care. Some of these examples are only aspirational today or only exist in select
communities or health systems. However, these examples illustrate the type of transformed health care that could be possible with the achievement of the
goals of this Plan.
The ability to easily access health information electronically
has spurred innovation in the development of mobile
technology applications and other tools that can help patients
better manage chronic diseases and stay healthy. After
George is diagnosed with chronic heart failure, he and his
PCP decide to use a new mobile health device to help him
track his health status. Using sensors and an easy-to-use
interface on his Smartphone, the device records his exercise
patterns, heart rate, weight and diet. This information is
uploaded to an online site where George sets goals, tracks
progress, and engages in contests with other individuals
managing CHF. Periodically, over the course of a year,
George notices abnormalities in his trends and logs onto his
personal health portal: a site where his personal health
information is stored and both he and his provider have
access to this electronic health information. There he uploads
data from his mobile app, and sends a secure email to his
provider to ask questions about what he is viewing in the
portal. Without having to wait until the next appointment,
the provider is able to tell George that everything looks fine
and to encourage him to keep up the good work. When
George does have his regular in-person visit a year later, his
blood pressure is under control at 128/88 and his LDL is 70.
These results, which George anticipated after noticing
positive trends in his data and feeling better, indicate a
significant improvement in George’s cardiovascular health
and a dramatic decrease in risk of a heart attack.
After her hospitalization, Jane’s family decides they would
like to take care of her at home and are equipped by the
hospital with a remote monitoring system. Remote
monitoring systems may reduce medical complications and
hospitalizations by giving providers more frequent data
readings on their patients. When used by homebound,
chronically ill patients, these systems could be linked to
EHRs to alert providers of a problem and allow the provider
to react more quickly to adjust a medication or troubleshoot
the problem. Jane’s particular device allows her to do weekly
remote visits with a nurse, instead of returning to a medical
facility for these visits. The nurse is able to take readings on
Jane’s blood pressure, glucose levels, and weight, while
interacting with her over video conference to check in on
symptoms and see how Jane is doing with her medications.
Using this device, the nurse is able to answer Jane’s questions
without needing an in-person office visit, and to identify
major problems before they require an emergency room visit.
Jane’s quality of life is greatly improved, and she has been
able to reduce the number of times she and her family have
needed to go to the hospital and spend time in waiting
rooms. These remote monitoring systems have also enabled
Jane from needing to live in an assisted living environment.
Federal Health IT Strategic Plan 39
OBJECTIVE A
Engage individuals with health IT
Strategy IV.A.1: Listen to individuals and
implement health IT policies and programs
to meet their priorities.
The benefits of health IT can only be realized if
individuals are fully involved in the development of
health IT policy and confident that electronic health
information is kept private and secure. When
including individuals in the health IT policymaking
process, the government cannot expect them to
come to Washington, D.C. or to seek out rulemaking
processes. To truly be representative, ONC will seek
to participate in on-going public conversations about
health IT. These conversations are already taking
place, whether it is in online forums serving specific
demographics, community-based faith groups, or
chronic disease advocacy groups. ONC will
participate in these public dialogues with the aim of
learning how health IT policy and programs can
support individual empowerment.
These efforts will be complemented by the primary
formal mechanism established by the HITECH Act
for public input into health IT policy: the federal
advisory committees. As mentioned previously, there
are two committees – the HIT Policy Committee
(HITPC) and the HIT Standards Committee
(HITSC) – and several “sub-committees,” or
workgroups. The HITPC and HITSC make
recommendations to the National Coordinator on
crucial policy and program decisions on an ongoing
basis. While individuals and consumer advocates
have been represented on some of the Committees
already, the federal government will strengthen that
representation going forward.
ONC will also reach out to consumer organizations
directly, both to engage them in its own work and to
encourage them to reach out to their constituents in
the context of their own efforts as well.
Strategy IV.A.2: Communicate with
individuals openly and spread messages
through existing communication networks
and dialogues
.
The HHS-led education and outreach strategy
discussed in strategies I.A.6 and III.B.1 will engage
consumers as an important audience. Education and
outreach efforts will be aimed at helping people
understand the transition to EHRs, the value of
health IT more broadly and how health IT can be
leveraged to make informed choices and support
behavioral change related to their physical and
behavioral health and care. In order to effectively
reach millions of Americans, HHS intends to
collaborate whenever possible with communication
networks that already exist (such as health care
advocacy groups, faith-based groups, groups aimed
at supporting specific demographics, etc.) and to
take advantage of social media (such as blogs and
online social forums).
ONC has already reached out to numerous
consumer organizations, including those
representing individuals with disabilities, non-
English speaking populations, and people with lower
literacy levels, to involve them in discussions to
shape ONC’s programs and activities.
OBJECTIVE B
Accelerate individual and caregiver
access to their electronic health
information in a format they can use
and reuse
Strategy IV.B.1: Through Medicare and
Medicaid EHR Incentive Programs,
encourage providers to give patients access
to their health information in an electronic
format.
A primary barrier to individual access to information
is the lack of a business case for providers to share
that information. Providers record and store patient
health data in a health record; for them to also share
that information with patients has historically caused
additional administrative burden and cost. While
individuals have a right to access their health
information under the HIPAA Privacy Rule, there
has been little financial incentive for providers to
proactively share a copy of the medical record with
the patient or to minimize the burden for the patient
Federal Health IT Strategic Plan 40
to obtain a copy of the medical record. EHRs,
however, reduce this additional burden and
meaningful use incentive payments help make a
business case for doing so. The first stage of
meaningful use requires providers to send patients a
clinical summary of each office visit and an
electronic copy of their health information within
three days of their request, and includes a menu set
item to identify and provide patient-specific
education resources to patients. We expect that
future stages of meaningful use will build on these
requirements.
ONC is exploring ways to encourage EHR vendors
to add features that would allow patients to access
and download their health information through
consumer e-health tools, such as PHRs and secure
mHealth application on smart phones and other
mobile devices. It is important that personal health
data be not only downloadable, but also available in
a format that can be re-used by other applications
and support interactions between EHRs and external
sources of patient-specific education resources, such
as those available through NIH/NLM’s MedlinePlus
Connect interface.
Strategy IV.B.2: Through federal agencies
that deliver or pay for health care, act as a
model for sharing information with
individuals and make available tools to
do so.
Beyond simple access, better tools and processes are
necessary to make information more useful to
individuals and their caregivers. The government will
be a leader in providing information to individuals.
For example, the Blue Button is a web-based feature
through which patients may easily download a copy
of their health information and share it with health
care providers, caregivers, and others they trust. This
feature is available on the DoD, VA, and CMS
websites for their respective beneficiaries to use.
This model is a key step forward in privately and
securely sharing information with individuals, which
will be enhanced over time. Using the Blue Button in
combination with PHRs and other consumer health
IT, individuals will be able to collect, aggregate, and
analyze their health care information. Over the next
five years, the government will consider more
advanced features of health information sharing with
individuals, including data subscriptions,
standardized code sets, standards for consumer
health IT applications, and applications that enable
information to be exchanged through mobile
devices.
The Nationwide Health Information Network has
already demonstrated sharing of patient-health
information between the VA, DoD, SSA, and many
private sector partners. Extending the Nationwide
Health Information Network specifications with
additional building blocks such as the Direct
specifications will include protocols for provider-
patient secure messaging, which is a major step
towards patient-centered care.
The Federal Health IT Taskforce has recognized
individual access to data as a primary objective. As
done with the Blue Button initiative, it will continue
to seek ways to align government investments with
methods for giving individuals useful and reusable
copies of their own data.
Strategy IV.B.3: Establish public policies
that foster individual and caregiver access to
their health information while protecting
privacy and security.
While the Medicare and Medicaid EHR Incentive
Programs provide incentives for individual and
caregiver access to health information, there remain
policy opportunities and barriers that the
government will address outside of this program.
For instance, CMS and OCR are looking at ways to
enable individuals to request access to their test
results directly from laboratories. CMS has also
issued guidance to laboratories to clarify this issue.
OCR has proposed to revise the HIPAA regulations
such that a covered entity health plan would be
required to provide an enrollee access to the
enrollee’s electronic claims data in the electronic
form and format requested by the enrollee, if it is
readily producible in such form and format. These
policy issues may evolve over the next five years, but
HHS will support approaches that:
Feature a transparent, understandable, and easy to
use online process that enables consumers to
download and reuse their data

Federal Health IT Strategic Plan 41
Accommodate the range of user capabilities,
languages and access considerations, including
effective strategies for ensuring accessibility and
usability of electronic health information for
people with disabilities and meaningful access to
such information for individuals with limited
English proficiency
Provide strong privacy and security protections
Some of HHS’ priority policy work related to
individual access to information has been discussed
in Goal III, including: modifications to HIPAA as
stipulated in the HITECH Act, individual consent to
participate in health information exchange, and
authorization and authentication.
OBJECTIVE C
Integrate pa
tient-generated health
information and consumer health IT
with clinical applications to support
patient-centered care
Strategy IV.C.1: Support the development of
standards and tools that make EHR
technology capable of interacting with
consumer health IT and build these
requirements for the use of standards and
tools into EHR certification.
There are a number of compelling examples of
technologies that enable individuals to manage their
own health and care, and capture more complete
information about themselves. EHRs should be able
to interact with these devices, so that a provider can
access information that a patient using health IT
chooses to share with him or her. ONC, in
partnership with FDA and other federal agencies,
will promote standards to enable integration,
including standards for devices and EHR
interoperability, standards for data integration, such
as glucometer measurements and unique device
identifiers (UDI), for identifying the source of the
device generated data. Through the adoption of
certification criteria, ONC could encourage the use
of these standards and tools that may enable EHRs
to receive information from any consumer health IT
device that also uses similar standards and tools.
Strategy IV.C.2: Solicit and integrate
patient-generated health information into
EHRs and quality measurements.
There are two main types of patient-generated health
information - both of which could help achieve the
goal of improved care, improved population health,
and reduced per capita costs of health care:
1. “Patient-generated insights” are individual’s
observations and perceptions about their own
health or care. These observations of daily living
could come in the form of surveys, health journal
entries, online blog entries, or any number of
other media
2. “Device-generated data” is data captured by
medical devices or other consumer health IT.
W
hile we acknowledge there are policy questions
that need to be examined related to the integration
of patient-generated health information into EHRs,
this information can be valuable to providers in
adjusting treatment regimens, valuable to individuals
in understanding and improving their health choices,
and valuable to the health system in measuring and
rewarding for health care quality. As part of its
health care quality activities, HHS is studying
opportunities to encourage providers to solicit and
report patient-generated information on physical and
behavioral health. This includes ensuring that this
information could be captured and integrated into
EHRs as part of meaningful use, and exploring
standards and specifications that will enable that
integration.
Strategy IV.C.3: Encourage the use of
consumer health IT to move toward patient-
centered care.
Today, eighty percent of people on the Internet use
it to search for health information.
xv
Online
resources, including advice from peers, are a
significant source of health information. Many
people use the Internet to seek advice and to share
their experience, but far fewer have gone online to
review test results, used a PHR, or emailed their
doctor.
xvi
Consumers have expressed interest in the
use of health IT tools to make sure their health
record is correct, review test results, email providers,
Federal Health IT Strategic Plan 42
schedule appointments online, and refill
prescriptions online, all of which lend themselves to
more patient-centered care.
xvii
To further the use of consumer health IT, ONC and
CDC are working with two Beacon communities to
design tools that aim to help patients better manage
their diabetes. This program is modeled after
Text4Baby, a free text messaging service for
pregnant women and new moms that delivers timely
and practical tips customized for each stage of a
woman’s pregnancy or her baby’s age. Text4Baby is
the result of a public-private partnership with HHS,
the White House Office of Science and Technology
Policy and many private sector partners.
For care to truly become more patient-centered,
providers will need to adopt new processes and uses
of health IT that empower individuals in
understanding and directing their care. HHS’
primary approach to encouraging changes in
provider behavior is through the implementation of
quality measures and the attachment of incentives or
penalties to improving on these measures. To this
end, the National Quality Strategy, the National
Prevention and Health Promotion Strategy and the
Medicare and Medicaid EHR Incentive Programs
will work in concert to promote the integration of
consumer technologies and patient provided health
information into clinical workflows to improve
physical and behavioral health and care.
There are four domains of quality improvement that
can help lead to patient-centered care:
1. Self-management/activation refers to
measures of quality improvement that assess the
degree to which patients understand the role they
are meant to play in their care process, and the
degree to which patients have the knowledge,
skills, confidence, and self management
resources/support to move forward in this role.
2. Honoring patient preferences and shared
decision making refers to measures of quality
improvement that assess the degree to which
patients have the knowledge to make informed
decisions about their care. It also encompasses
measures that assess the quality of decision
making, patient connectedness to resources,
patient preferences, and care provider adherence
to patient preferences.
3. Patient health outcomes refers to measures of
quality improvement that assess the degree to
which the care provided affects disease/disability,
health risk, and functional health status at the
individual patient and population level.
4. Community resources coordination /
connection refers to measures of quality
improvement that assess if, and to what extent,
patients are connected to community resources.
C
ertain consumer health IT applications, when used
by consumers and providers in concert, enable
improvement in these domains. Future quality
measures and meaningful use requirements will help
to realize these benefits.
Federal Health IT Strategic Plan 43
Goal V: Achieve Rapid Learning and Technological
Advancement
eaningful use of certified EHR
technology will help the health care
system “catch up” with proven
technology and process changes that have been
available for years. Technology is not in stasis – it is
a dynamic industry prone to innovation which,
though at times disruptive, can yield enormous
benefits. There are two areas where the government
is working in concert with the framework of
meaningful use and the Affordable Care Act to
prepare for a future that is hard to predict:
1) enabling health IT innovation and research, and
2) leading the creation of a learning health system.
Health IT Innovation and Research
The future of health IT rests in innovation. The
government will embrace ongoing technology
advancements whether they are incremental or
fundamental. This means both adapting government
strategy to advances in technology, and continuing
to encourage rapid industry innovation.
Though there have been great leaps in health IT in
the past few years, the most remarkable gains are
likely still ahead of us. Possibilities include new ways
of engaging individuals with their health
information, new ways of aggregating and analyzing
data, new ways of connecting the clinical setting
more directly with individuals’ everyday lives, and
new ways of protecting privacy and ensuring the
security of health information. The government’s
first step to enabling innovation is liberating data
that is useful to consumers, providers, and
innovators. But the government will also invest
directly in research and development, use
government mechanisms as levers for fostering
adoption of innovative technology, and encourage
collaboration and targeted innovation in the health
IT industry.
The Learning Health System
A nation of providers who are meaningful users of
health IT will create very large amounts of clinical
information that is captured and stored in electronic,
computable form, and represented using defined
standards. Developing effective privacy policies and
technologies that can de-identify personally
identifiable health information will be challenging,
yet is essential to ensuring public trust and
safeguarding sensitive information. Through
carefully designed and trusted mechanisms, this data
will be able to flow securely from the system that
collected it to other systems, such as research
consortia, registries, and biorepositories, with an
authorized use for it. The secondary use and
population level analysis of this information holds
great promise for many forms of biomedical
research, public and population health, such as
tracking and management of epidemics, and
improving quality and efficiency of prevention and
care.
The government’s vision for realizing the value of
this information is a learning health system – an
environment where a vast array of health care data
can be appropriately aggregated and analyzed,
turning data into knowledge that can be put to
immediate use. A learning health system can shorten
the gap between the creation of new knowledge and
its widespread adoption in health care from the
often-quoted 17 years to 17 months, or even 17
weeks. Through a learning health system, the right
information will be available to support a given
decision, whether it is about the efficacy of a
treatment or medication for an individual patient,
predicting a national pandemic, or deciding whether
to proceed with the research and development for a
potential new treatment.
xviii
The learning health system will benefit from the
potential of Medicare and Medicaid EHR Incentive
Programs payments and payment reforms initiated
by the Affordable Care Act to motivate demand for
health care information, and to create the policies
and infrastructure for information exchange. The
government’s strategy to promote health
information exchange is described in Goal I, and
focuses on fostering exchange at the local level
M
Federal Health IT Strategic Plan 44
where there are existing business models for
information exchange. We expect future stages of
meaningful use to require more rigorous information
exchange requirements and will work in concert with
the Affordable Care Act to create demand for health
care information throughout the health care system.
Drivers for information exchange will be coupled
with federal leadership on national standards, privacy
and security requirements, and infrastructure that
supports information exchange.
The learning health system will use the policies,
requirements, and infrastructure created to support
meaningful use of certified EHRs, and will build on
them to support more sophisticated modes of
information exchange necessary for a system that
can “learn.” ONC commissioned the Institute of
Medicine (IOM) to convene national private and
public sector leaders in health care for a workshop
series on The Electronic Infrastructure to Support a
Learning Healthcare System. The report resulting from
these workshops series describes how lessons from
current smaller-scale examples of learning health
care systems, can be put into a policy framework that
could be implemented on a national scale.
xix
After soliciting input from the private sector, ONC
will work with federal partners to establish an initial
group to ascertain how to structure a learning health
system. Initial efforts will focus on creating a
federated model for the learning health system that
bridges disparate systems. Additional efforts will
focus on expanding the learning health system to
include additional public and private sector entities.
The government’s objectives to “Achieve Rapid
Learning and Technological Advancement” are:
A. Lead the creation of a learning health system to
support quality, research, and public and
population health
B. Broaden the capacity of health IT through
innovation and research
Spotlight on Health Outcomes
A learning health system can lead to earlier detection and better risk management
The use of health IT can enable a learning health
system to help prevent and monitor adverse events
caused by new drugs. As George begins therapy
using a new drug, information about his health can
be captured in the EHR and findings may be
automatically transmitted from the EHRs in which
they are collected and reported in aggregate via a
standard format to oversight agencies, such as the
FDA, or to the company which manufactures the
drug. By making this information available quickly in
the learning health system, population-level data
could be aggregated for earlier signaling of possible
adverse reactions to new drugs. If a potential adverse
reaction is identified, EHRs can serve another role in
helping providers to quickly identify each of their
patients taking a certain medication and notify the
patients via their preferred communication channel
about the potential risks.
These “Spotlight on Health Outcomes” are intended to highlight exemplary ways that widespread adoption and use of health IT and electronic health
information exchange could help transform and improve health care. Some of these examples are only aspirational today or only exist in select
communities or health systems. However, these examples illustrate the type of transformed health care that could be possible with the achievement of
the goals of this Plan.
The nationwide adoption and meaningful use of EHRs could
facilitate the collection of clinical and research data from disparate
sources including hospital systems, provider offices, laboratories,
biorepositories, registries, and other research databases. Some
stakeholders within the health care industry – such as researchers –
are currently on the cutting edge of analyzing EHR-generated data
to identify patient populations that are at-risk for preventable
hospitalizations. EHR-generated data combined with analytical
systems can be a boon to predictive modeling and knowledge
generation. As an elderly woman with multiple medical conditions,
Jane is part of an at-risk population. As these populations are
identified earlier and risk factors are better understood, the learning
health system could also enable resources, such as disease
management and case management, to be deployed earlier to help
avoid preventable hospitalizations.
Currently, good clinical
information regarding patient-centered outcomes on the best
treatment options for patients with multiple diagnoses is lacking.
In the long-term, EHR-generated data could be used to translate
research findings to better inform preventive approaches, establish
correlations, identify risks, and develop a deeper understanding of
disease in patients with multiple conditions.

Federal Health IT Strategic Plan 45
OBJECTIVE A
Lead the creation of a learning health
system to support quality, research,
and public and population health
Strategy V.A.1: Establish an initial group of
learning health system participants.
The learning health system’s success will depend in
part on the participation of a select number of
institutions that collect and use large amounts of
health care data. ONC recognizes this initial group
of participants is only a sub-set of a broader set of
activities occurring in the public and private sectors,
and plans to engage both sectors early in the process
and expand participation in the learning health
system over time (see Strategy V.A.4).
Several federal organizations are already fostering
learning health systems scaled to their own agencies,
and some of these agencies will be key initial
members of this group. The efforts of these agencies
provide a base of experience on which to build the
system at a larger scale. FDA’s Sentinel Initiative is a
national electronic system that is currently being
designed to enhance FDA’s ability to track the safety
of drugs, vaccines, biologics, and medical devices
after they reach the market. CDC’s programs are
supporting a national surveillance network through
which health care organizations, public health
entities, health information exchanges, and others
are able to contribute to the picture of the health of
the nation. Its goal is to be able to provide
nationwide and regional situational awareness for all-
hazard health-related threats and to support national,
state, and local responses to those threats. CDC also
has the National Environmental Public Health
Tracking Network, which integrates health,
exposure, and hazard data from a variety of national,
state, and local sources. It offers new understanding
of how hazardous substances can contribute to
illness and potentially be prevented.
Strategy V.A.2: Develop standards, policies,
and technologies to connect participants
within the learning health system.
In order to make the learning health system a reality
on a national scale, standards, policies, and mutually
reinforcing technologies must be put in place to
ensure that data collected at the point of care can be
de-identified, aggregated, queried and analyzed for
population health studies and quality improvement.
Data used in these studies must be represented
compatibly across participating organizations. Many
of these can be built upon already-existing standards,
policies, and technologies stemming from
meaningful use and the State HIE, Beacon
Community and SHARP grantees, but new
standards, policies and technologies will also be
needed.
To begin identifying specific standards, policies, and
technologies needed for the learning health system,
the Institute of Medicine (IOM) convened, with
ONC support, an Electronic Infrastructure to Support a
Learning Healthcare System workshop series in 2010.
The report stemming from the workshop series,
Digital Infrastructure for the Learning Health System: The
Foundation for Continuous Improvement in Health and
Health Care – Workshop Series Summary,
xx
takes lessons
from current examples of learning health care
systems, including those in the private sector, and
broadens them to propose technologies and policies
that could be implemented on a national scale. It
provides the federal government a path forward to
implement such a framework, and makes
recommendations to address the policy and technical
barriers that will need to be addressed.
xxi
Strategy V.A.3: Engage patients, providers,
researchers, and institutions to exchange
information through the learning health
system.
ONC is
working to ensure that its ongoing efforts related to
standards, certification, and governance of
nationwide health information exchange will align
with the vision for a learning health system.
The learning health system will only be as valuable as
the information that is exchanged. As more
organizations and members participate in the
learning health system, more knowledge will reach
more entities to make a positive impact on clinical
and research practices. ONC will engage the sources
of critical information – patients and providers – so

Federal Health IT Strategic Plan 46
that they understand the learning health system, its
relation to and interaction with research, and the
benefits of such research to inform the learning
health system. Increasing the engagement and
understanding of patients and providers may
increase their willingness to participate in
information sharing that they trust and that is private
and secure, including for secondary uses of EHR
data in research. Consumers stand to directly benefit
from more information flowing into the learning
health system which would allow for a better
understanding of which subgroups may respond
better to certain medications or treatments.
Consumers are also likely to benefit from the
availability of population level data in interacting
with their clinicians about what treatment is right for
them. Work to engage patients and providers will be
done directly and through representative consumer
and provider groups, as well as in public health
settings in underserved communities.
Strategy V.A.4: Grow the learning health
system by adding more members and
expanding policies and standards as
needed.
The government will seek to expand participation in
the learning health system early in the process,
beyond the initial group of federal partners, to add
private sector partners. Future participants could
include public and private provider groups, Health
Information Exchanges, payers, small community
medical and behavioral health practices, registries
and additional federal agencies. Incentives to join
this group will include the positive results of the
initial exchange activities and the possibility of
reciprocal benefit. The private sector is already
coming together to share data and knowledge via
various consortiums, and ONC will continue to
coordinate and learn from these efforts. As
standards and policies are expanded to support
system growth, the learning health system will
engage the private sector and will also support
government efforts at the state, local, and tribal
levels. Over the next five years, the government will
expand on the findings of the IOM study (see
strategy V.A.2) and continue evolving the federal
plan for the learning health system.
OBJECTIVE B
Broaden the capacity of health IT
thr
ough innovation and research
Strategy V.B.1: Liberate health data to
enable health IT innovation.
Facilitating access to health data, in accordance with
privacy and security protections, is a key mechanism
of the government to encourage innovation in the
industry and demonstrate to the public the value of
health IT. Rich and high quality data are the starting
point for building applications that provide value to
individuals and care providers. For instance, PHRs
become much more interesting if they can use the
patient’s entire medical history to provide advice on
how to reach personal health goals. Huge quantities
of data exist already, but in forms that are not easily
usable for those that could benefit from the data.
The government is working on multiple fronts to
correct this.
The first priority is giving individuals timely access to
their electronic personal health information. The
government is working to facilitate the ability for
users to successfully access, retrieve, process, and act
on the data easily and efficiently. This approach is
discussed at length in Goal IV Objective B. In
addition, the government is also seeking innovative
means for protecting users’ personal health
information, including effective techniques to de-
identify and segment data, and to facilitate informed
choice. As individuals become empowered with their
health data, demand for consumer health IT
applications will likely accelerate.
Outside of individual health information, the
government is a leading generator of health care
data. HHS maintains valuable information about the
health care system’s performance (e.g., the safety and
efficacy of treatments, disease surveillance).
Although much of this data is already public, it has
historically been stored in disparate datasets that are
largely inaccessible or unusable for developers. HHS
is now taking an active role in getting this data in the
hands of developers to activate innovation. This
includes the launch of
HHS.gov/Open, a website
tailored to providing the public more transparency
Federal Health IT Strategic Plan 47
into HHS’ administration, and the Community
Health Data Initiative (CHDI), a public-private
partnership committed to innovation through the
use of public data. CHDI is making many large data
sets, and tools that make those data sets useful,
readily downloadable from the CHDI website. It has
also organized contests and challenges to ignite
innovation using this data, such as the Health 2.0
Developer Challenge. In that ongoing contest,
anyone interested in submitting a challenge can do
so. Technology companies, health care companies,
and government agencies work together to both
identify specific market needs, and develop software
solutions using data to meet those needs. Dozens of
compelling applications have already been built as a
result of this challenge.
Strategy V.B.2: Make targeted investments
in health IT research.
The federal government is committed to investing
directly in health IT research and development in
areas that hold great promise for improving the
health of individuals and populations. NIH and
ARHQ, in particular, are funding dozens of research
projects related to the development of health IT.
Through the HITECH Act, ONC established the
Strategic Health IT Advanced Research Projects
(SHARP) Program, a four-year program funding
research in health IT security, patient-centered
cognitive support, health care applications and
network platform architectures, and secondary use
of EHR data. The progress made by grantees will
assist in developing best practices which can be
applied nationwide, possibly through meaningful use
requirements. AHRQ sponsors projects focused on
best practices and integration of health IT into the
practice of medicine. Focus topics include usability
of EHRs, clinical decision support, consumer health
IT, health information exchanges, and telehealth.
The Networking and Information Technology
Research and Development (NITRD) Program
coordinates federal research and development
investments in computing, networking, and software.
As required under the HITECH Act, NITRD is
developing a program and strategic plan to
coordinate research and development relating to
health IT. This work will make the pursuit of
important opportunities for technology
breakthroughs through coordinated inter-agency
initiatives possible, and will ensure that programs of
different agencies are non-redundant and mutually
reinforcing. In December 2010, PCAST issued a
report on all NITRD activities called Designing a
Digital Future: Federally Funded Research and Development
in Networking and Information Technology, which
emphasizes the importance of research to improve
health IT.
xxii
Strategy V.B.3: Employ government
programs and services as test beds for
innovative health IT.
Government agencies are leaders in adopting
innovative health IT into provider and payer
settings. Applying advanced health IT to the
government’s own health care practices and payment
administration creates a large market for
technologies, helps to prove their value, and creates
best practices for wider adoption.
VA’s Care Coordination Services uses health
informatics, e-care, and disease management
technologies to avoid unnecessary admission to
long-term institutional care facilities. Technologies
include videophones, messaging devices, biometric
devices, digital cameras, and remote monitoring
devices. VHA also has an award-winning PHR, “My
HealtheVet,” which gives its patients access to their
health information along with other VA information
and services. DoD’s MiCare portal enables its
patients to manage their medical information
through a PHR of their choice. IHS is in the process
of developing a PHR for its patients which will
support meaningful use requirements.
CMS is piloting free PHR options for Medicare
recipients. “Medicare PHR Choice” gives people
living in Arizona and Utah a choice among four
vendors’ PHRs, and automatically updates their
online record with Part A and Part B claims. “My
Personal Health Record South Carolina” allows
participants to see their medical history based on the
past two years of claims. Additional information can
be added manually, and the PHR provides helpful
resources to understand diagnoses, conditions, and
procedures.
Federal Health IT Strategic Plan 48
Strategy V.B.4: Monitor and promote
industry innovation.
The government facilitates and monitors the health
IT industry and stays abreast of innovation’s impact
on federal policies and programs in order to further
promote innovation within the industry. Such
activity is conducted primarily through panels,
conferences, white papers, and similar outreach
efforts. The government also plans to promote
innovation through open innovation prizes and
challenge grants focused on specific health IT
problems. Potential focus areas include helping to
ensure privacy and security in the digital health
infrastructure, increasing the usability of health
information systems to enhance provider
interactions, the creation of new analytical
techniques to inform improved care, and the
development of more efficient methods of data
compression and communication through modalities
such as mobile health.
Strategy V.B.5: Provide clear direction to the
health IT industry regarding government
roles and policies for protecting individuals
while not stifling innovation.
ONC commissioned the Institute of Medicine
(IOM) to thoroughly evaluate health IT patient
safety concerns and to recommend additional
actions and strategies to address those concerns, as
well as to define the role of public and private
sectors in ensuring the safety of health IT-assisted
health care services. Over the next two years, ONC,
in collaboration with federal partners, will develop a
consistent approach to health IT that protects
individuals without stifling innovation. The
government is committed to being as open and
transparent as possible in formulating its approach.
Federal Health IT Strategic Plan 49
Appendix A: Performance Measures
The performance measures below reflect key aspects of progress towards achieving the goals in this Federal Health
IT Strategic Plan for 2011-2015, and the overarching goal that all Americans will benefit from EHRs. These
performance measures are not intended to be a complete set, but a subset of key indicators in assessing progress.
Supporting information for these performance measures is contained in ONC’s Annual Performance Plan and
Report, which is integrated into the annual Congressional Budget Justification, which is available on the HHS
website. The most recent assessment about the status of meeting each goal is also included to provide a baseline
from which ONC aims to improve performance.
Goal Performance Measures
Most Recent
Assessment of
Performance Data Sources
I. Achieve
Adoption and
Information
Exchange
through
Meaningful Use
of Health IT
Increase the percentage of
eligible professionals receiving
Medicare and Medicaid EHR
Incentive Programs payments
N/A
Baseline TBD
(FY 2011)
Centers for Medicare &
Medicaid Services (CMS)
Meaningful Use Registration
and Attestation System
Better performance in hospitals:
Increase the percentage of
eligible hospitals receiving
Medicare and Medicaid EHR
Incentive Programs payments
Increase the percentage of
hospitals that have adopted
electronic health records
N/A
Baseline TBD
(FY 2011)
12% (CY 2009)
CMS Meaningful Use
Registration and Attestation
System
American Hospital Association
(AHA) Annual Survey of
Hospitals, IT Supplement
Better performance for physicians:
Increase the percentage of
eligible primary care
professionals receiving
meaningful use incentive
payments
Increase the percentage of
Federally Qualified Health
Centers (FQHCs) that are
affiliated with providers that
receive Medicare and Medicaid
EHR Incentive Programs
payments
Increase the percentage of
office-based physicians who
have adopted electronic health
records
Increase the percentage of
office-based primary care
physicians who have adopted
N/A Baseline
TBD (FY 2011)
N/A Baseline
TBD (FY 2011)
21% (CY 2009)
20% (CY 2009)
CMS Meaningful Use
Registration and Attestation
System
TBD
CDC National Ambulatory
Medical Care Survey, IT
Supplement
Centers for Disease Control
and Prevention (CDC),
National Ambulatory Medical
Federal Health IT Strategic Plan 50
Goal Performance Measures
Most Recent
Assessment of
Performance Data Sources
electronic health records
Care Survey, IT Supplement
Increase the percentage of
community pharmacies in the
U.S. that are capable of
exchanging health information
electronically
85% (CY 2009)
Surescripts National Progress
Report on E-Prescribing
II. Improve Care,
Improve
Population
Health, and
Reduce Health
Care Costs
through the Use
of Health IT
Proportion of eligible providers
in Beacon Communities that
receive Medicare and Medicaid
EHR Incentive Programs
payments
N/A
Baseline TBD
(FY 2011)
ONC Office of State and
Community Programs,
Beacon Division
Number of providers
participating in Beacon
Community interventions
N/A
Baseline TBD
(FY 2011)
ONC Office of State and
Community Programs,
Beacon Division
III. Inspire
Confidence
and Trust in
Health IT
Decrease the percentage of
Americans who are very
concerned about the security of
electronic health records
N/A
Baseline TBD
(FY 2011)
ONC Privacy and Security
Attitudes Survey
IV. Empower
Individuals with
Health IT to
Improve their
Health and the
Health Care
System
Increase the percentage of
Americans who have been given
electronic access to any part of
their health care record
N/A
Baseline TBD
(FY 2011)
ONC Privacy and Security
Attitudes Survey
V. Achieve Rapid
Learning and
Technological
Advancement
Measure TBD
N/A
Baseline TBD
Data Source TBD
Federal Health IT Strategic Plan 51
Appendix B: Programs, Initiatives, and Federal
Engagement
Department of Agriculture (USDA) improves agricultural productivity and competitiveness and contributes
to the national economy and the public health. The Recovery Act appropriated funds to the Department of
Agriculture’s Rural Utilities Service (RUS) and the Department of Commerce’s National Telecommunications
Information Administration (NTIA) to expand broadband access and adoption in communities across the U.S.,
to increase jobs, spur investments in technology and infrastructure, and provide long-term economic benefits.
Department of Commerce (DoC) has cross-cutting responsibilities in the areas of trade, technology,
entrepreneurship, economic development, environmental stewardship, statistical research, and analysis. Its
involvement with health IT has been evident through one of its agencies, the National Institute for Standards
and Technology.
– National Institute of Standards and Technology (NIST) is a non-regulatory federal agency whose
mission is to promote U.S. innovation and industrial competitiveness by advancing measurement
science, standards, and technology in ways that enhance economic security and improve quality of life.
NIST collaborates with HHS/ONC in realizing the health IT goals of the Administration and
Congress. This relationship allows ONC to draw upon NIST expertise in applying IT to health
care through standards, conformance measurement, prototype implementation, security, and
usability, and in consulting on the Nationwide Health Information Network, standards, and
certification processes.
NIST has funded a grant on the “Relationship Between Health IT Usability and Patient Safety:
A Human Factors Engineering Framework for Action.” This grant will develop a framework
explaining how the multiple facets of usability may be linked to different aspects of patient
safety.
Department of Defense (DoD) provides health care to all U.S. military personnel worldwide through the
Military Health System (MHS) and is supported by a robust EHR system.
– Armed Forces Health Longitudinal Technology Application, (AHLTA) the military’s EHR, is an
enterprise-wide medical and dental information management system that provides secure online access
to Military Health System (MHS) beneficiaries’ records. It is used by medical clinicians in all fixed and
deployed Military Treatment Facilities (MTFs) worldwide. This centralized EHR allows health care
personnel worldwide to access complete, accurate health data to make informed patient care decisions.
– Virtual Lifetime Electronic Record, (VLER) will permit information vital to health care, benefits
and services to be available to the DoD and the VA from the moment a service member enters the
military until the death of the service member or veteran. Both the DoD and VA have begun to work
together to define and build a seamless system of integration that will provide a framework to ensure
that health care providers have all the information they need to deliver high-quality health care, while
reducing medical errors. VLER is intended to be a lifetime, personal record that ensures a seamless
continuum of care and benefits. VLER leverages the work of CONNECT and the Nationwide Health
Information Network in service to military and veteran personnel.
– Electronic Health Record (EHR) Way Ahead is a proposed Major Automated Information System
(MAIS) program designed to replace/sunset the current portfolio of systems providing initial EHR
capability, primarily AHLTA and Composite Health Care System (CHCS). EHR Way Ahead will
Federal Health IT Strategic Plan 52
establish a comprehensive, longitudinal, electronic health record that is available anytime and anywhere
for the lifetime of every patient. This longitudinal electronic health record will support a virtual lifetime
electronic record (VLER) for a service member by being a source system for health care information to
be shared via VLER.
– “Blue Button” is a web-based portal enabling individuals to download their personal health
information and share this information with health care providers, caregivers, and others they trust. It
provides consumers with a standardized and reusable copy of their health information through a simple
download function on DoD, VA and CMS’ websites.
Department of Health and Human Services (HHS) is the principal agency responsible for protecting the
health of all Americans and has many agencies and initiatives that work towards advancing health IT within the
U.S. and implementing various aspects of the Affordable Care Act and the HITECH Act.
– Text4Baby is a free mobile information service designed to promote maternal and child health by
connecting women to prenatal and infant care services, as well as providing tips on what women need
to know during pregnancy and the baby’s first year. Text4baby is made possible through a broad,
public-private partnership that includes government agencies, corporations, academic institutions,
professional associations and non-profit organizations.
– Section 2041 of the Affordable Care Act authorizes the Secretary of HHS to make grants to long-term
care facilities for the purpose of assisting such entities in offsetting the costs related to the purchasing,
leasing, developing, and implementing of certified EHR technology.
– Agency for Healthcare Research and Quality (AHRQ)
is the lead federal agency charged with
improving the quality, safety, efficiency, and effectiveness of health care for all Americans. AHRQ
supports health services research that seeks to continuously improve the quality of health care and
promote evidence-based decision-making.
AHRQ’s Health IT Portfolio has supported health services research grants and contracts that
create new knowledge, synthesize and disseminate best evidence and provide tools for
implementation addressing health IT’s impact on the quality of health care since 2004. Current
initiatives address clinical decision support, patient safety, patient centered care, quality
measurement, and usability and workflow issues. Examples like treating chronic illness in an
effective and efficient manner using telemedicine through Project ECHO in New Mexico,
texting diabetic patients in Colorado to incorporate their blood sugar readings into an EHR, or
using health IT to reduce the incidence and impact of pressure ulcers in long term care
facilities in Utah, demonstrate the power of health IT to revolutionize the health care system.
In this portfolio, AHRQ has developed a publically available web site, United States Health
Information Knowledgebase (USHIK.ahrq.gov) where information (metadata: such as name,
definition, how they are represented) about the data elements from the HHS Secretary’s
National Interoperability Standards (HIPAA transactions, Consolidated Health Informatics,
Health Information Technology Standards Panel, and others) is related to the data elements’
use cases and the standards from which they come. This site promotes understandable health
information exchange and the uniformity of data used for health research and decision-making.
AHRQ’s Patient-Centered Health Research/Effective Health Care Portfolio supports projects
that develop the information infrastructure needed to conduct patient--centered health
research and enable a learning health care system. Current initiatives are supporting
infrastructure development projects, EHC distributed data research networks and enhanced
clinical registries, and methods work to support them. The Portfolio includes efforts like the
Federal Health IT Strategic Plan 53
Safe Surgery Project at the University of Washington, which has implemented a standardized
surgical checklist statewide to improve safety.
– Assistant Secretary for Preparedness and Response (ASPR)
serves as the Secretary’s principal
advisor on matters related to bioterrorism and other public heath emergencies.
ASPR is looking to health IT, EHRs, and Joint Patient Tracking Systems (JPTS) to assist in
addressing various functions, including Identifying at Risk Individuals, Strategic National
Stockpiling, City Readiness Initiative, Medical Reserve Corps coordination, Emergency System
Management for Advance Registration of Volunteer Health Professionals, Hospital
Preparedness, and National Disaster Medical Management.
– Assistant Secretary for Planning and Evaluation (ASPE) is the principal advisor to the HHS
Secretary on policy development, and is responsible for major activities in policy coordination,
legislation development, strategic planning, policy research, evaluation, and economic analysis and is
currently building a multi-payer, multi-claim database to support patient-centered research using
Medicare, Medicaid, and private payer claims data.
ASPE is leading the Department’s research initiatives and focus on health IT adoption by post-
acute and long-term care providers, including identifying health IT standards to advance
interoperable health information by post-acute and long-term care providers, and producing
the HITECH required Report to Congress in which the Secretary is to determine the extent to
which and manner in which incentives and other funding for using certified EHRs should be
made available to providers who are not eligible for incentives or other funding for such
purposes.
– Centers for Disease Control and Prevention (CDC)
collaborates to create the expertise,
information, and tools that people and communities need to protect their health – through health
promotion, prevention of disease, injury and disability, and preparedness for new health threats.
The Public Health Information Network (PHIN) is a national initiative to increase the
capacity of public health to exchange data and information electronically across organizational
and jurisdictional boundaries by promoting the use of standards and defining functional and
technical requirements. PHIN strives to improve public health by enhancing research and
practice through best practices related to efficient, effective, and interoperable public health
information systems.
The National Healthcare Safety Network (NHSN) is a voluntary, secure, Internet-based
surveillance system that integrates patient and health care personnel safety surveillance systems
and has the capacity for health care facilities to share data in a timely manner between health
care facilities and with other entities.
The National Electronic Disease Surveillance System (NEDSS), a major component of
PHIN, advances the transition to standards-based electronic data exchange for reportable
disease surveillance to improve local/state/territorial capacity to detect and respond to
reportable diseases and the nation’s ability to support the revised International Health
Regulations.
BioSense is a national program to improve capabilities for rapid disease detection, monitoring,
and real-time situational awareness through access to existing data from health care
organizations. BioSense enables local and state public health departments to share and access
Federal Health IT Strategic Plan 54
data, providing a more complete picture of potential and actual health events both locally and
across jurisdictional boundaries.
The National Environmental Public Health Tracking Network integrates health,
exposure, and hazard data from a variety of national, state, and city sources and offers a new
understanding of how hazardous substances can contribute to illness.
National Center for Health Statistics, as the Nation’s principal health statistics agency,
provides statistical information that will guide actions and policies to improve the health of the
American people. NCHS collects data from birth and death records, medical records, interview
surveys, and through direct physical exams and laboratory testing. NCHS is a key element of
the national public health infrastructure, providing important surveillance information that
helps identify and address critical health problems.
“Strengthening Public Health Infrastructure for Improved Health Outcomes” is funded
within the Prevention and Public Health Fund under the Affordable Care Act and is designed
to advance any or all of the key areas for infrastructure investment and to help ensure
successful implementation of the Affordable Care Act, specifically by: improving the public
health workforce, developing information systems to support adoption and implementation of
rules and regulations, reengineering of infrastructure to improve networking and coordination,
implementing best health care practices and impact evaluation, improving information and
data system capacity, and improving organizational capacity. The new program is seeking to
increase the performance management capacity of public health departments and ensure that
public health goals are being met.
CDC’s Public Health Informatics and Technology Program Office (PHITPO) at the Office of
Surveillance, Epidemiology and Laboratory Services (OSELS) is leading the development of
public health standards that align with certified EHR technology. As with clinical data, public
health departments require public health standards and may benefit from certified public
health information systems to effectively exchange information.
– Centers for Medicare & Medicaid Services (CMS) is the federal agency that oversees the Medicare
and Medicaid EHR Incentive Programs, thus playing a key role in the overall direction of the health
care system. The HITECH Act established the incentive programs to provide payments for the
meaningful use of certified EHR technology. The Medicare and Medicaid EHR Incentive Programs
provide payments to eligible professionals and hospitals who meet meaningful use requirements. These
incentive programs are designed to instill the use of EHRs in a meaningful way to support the nation in
improving care, efficiency, and population health.
The Center for Medicare and Medicaid Innovation (Center for Innovation or CMMI)
was established to test innovative payment and service delivery models to reduce program
expenditures under the applicable titles while preserving or enhancing the quality of care.
My Personal Health Record South Carolina (MYPRSC) is a Personal Health Record
(PHR) pilot conducted by CMS that provides an online PHR to Medicare beneficiaries who
reside in South Carolina and have original (fee-for-service) Medicare.
Medicare PHR Choice, a PHR pilot conducted by CMS, for people with original (fee-for-
service) Medicare residing in Utah and Arizona.
Under the Children’s Health Insurance Program Reauthorization Act of 2009
(CHIPRA), CMS has awarded ten Quality Demonstration grants in a total of 18 States to
Federal Health IT Strategic Plan 55
implement and evaluate provider performance measures, utilize health information
technologies such as pediatric electronic health records, and test the effectiveness of provider
delivery models such as medical homes.
The Affordable Care Act also provides $300 million dollars for the development and
implementation of a voluntary Medicaid Adult Health Quality Measures Program -
including quality measures that can be collected via electronic health records.
“Blue Button” is a web-based portal enabling individuals to manage their personal health
information and provide access to health care providers, caregivers, and others they trust. The
Blue Button feature allows individuals to access and download information into a text file (or
an enhanced PDF) that can be read, printed, or saved on any computer. The download can be
broken out by data class or data range. Blue Button allows control of information without
special software – and enables individuals the ability to share data with their health care
providers, caregivers, or people they trust. It provides consumers with a standardized and
reusable copy of their health information through a simple download function on DoD, VA
and CMS’ websites.
– Food and Drug Administration (FDA)
is the primary federal agency responsible for protecting the
public health by assuring the safety, efficacy, and security of human and veterinary drugs, biological
products, and medical devices, and providing oversight of the nation’s food supply, cosmetics, products
that emit radiation, and tobacco products. FDA also promotes the public health by promptly and
efficiently reviewing clinical research and taking timely and appropriate action on the marketing of
regulated products. The agency’s actions support innovations that make medical products more
effective and safer. FDA also helps the public obtain the accurate, science-based information they need
to use medical products and appropriately consume foods to improve their health. FDA’s Center for
Devices and Radiological Health (CDRH) is responsible for assuring the safety and effectiveness of
medical devices. CDRH will continue to monitor health IT patient safety concerns using its existing
programs and initiatives.
Medwatch-Plus provides electronic capability for receiving adverse event data, processing,
storing and analyzing adverse event reports and other safety information for human drugs,
medical devices, vaccines and other biologics, dietary supplements, and cosmetics. Alerts
issued based on this data contain useful information.
FDA Adverse Event Reporting System (FAERS) is a program within MedWatch Plus.
FAERS will provide a back-end database for processing, storing and analyzing post-market
adverse event reports and other safety information for FDA-regulated drug, biologic, and
medical device products.
The Sentinel Initiative is building a national electronic system, the Sentinel System, to
enhance FDA’s ability to track the safety of drugs, vaccines, biologics, and medical devices
once they reach the market. The Sentinel Initiative aims to develop and implement an active
surveillance system that will augment existing systems that the FDA has in place to track
reports of adverse events linked to the use of its regulated products.
Structured Product Labeling (SPL) is an electronic document markup standard approved
by Health Level Seven (HL7) and adopted by FDA as a mechanism for exchanging product
information. SPL is also used by FDA and NLM DailyMed initiative, which provides
information on human drugs and biologics in electronic format in an effort to improve
patient safety.
Federal Health IT Strategic Plan 56
– Health Resources and Services Administration (HRSA)
is the primary federal agency for
improving access to health care services for people who are uninsured, isolated or medically vulnerable.
In an effort to use health IT to extend access to health care, HRSA is working to identify, disseminate
and provide technical assistance to health centers and other HRSA grantees in adopting model practices
and technologies. HRSA is also working collaboratively with foundations, national organizations, the
private sector, and other government agencies to help HRSA grantees adopt health IT.
The HRSA Health Disparities Collaborative (HDC) was created to assist in the
transformation of primary health care practices to improve the health care provided to
everyone and to eliminate health disparities. This initiative was originally funded by HRSA but
now continues as a public-private endeavor.
HRSA’s Telehealth Network Grant Program supports established telehealth networks that
are looking to expand the number of sites receiving clinical services.
HRSA’s Telehealth Resource Program funds Centers of Excellence that provide technical
assistance on telehealth to any HRSA grantee in the country.
Telehealth Services for Children and Youth with Epilepsy grants fund initiatives to
demonstrate ways to improve the system of services for children and youth with epilepsy
through the use of telehealth/telemedicine.
Health Center Controlled Networks (HCCNs) improve operational effectiveness and
clinical quality in health centers through the provision of management, financial, technology
and clinical support services. An overwhelming number of community health centers who
have signed on with an HCCN have successfully adopted an EHR system.
Health IT Toolboxes provide a compilation of resources to help community health centers,
safety net providers and ambulatory care providers implement health IT and better understand
meaningful use.
The National Health Service Corps (NHSC), through scholarship and loan repayment
programs, helps Health Professional Shortage Areas (HPSAs) in the U.S. get the medical,
dental, and mental health providers they need to meet their tremendous need for health care.
The Rural Health Network Development Planning Grant Program (Network Planning)
expands access to, coordinates and improves the quality of essential health care services and
enhances the delivery of health care, in rural areas. The program provides one-year grants to
rural entities to plan and develop a formal health care network.
HRSA Pediatric Primary Care Electronic Health Record (EHR) Network for
Comparative Effectiveness Research (CER). The CER study is testing, via a cluster
randomized trial, a point-of-care clinical decision support system linked to electronic health
records in improving the quality of care for a chronic pediatric condition.
The Community Health Applied Research Network (CHARN) is a consortia of
researchers based at community health centers funded under the 2009 Recovery Act. The
CHARN will demonstrate that a well conceived and fully operational data infrastructure can be
put in place to support patient-centered outcomes research (PCOR) on diverse populations
and patient subgroups that are often underrepresented in health outcomes research. The
CHARN will actively disseminate research results to patients and clinicians in safety net
treatment settings.
Federal Health IT Strategic Plan 57
Integrating Child Health Information Systems through health information exchange funds
allows states to develop an interoperable system of collecting and exchanging information
including immunizations, vital statistics, and newborn screening. States and public health
departments are implementing systems that enhance communication and facilitate the
exchange of information between multiple partners including clinicians, laboratorians, public
health agencies, researchers and various community support services.
– Indian Health Service (IHS) is responsible for providing federal health services to American Indians
and Alaska Natives. The IHS is the principal federal health care provider and health advocate for Indian
people and its goal is to raise their health status to the highest possible level. The IHS provides a
comprehensive health service delivery system for approximately 1.9 million American Indians and
Alaska Natives who belong to 564 federally recognized tribes in 35 states. The IHS has long leveraged
health IT to serve its populations, some of whom are located in the most remote areas of the country.
Indian Health Service, along with its Tribal and Urban Program partners, have developed and deployed
a comprehensive suite of software applications to support the provision of quality services and the
secure management of health information.
IHS Resource and Patient Management System (RPMS) is the suite of health IT
applications that support health care delivery throughout the IHS. The RPMS includes an
EHR, population management tools, clinical decision support, quality reporting, integrated
behavioral health, electronic dental record, practice management, patient registration and
management, and other integrated applications. In April 2011, IHS became the first federal
agency to have part of its health information system certified for stage one meaningful use.
The IHS RPMS Suite is certified as a Complete EHR for both inpatient and ambulatory
settings. Part of the EHR system development included creation of a personal health record
(PHR) portal to support meaningful use requirements related to engaging patients and their
families in their health care.
IHS Population Health Management (iCare) is the IHS’ population management tool that
enables providers to easily identify groups of patients (populations) that share similar
characteristics. It presents diverse patient data in a user-friendly view by retrieving patient
information from the various underlying components of the RPMS database and bringing it
together under a single interface. User-defined patient lists (panels) are easily created, sorted
and filtered in a variety of ways to form the core functionality of iCare. The Care Management
Event Tracking (CMET) electronically tracks and manages certain pre-defined events related to
breast, cervical, colon, and skeletal health from screening through completion. “Anonymous
Community Alerts” related to CDC Nationally Notifiable Diseases and Suicidal Behavior are
mined on a nightly basis and displayed in a variety of locations to promote early awareness and
allow for prompt intervention.
IHS Patient Wellness Handout (PWH) is a paper-based report for patients that combines
information from their medical records along with an explanation of their results. It can be
used to provide patients with a listing of the recommended health maintenance services that
are due, serve as a tool to promote health communication, or as a portable record of selected
health information. The PWH can be generated on demand by anyone who is providing care
services to the patient.
IHS National Patient Information Reporting System (NPIRS) is the national data
warehouse for the IHS. The NPIRS maintains historical data from RPMS and other sources to
Federal Health IT Strategic Plan 58
provide information on health trends, cost and quality reporting, and individual data marts for
specific chronic health care challenges, such as diabetes.
IHS Infrastructure, Office Automation, and Telecommunications (IOAT) is the
foundational network of hardware, software and services that support RPMS, NPIRS and the
operations of the IHS. The IOAT enables information exchange for RPMS and security for all
IHS operations.
– The Office of Minority Health (OMH)
has developed and supports the National Health Information
Technology (NHIT) Collaborative that works to bridge gaps between coordinating and implementing
health IT within underserved communities, helping to educate health care providers and advocate
within these communities concerning the use and application of health IT, and advising other federal,
state and local agencies of how to best coordinate the use of health IT within underserved communities
of color.
– National Institutes of Health (NIH) is the primary federal agency for the support and conduct of
biomedical and behavioral research. Its mission is to seek fundamental knowledge about the nature and
behavior of living systems and apply it to enhance health, lengthen life, and reduce the burdens of
illness and disability. In terms of health IT, NIH supports and conducts research and standards
development to advance the meaningful use of certified EHR technology in research and clinical
practice. Given the unprecedented opportunities to answer new and important research questions using
the information contained in EHRs, NIH is working assiduously to facilitate appropriate access and
exchange of data for research purposes. Health IT is of interest and relevance to all of the NIH
Institutes and Centers. A few examples of relevant NIH activities include the following:
The National Library of Medicine (NLM) has a lead role in federal health IT policy as the
central coordinating body for clinical terminology standards within HHS. NLM supports,
develops, and disseminates key health data standards that are designated to enable certain users
to achieve meaningful use of the certified EHRs. NLM supports and conducts research and
development related to health IT, including clinical terminologies, clinical decision support,
personally controlled EHRs, health information exchange, syndrome surveillance, anatomical
image databases, natural language processing, information retrieval, advanced
telecommunications, and information infrastructure for emergency response. NLM also
manages the ClinicalTrials.gov databank which contains public information and data on clinical
trials. NLM also supports the training of health IT professionals through academic biomedical
informatics research training centers.
Cancer Biomedical Informatics Grid (caBIG®) is an information network supported by
the National Cancer Institute (NCI) enabling members of the cancer community – researchers,
providers, and patients – to collect, manage, and analyze large volumes of biomedical and
clinical data. The components of caBIG® are widely applicable beyond cancer as well.
The Electronic Medical Records and Genomics (eMERGE) Network, an initiative of the
National Human Genome Research Institute (NHGRI), is developing, disseminating, and
applying approaches to research that combine DNA biorepositories with electronic medical
record (EMR) systems for large-scale, high-throughput genetic research.
NHGRI and NCI have collaborated with the Office of the Surgeon General and the Office of
the Secretary to develop standards and tools for the collection, storage and dissemination of
family history information. The U.S. Surgeon General’s My Family Health Portrait (MFHP)
has been a centerpiece of these activities to date. It is a free web-based tool for family history
Federal Health IT Strategic Plan 59
collection that is standards-based and potentially interoperable with EHR systems. Recently an
inter-agency NIH working group has been established to address future governance of MFHP.
Future activities include the development of clinical decision support tools for common
heritable conditions that are compatible with MFHP.
The National Institute of Biomedical Imaging and Bioengineering’s Radiological
Society of North America RadLex Ontology Project provides uniform terms and concepts
for indexing and retrieving imaging research databases, educational materials, and clinical
imaging reports in an EHR. The project develops and deploys radiology reporting templates
for EHR software.
The NIH Clinical Center, in association with a number of NIH Institutes, developed the
Biomedical Translational Research Information System (BTRIS), a repository of clinical
research data that facilitates the conduct of intramural clinical trials. BTRIS is also addressing
important questions related to the standardization and aggregation of EHR data that will be
relevant to other national efforts involving EHR data reuse.
– Office for Civil Rights (OCR)
administers and enforces four key privacy and security laws: 1) the
HIPAA Privacy Rule, which protects the privacy of individually identifiable health information; 2) the
HIPAA Security Rule, which sets national standards for the security of electronic health information;
and 3) the HIPAA Breach Notification Rule, which requires HIPAA covered entities to notify
individuals, HHS, and in some cases the media of impermissible uses and disclosures of health
information that compromise the privacy and security of such information; and 4) the confidentiality
provisions of the Patient Safety Rule, which protect identifiable information being used to analyze
patient safety events and improve patient safety. Together, ONC and OCR are the lead HHS offices for
health-IT-related privacy and security policy.
OCR also enforces federal civil rights laws protecting individuals from discrimination on the
basis of race, color, national origin, gender, age, and disability and works with ONC to ensure
that health information technology benefits all individuals, including those who are protected
by these laws.
– Office of the National Coordinator for Health IT (ONC)
is at the forefront of the administration’s
health IT efforts and is a resource to the entire health system to support the adoption of health IT and
the promotion of nationwide health information exchange. ONC is the principal federal entity charged
with coordinating nationwide efforts to implement and advance the use of health IT and promote the
electronic exchange of health information.
The Health Information Technology Extension Program (Regional Extension Centers
or RECs) offers technical assistance, guidance and information on best practices to support
and accelerate health care providers’ efforts to become meaningful users of certified EHR
technology.
The Health Information Technology Research Center (HITRC) helps support the RECs
by gathering information on effective practices and helping the RECs collaborate with one
another and with relevant stakeholders to identify and share best practices in EHR adoption,
meaningful use, and provider support.
The State Health Information Exchange Cooperative Agreement Program supports
states or state designated entities in building health information exchange capacity for
exchanging health information electronically across the health care system both within and
across states.
Federal Health IT Strategic Plan 60
The Beacon Community Cooperative Agreement Program supports communities at the
cutting edge of EHR adoption and health information exchange to build and strengthen their
health IT infrastructure and exchange capabilities to push them to achieve new levels of
sustainable health care quality and efficiency. These communities will focus on demonstrating
measurable improvements in care, efficiency, and population health.
The Health IT Workforce Development Program focuses on several key resources needed
to rapidly expand the availability of skilled health IT professionals who will support broad
adoption and use of health IT in the provider community.
The Strategic Health IT Advanced Research Projects (SHARP) Program funds research
focused on achieving breakthrough advances to address well-documented problems that have
impeded adoption of health IT. The knowledge generated from this program will help
accelerate progress towards meaningful use of health IT and a high performing, adaptive,
nationwide health care system.
The Nationwide Health Information Network is a set of standards, services and policies
that enable secure health information exchange over the Internet. The Nationwide Health
Information Network will provide a foundation for the exchange of health information across
diverse entities, within communities, and across the country.
The Federal Health Architecture (FHA) is an E-Government Line of Business initiative
managed by the Office of the National Coordinator for Health Information Technology. FHA
was formed to coordinate health IT activities among federal agencies that provide health and
health care services to citizens.
The CONNECT project is an E-government initiative managed by ONC. CONNECT was
formed as a consortium of interested federal agencies to develop software based on the
Nationwide Health Information Network specifications to support standards-based exchange.
The CONNECT software is available through an open source license and is used by both
federal and private sector organizations.
– Substance Abuse and Mental Health Services Administration (SAMHSA) is the lead agency
within the Department of Health and Human Services charged with Behavioral Health Services
integration into community and existing provider-based prevention and treatment systems at
community, State and national levels. The role of health IT in SAMHSA is incorporated into a broad
range of activities that include but are not limited to:
Working with the VA and DOD on Suicide Prevention National Lifeline activities to expand
and strengthen use of the VA model for EHR with a “flag” protocol to identify and coordinate
interventions and services for those at high risk of suicide, or with a past history of attempts.
Working with the VA’s Virtual Lifetime Electronic Record (VLER) initiative to demonstrate
privacy protected exchange of sensitive clinical records between community-based behavioral
health programs and VA health centers.
Working with several State behavioral health and Medicaid agencies to develop open source
EHRs and HIE services that integrate behavioral health within community-based health
homes and State Health and Human Service programs.
Testing the usability and feasibility of smartphone-based applications and patient links to
clinical services, including, but not limited to a recovery tool called Addiction
Comprehensive Health Enhancement Support System (A-Chess) – an online peer
Federal Health IT Strategic Plan 61
support group and clinical counselors, a GPS feature that sends an alert when the user gets
near an area of previous drug or alcohol activity, real-time video counseling, and a “panic
button” that allows the user to place an immediate call for help with cravings or triggers.
Open Behavioral Health Information Technology Architecture (OBHITA) supports the
creation of a behavioral health EHR reference model information technology architecture.
OBHITA will also build on privacy protection standards developed over the past five years.
The SAMHSA Health Information Network (SHIN) includes the National Clearinghouse
for Alcohol and Drug Information (NCADI) and the National Mental Health Information
Center (NMHIC). SHIN connects the behavioral health workforce and the general public to
the latest information on the prevention and treatment of mental and substance use disorders.
The NMHIC was developed to provide information about organizations dedicated to treating
and preventing medical illness, as well as information about federal grants, conferences, and
events.
Exploring the use of pharmacy and medical provider information from individual State
Prescription Drug Monitoring Programs and the National All Schedules Prescription
Electronic Reporting Act, or NASPER, to inform state and community treatment and
prevention programs, including community coalitions that will be using the Strategic Planning
Framework to identify and provide local, real time information regarding questionable
prescription drug abuse.
Providing Grants to Expand Substance Abuse Treatment in Targeted Areas of Need -
Technology Assisted Care (TCE - TAC). The purpose of this program is to enhance and/or
expand the capacity of substance abuse treatment providers to serve clients who have been
underserved because of lack of access to treatment in their immediate community due to
transportation concerns, an inadequate number of substance abuse treatment providers in their
community, and/or financial constraints, through the use of therapeutic techniques that
involve innovative, creative and cost-effective advanced technology. This approach includes
the use of various technological modalities such as Internet, tele-behavioral health, chatlines,
videocams, etc.
Regulating 1230 opioid treatment programs that dispense the treatment medications
methadone and buprenorphine to 288,824 patients nationwide. Through an interactive online
“Extranet,” providers extract patient health information from medical records, and submit an
electronic form that is evaluated concurrently by Federal and State regulatory authorities. The
system addresses exemptions from certain Federal and State regulatory requirements.
Working with the field to develop a digital access to medication (DAT-M) system. This Web-
based system would concentrate selected patient health information, including dose levels, into
an interoperable data base that could be securely accessed by providers throughout the
country. DAT-M is being developed to address opioid dependent patients to continue care
after being displaced by various disasters.
Providing U.S. public health statistics on the use of alcohol, illegal drugs, prescription drugs
and mental health issues through the Center for Behavioral Health Statistics and Quality. This
Center also provides information on substance use disorder treatment episodes. It also
publishes brief reports based on the National Survey on Drug Use and Health, the Drug
Abuse Warning Network, and the Treatment Episode Data set.
Federal Health IT Strategic Plan 62
Request for Application (RFA) for Supplemental Funds for Health IT Infrastructure
Development. Two new RFAs were announced that are specifically designed for the following
entities: 1) current Primary and Behavioral Health Care Integration (PBHCI) grantees ($11.2
million); and 2) State-Designated-Entities (SDEs), including for technical assistance to States
and grantees ($3.8 million). The purpose of the PBHCI program is to improve the physical
health status of people with serious mental illnesses, including individuals with co-occurring
substance use disorders, by supporting communities to coordinate and integrate primary care
services into publicly funded community mental health and other community-based behavioral
health settings. The overarching goal for the supplemental funding for HIT is to integrate care
across and among providers via the appropriate use of certified EHR technology.
Department of Veterans Affairs (VA) provides Veterans with health benefits and uses EHR systems to better
their service and accelerate consumer use.
– Veterans Health Information Systems and Technology Architecture (VistA) is an enterprise-wide
information system built around an EHR, used throughout the VA medical system which is known as
the Veterans Health Administration (VHA). VistA is one of the most widely used EHRs in the world.
– Virtual Lifetime Electronic Record, (VLER) will permit information vital to health care, benefits
and services to be available to the DoD and the VA from the moment a service member enters the
military until the service member or veteran’s death. Both the DoD and VA have begun to work
together to define and build a seamless system of integration that will provide a framework to ensure
that health care providers have the information they need to deliver high-quality health care, while
reducing medical errors. VLER is intended to be a lifetime, personal record that ensures a seamless
continuum of care and benefits. VLER leverages the work of CONNECT and the Nationwide Health
Information Network in service to military and veteran personnel.
– “Blue Button” is a web-based portal enabling individuals to manage their personal health information
and provide access to health care providers, caregivers, and others they trust. It provides consumers
with a standardized and reusable copy of their health information through a simple download function
on DoD, VA and CMS’ websites.
– My Health
e
Vet is VA’s e–health website, which offers Veterans, active duty service members, their
dependents, and caregivers access anywhere, anytime via the Internet to VA health care information
and services. My HealtheVet is a free, online PHR that empowers Veterans to become informed
partners in their health care by allowing access to trusted, secure, and current health and benefits
information, as well as the ability to record, track and store important health and military history
information.
– Care Coordination/Home Telehealth (CCHT) is the national program the VHA uses to coordinate
the care of veteran patients with chronic conditions. CCHT involves the systematic use of health
informatics, e-care, and disease management technologies to avoid unnecessary admission to long-term
institutional care facilities. Technologies include videophones, messaging devices, biometric devices,
digital cameras, and remote monitoring devices. E-care is an appropriate and cost-effective way to
manage chronic care patients in urban and rural settings and enables patients to live independently at
home.
– Healthcare Associated Infection & Influenza Surveillance System, (HAIISS) is a national VA IT
initiative that will allow VA healthcare providers to detect the development of healthcare acquired
infections in near real time; perform syndromic surveillance and track microbiological organisms of
epidemiologic significance, including automated reporting of infectious diseases to local public health
Federal Health IT Strategic Plan 63
agencies and CDC; and provide tools for tracking multidrug resistant organisms and monitoring
antimicrobial utilization in VA medical centers to improve the quality of care for Veterans. VA and
DoD are also working together to build a bi-directional biosurveillance system that will provide
improved situational awareness for public health related events.
Federal advisory committees are established or authorized by statute to provide advice or recommendations
to federal officials on issues or policies that are within the purview of the federal government. These committees
include groups from outside the federal government that afford an expertise or perspective not available within
the Department of other federal agencies. They provide a mechanism for public input into health IT policy.
– National Committee on Vital and Health Statistics (NCVHS) advises the HHS Secretary in the
area of health data, statistics, and national health information policy and the Department’s strategy to
best address those issues.
– HIT Policy Committee (HITPC) was created by the HITECH Act to make recommendations to the
National Coordinator for Health IT on a policy framework for the development and adoption of a
nationwide health information infrastructure, including standards for the electronic exchange and use of
patient medical information.
– HIT Standards Committee (HITSC) was created by the HITECH Act to make recommendations to
the National Coordinator for Health IT on standards, implementation specifications, and certification
criteria for the electronic exchange and use of health information.
Federal Communications Commission (FCC) is the federal agency responsible for regulating interstate and
international communications, and is actively involved in efforts to build the communications infrastructure
necessary to facilitate information exchange. FCC’s investments are helping to connect rural health communities
and improve access to health IT for more Americans.
– The Rural Health Care Pilot Program facilitated the creation of a nationwide broadband network
dedicated to health care and connecting public and private non-profit health care providers in rural and
urban locations.
– The Expanding Investment in Broadband Health Care Technology program will invest $400
million annually to enable doctors, nurses, hospitals and clinics to deliver, through communications
technology, world-class health care to patients no matter where they live. It is one of four programs in
the Universal Service Fund administered by the FCC.
Federal Health IT Taskforce serves as the overall government coordination body for policy development,
coordination and implementation of federal health IT activities. This Taskforce also aims to improve
transparency of federal government activities related to health IT and communication among federal agencies as
they execute federal health IT policy. The Taskforce is chaired by the National Coordinator, with OMB’s Health
Program Associate Director and the federal government’s Chief Information Officer and Chief Technology
Officer serving as vice chairs. Agency participants include senior policy officials from HHS (and its relevant
offices and operating divisions), DoD, VA, SSA, USDA, OPM, and Commerce.
Federal Trade Commission (FTC) advances consumers’ interests by sharing its expertise with federal and
state legislatures and U.S. and international government agencies. The Commission has been actively involved in
enforcing competition in health care markets. Alongside ONC and OCR, the FTC continues to analyze and
update breach notification policies and procedures to ensure they protect individuals’ rights and meet their
needs.
Federal Health IT Strategic Plan 64
Office of Personnel Management (OPM) provides comprehensive human resource services to all federal
agencies and employees. It continues to develop plans to encourage health insurance plans purchased by the
government to support meaningful use among their network of providers.
Social Security Administration (SSA) administers the Social Security Act, which provides benefits for
retirement, disabilities, and survivors. SSA is an important partner and early adopter of the Nationwide Health
Information Network. In partnership with MedVirginia, SSA uses the Nationwide Health Information Network
to obtain electronic medical records in disability cases, and is working with ONC and other Nationwide Health
Information Network cooperative members to expand this effort.
White House Office of Science and Technology Policy (OSTP) leads interagency efforts to develop and
implement sound science and technology policies and to work with the private sector, state and local
governments, the science and higher education communities, and other nations toward this end.
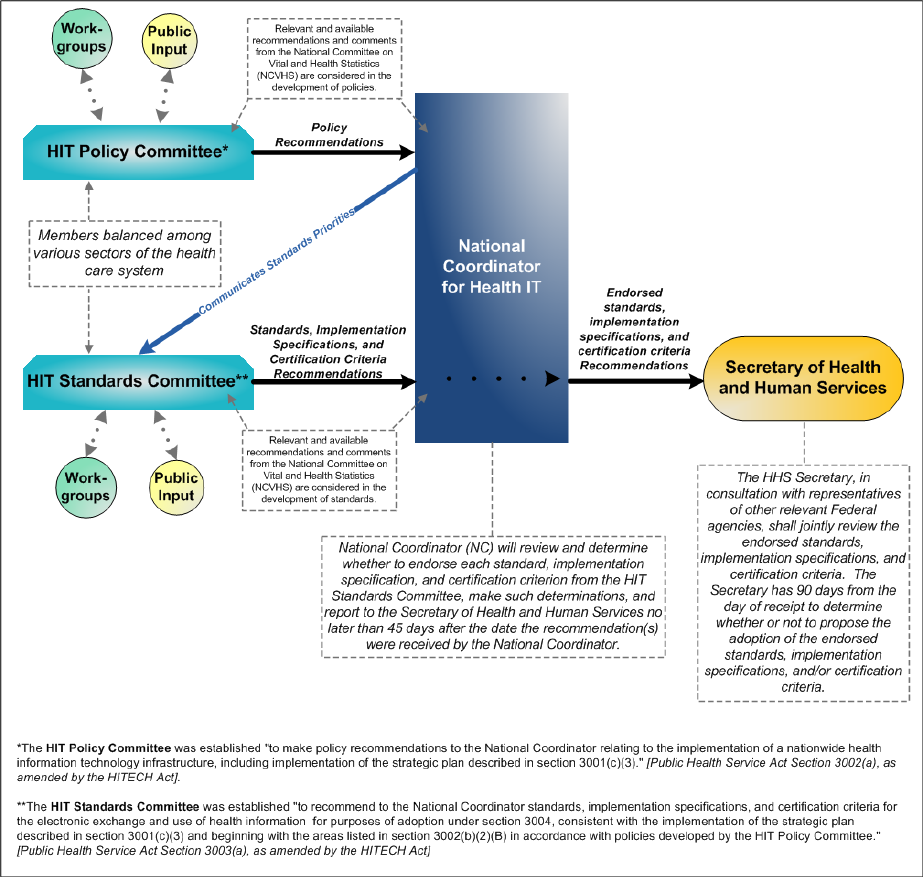
Federal Health IT Strategic Plan 65
Appendix C: HIT Standards and HIT Policy Committees
Information Flow
Figure 2; Flow of recommendations through the HIT Policy and Standards Committees, ONC, and
the HHS Secretary
Federal Health IT Strategic Plan 66
Appendix D: Process Approach
In creating the Federal Health IT Strategic Plan, several methods and key sources were utilized and incorporated in
order to achieve the final document. The process for obtaining input included working collaboratively with both
the public and private sectors, as well as gathering input from current policy and regulations.
At its core, the plan leverages the work of the Strategic Plan workgroup of the HIT Policy Committee. Beginning
in January 2010, the workgroup met regularly to devise a strategic plan framework that was submitted to the
Health IT Policy Committee which in turn submitted its recommended approach for consideration to the National
Coordinator. This framework served as a key input for consideration as ONC wrote the Federal Health IT
Strategic Plan. The framework was developed by members of the Workgroup which included health IT leaders
from across both the public and private sectors, and also incorporated feedback from the public gathered during
public meetings and a listening session.
Due to the diverse scope and multi-agency nature of the plan, it was essential to engage the federal health
community in various ways during the plan’s development and refinement. ONC conducted interviews and
conversations with representatives from key federal agencies and offices in order to create a cohesive and
integrated health IT plan across the federal government. After the meetings and discussions were held, ONC
looked to these federal agencies and leaders for valuable feedback on drafts of the plan, and intends to continue
this collaboration as the plan advances in the future.
ONC actively sought public input into the plan via its Health IT Blog and hosted a consumer working group
discussion with health IT leaders in the public and private sectors to gather input in developing its consumer
strategy (Goal IV).
The Federal Health IT Strategic Plan was developed with the crucial understanding that several policies and
regulations have critical implications pertaining to the current and future state of health IT (See Appendix E). The
Plan has also undergone a public comment period and has been updated to reflect input gathered from the public
during this process.
Federal Health IT Strategic Plan 67
Appendix E: Statutes and Regulations
Statutes
American Recovery and Reinvestment Act of 2009 (The Recovery Act)
On February 17, 2009, the President signed the Recovery Act. This statute includes the Health Information
Technology for Economic and Clinical Health Act (the HITECH Act) (see below) which establishes the Medicare
and Medicaid EHR Incentive Programs that encourage meaningful use of certified EHRs and other health
information technology (IT) to improve quality of care.
Health Information Technology for Economic and Clinical Health Act of 2009
(The HITECH Act)
The Health Information Technology for Economic and Clinical Health (HITECH) Act, passed as part of the
Recovery Act, allocated billions of dollars for the health care system to adopt and meaningfully use health IT to
improve health. A number of provisions in the HITECH Act strengthen the privacy and security protections for
health information established under the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
Health Insurance Portability and Accountability Act of 1996 (HIPAA)
HIPAA called for the establishment of standards and requirements for transmitting certain health information to
improve the efficiency and effectiveness of the health care system while protecting patient privacy. The
Administrative Simplification Regulations have been developed to implement the Administrative Simplification
provisions of HIPAA.
The Patient Protection and Affordable Care Act of 2010 (the Affordable Care Act)
On March 23, 2010, the President signed the Patient Protection and Affordable Care Act of 2010, later amended
by the Health Care and Education Reconciliation Act of 2010 (collectively, the Affordable Care Act), which,
among other things, is estimated to expand health care coverage to 32 million currently uninsured Americans by
2019. The Affordable Care Act builds on the HITECH Act and recognizes health IT as a critical enabler to broad
transformations in health care.
Regulations
Medicare and Medicaid Programs: Electronic Health Record Incentive Programs Final Rule
This rule implements the Recovery Act provisions that provide incentive payments to eligible professionals and
eligible hospitals that adopt and use certified EHR technology in a meaningful way. The programs seek to help
improve care, efficiency, and population health. This rule also specifies the initial criteria that eligible providers
must meet to qualify for the Medicare and Medicaid EHR incentive payments, and it includes other incentive
programs participation requirements.
Health Information Technology: Initial Set of Standards, Implementation Specifications, and
Certification Criteria for Electronic Health Record Technology Interim Final and Final Rules
Under these rules, the Secretary has adopted the initial set of standards, implementation specifications and
certification criteria that are required for the certification of EHR technology. These rules have been aligned to
support the achievement of meaningful use stage one by eligible professionals, eligible hospitals, and critical access
hospitals under the Medicare and Medicaid EHR Incentive Programs.
Federal Health IT Strategic Plan 68
Establishment of the Temporary Certification Program for Health Information Technology
Final Rule
This final rule establishes a temporary certification program for the purposes of testing and certifying health IT,
thereby ensuring the availability of Certified EHR Technology for eligible health care providers seeking incentive
payments available under the Medicare and Medicaid EHR Incentive Programs. This final rule is issued under the
authority granted to the National Coordinator by section 3001(c)(5) of the Public Health Service Act (PHSA), as
added by the HITECH Act. Under the temporary certification program, the National Coordinator will authorize
qualified organizations that meet specified requirements to conduct the testing and certification of Complete
EHRs and/or EHR Modules.
Establishment of the Permanent Certification Program for Health Information Technology
Final Rule
This final rule establishes a permanent certification program for the purpose of certifying health IT. This final rule
is issued pursuant to the authority granted to the National Coordinator for Health Information Technology (the
National Coordinator) by section 3001(c)(5) of the PHSA, as added by the HITECH Act. The permanent
certification program will eventually replace the temporary certification program that was previously established by
a final rule. The National Coordinator will use the permanent certification program to authorize qualified
organizations to certify certain types of EHR technology, such as Complete EHRs and/or EHR Modules. The
permanent certification program could also be expanded to include the certification of other types of health IT.
Breach Notification for Unsecured Protected Health Information Interim Final Rule
This rule implemented section 13402 of the HITECH Act by requiring HIPAA covered entities to provide
notification following a breach of unsecured protected health information to individuals, HHS, and in some
cases the media. This rule also requires business associates to notify covered entities following a breach of
unsecured protected health information.
HIPAA Privacy and Security Rules
The HIPAA Privacy Rule provides federal protections for individually identifiable health information held by
covered entities and gives patients an array of rights with respect to that information. At the same time, the Privacy
Rule is balanced so that it permits the disclosure of protected health information needed for patient care and other
important purposes. The HIPAA Security Rule specifies a series of administrative, physical, and technical
safeguards for covered entities to implement to assure the confidentiality, integrity, and availability of electronic
protected health information.
Modifications to the HIPAA Privacy, Security, and Enforcement Rules Under the HITECH Act
Proposed Rule
This rule proposes a number of provisions that would implement certain parts of the HITECH Act that are
designed to strengthen the privacy and security protections for health information established under HIPAA. In
addition to seeking to implement these HITECH Act provisions, this rule proposes a number of modifications to
improve the HIPAA Rules, which are not mandated in the HITECH Act. The Department issued this proposed
rule in 2010 and expects to finalize it in 2011.
HIPAA Privacy Rule Accounting of Disclosures Under the HITECH Act Proposed Rule
This rule proposes modifications to the HIPAA standard for accounting of disclosures of protected health
information. The modifications in part would implement the statutory requirement under the HITECH Act to
require covered entities and business associates to account for disclosures of protected health information to carry
out treatment, payment, and health care operations if such disclosures are through an electronic health record. The
Federal Health IT Strategic Plan 69
rule also proposes to expand the accounting provision to provide individuals with the right to receive an access
report indicating who has accessed electronic protected health information in a designated record set.
Federal Health IT Strategic Plan 70
Appendix F: Goals, Objectives, and Strategies
Goal I: Achieve Adoption and Information Exchange through Meaningful Use of Health IT
Objectives Strategies
I.A. Accelerate adoption
of electronic health
records
I.A.1. Provide financial incentive payments for the adoption and meaningful use of
certified EHR technology.
I.A.2. Provide implementation support to health care providers to help them adopt,
implement, and use certified EHR technology.
I.A.3. Support the development of a trained workforce to implement and use health
IT technologies.
I.A.4. Encourage the inclusion of meaningful use in professional certification and
medical education.
I.A.5.
Establish criteria and a process to certify EHR technology that can support
meaningful use criteria.
I.A.6. Communicate the value of EHRs and the benefits of achieving meaningful use.
I.A.7.
Align federal programs and services with the adoption and meaningful use
of certified EHR technology.
I.A.8. Work with private sector payers and provider groups to encourage providers to
achieve meaningful use.
I.A.9. Encourage and facilitate improved usability of EHR technology.
I.B. Facilitate
information
exchange to support
meaningful use of
electronic health
records
I.B.1. Foster business models that create health information exchange.
I.B.2. Monitor health information exchange options and fill the gaps for providers
that do not have viable options.
I.B.3. Ensure that health information exchange takes place across individual exchange
models, and advance health systems and data interoperability.
I.C. Support health IT
adoption and
information
exchange for
public health and
populations with
unique needs.
I.C.1. Ensure public health agencies are able to receive and share information with
providers using certified EHR technology.
I.C.2. Track health disparities and promote health IT that reduces them.
I.C.3. Support health IT adoption and information exchange in long-term/post-acute,
behavioral health, and emergency care settings.
Federal Health IT Strategic Plan 71
Goal II: Improve Care, Improve Population Health, and Reduce
Health Care Costs through the Use of Health IT
Objectives Strategies
II.A. Support more
sophisticated uses
of EHRs and other
health IT to
improve health
system performance
II.A.1. Identify and implement best practices that use EHRs and other health IT to
improve care, efficiency, and population health.
II.A.2. Create administrative efficiencies to reduce cost and burden for providers,
payers, and government health programs.
II.B. Better manage care,
efficiency, and
population health
through EHR-
generated reporting
measures
II.B.1. Identify specific measures that align with the National Quality Strategy.
II.B.2. Establish standards, specifications, and certification criteria for collecting and
reporting measures through certified EHR technology.
II.C. Demonstrate health
IT-enabled reform
of payment
structures, clinical
practices, and
population health
management
II.C.1. Fund and administer demonstration communities to show how the advanced
use of health IT can achieve measurable improvements in care, efficiency, and
population health.
II.C.2. Align health IT initiatives and clinical and payment reform pilots and
demonstrations.
II.D. Support new
approaches to the
use of health IT in
research, public and
population health,
and national health
security
II.D.1: Establish new approaches to and identify ways health IT can support national
prevention, health promotion, public health, and national health security.
II.D.2: Invest in health IT infrastructure to support the National Prevention and
Health Promotion Strategy.
II.D.3: Ensure a mechanism for information exchange in support of research and the
translation of research findings back into clinical practice.
Federal Health IT Strategic Plan 72
Goal III: Inspire Confidence and Trust in Health IT
Objectives Strategies
III.A. Protect
confidentiality,
integrity, and
availability of health
information
III.A.1. Promulgate appropriate and enforceable federal policies to protect the
privacy and security of health information.
III.A.2. Enforce existing federal privacy and security laws and maintain consistency
with federal policy.
III.A.3. Encourage the incorporation of privacy and security functionality into
health IT.
III.A.4. Assess technical solutions that could support more granular patient choice
and data segmentation.
III.A.5. Identify health IT system security vulnerabilities and develop strategic
solutions.
III.A.6. Identify health IT privacy and security requirements and best practices, and
communicate them through health IT programs.
III.B. Inform individuals
of their rights and
increase
transparency
regarding the uses
of protected health
information
III.B.1. Inform individuals about their privacy and security rights and how their
information may be used and shared.
III.B.2. Increase transparency regarding the development of policies and standards
related to uses and sharing of protected health information.
III.B.3. Maintain strong breach notification requirements.
III.C. Improve safety and
effectiveness of
health IT
III.C.1. Provide implementation and best practice tools for the effective use of
health IT.
III.C.2. Evaluate safety concerns and update approach to health IT safety.
III.C.3. Monitor patient safety issues related to health IT and address concerns.
Federal Health IT Strategic Plan 73
Goal IV: Empower Individuals with Health IT to Improve
their Health and the Health Care System
Objectives Strategies
IV.A. Engage individuals
with health IT
IV.A.1. Listen to individuals and implement health IT policies and programs to
meet their priorities.
IV.A.2. Communicate with individuals openly and spread messages through existing
communication networks and dialogues.
IV.B. Accelerate
individual and
caregiver access to
their electronic
health information
in a format they can
use and reuse
IV.B.1. Through Medicare and Medicaid EHR Incentive Programs, encourage
providers to give patients access to their health information in an electronic format.
IV.B.2. Through federal agencies that deliver or pay for health care, act as a model
for sharing information with individuals and make available tools to do so.
IV.B.3. Establish public policies that foster individual and caregiver access to their
health information while protecting privacy and security.
IV.C. Integrate patient-
generated health
information and
consumer health IT
with clinical
applications to
support patient-
centered care
IV.C.1. Support the development of standards and tools that make EHR technology
capable of interacting with consumer health IT and build these requirements for the
use of standards and tools into EHR certification.
IV.C.2. Solicit and integrate patient-generated health information into EHRs and
quality measurements.
IV.C.3. Encourage the use of consumer health IT to move toward patient-centered
care.
Goal V: Achieve Rapid Learning and Technological Advancement
Objectives Strategies
V.A. Lead the creation of
a learning health
system to support
quality, research,
and public and
population health
V.A.1. Establish an initial group of learning health system participants.
V.A.2. Develop standards, policies, and technologies to connect participants within
the learning health system.
V.A.3. Engage patients, providers, researchers, and institutions to exchange
information through the learning health system.
V.A.4. Grow the learning health system by adding more members and expanding
policies and standards as needed.
V.B. Broaden the
capacity of health IT
through innovation
and research
V.B.1. Liberate health data to enable health IT innovation.
V.B.2. Make targeted investments in health IT research.
V.B.3. Employ government programs and services as test beds for innovative
health IT.
V.B.4. Monitor and promote industry innovation.
V.B.5. Provide clear direction to the health IT industry regarding government roles
and policies for protecting individuals while not stifling innovation.
Federal Health IT Strategic Plan 74
Appendix G: Acronyms
Term/Acronym Description
AHLTA
Armed Forces Health Longitudinal Technology Application
AHRQ
Agency for Healthcare Research and Quality
ASPE
Office of the Assistant Secretary for Planning and Evaluation (HHS)
ASPR
Office of the Assistant Secretary for Preparedness and Response (HHS)
caBIG
®
The Cancer Biomedical Informatics Grid
caGrid
Infrastructure that supports caBIG
CDC
Centers for Disease Control and Prevention
CDS
Clinical Decision Support
CHDI
Community Health Data Initiative
CMS
Centers for Medicare & Medicaid Services
DHS
U.S. Department of Homeland Security
DoD
U.S. Department of Defense
DoEd
U.S. Department of Education
DoL
U.S. Department of Labor
DURSA
Data Use and Reciprocal Support Agreement
EHR
Electronic Health Record
FACA
Federal Advisory Committee Act
FCC
Federal Communications Commission
FDA
U.S. Food and Drug Administration
FHA
Federal Health Architecture
FTC
Federal Trade Commission
HDC
Health Disparities Collaborative (HRSA)
Health IT
Health Information Technology
HHS
U.S. Department of Health and Human Services
HHS/OS
U.S. Department of Health and Human Services, Office of the Secretary
HIE
Health Information Exchange
HIPAA
Health Insurance Portability and Accountability Act of 1996
HITECH ACT
Health Information Technology for Economic and Clinical Health Act
HITPC
HIT Policy Committee
HITRC
Health Information Technology Research Center
Federal Health IT Strategic Plan 75
Term/Acronym Description
HITSC
HIT Standards Committee
HITSP
Healthcare Information Technology Standards Panel
HRSA
Health Resources and Services Administration
IHS
Indian Health Service
IOM
Institute of Medicine
LTPAC
Long-term and post-acute care
mHealth
Mobile health
NAMS
National Ambulatory Medical Survey
NEDSS
National Electronic Disease Surveillance System
NIH
National Institutes of Health
NIST
National Institute of Standards and Technology
NITRD
Networking and Information Technology Research and Development Program
NLM
National Library of Medicine
NPRM
Notice of Proposed Rulemaking
NQF
National Quality Forum
NRC
The National Resource Center for Health Information Technology
OCR
Office for Civil Rights
OGC
Office of the General Counsel
OPM
Office of Personnel Management
ONC-ATCB
Office of the National Coordinator for Health IT – Authorized Testing and
Certification Body
ONC
Office of the National Coordinator for Health Information Technology
OPP
ONC’s Office of Policy and Planning
OSI
ONC’s Office of Standards and Interoperability
OSTP
The White House Office of Science and Technology Policy
PCAST
President’s Council of Advisors on Science and Technology
PHR
Personal Health Record
REC
Regional Extension Center
RPMS
Resource and Patient Management System (Indian Health Service’s Electronic
Health Record)
SAMHSA
Substance Abuse and Mental Health Services Administration
SDO
Standards Development Organizations
SSA
U.S. Social Security Administration
Federal Health IT Strategic Plan 76
Term/Acronym Description
State HIE
State Health Information Exchange Cooperative Agreement Program
SHARP
Strategic Health IT Advanced Research Projects
S&I
Standards and Interoperability
USDA
U.S. Department of Agriculture
VA
U.S. Department of Veterans Affairs
VHA
Veterans Health Administration
VistA
Veterans Health Information Systems and Technology Architecture
(VA’s Electronic Health Record)
Federal Health IT Strategic Plan 77
ONC
Office of the National Coordinator for Health Information Technology
200 Independence Avenue SW
Washington, DC 20201
Acknowledgements
The Office of the National Coordinator is deeply grateful to the leaders and key staff from each federal agency
involved with the development of this document.
Development of this plan was supported under contract HHSP23320095633WC by professional staff from
Deloitte Consulting LLP. The Office of the National Coordinator gratefully acknowledges Deloitte’s contributions
to this document.
Federal Health IT Strategic Plan 78
Notes
i
The National Ambulatory Medical Care Survey (NAMCS). American Hospital Association IT Supplement 2010.
http://www.hhs.gov/news/press/2011pres/01/20110113a.html. These estimates refer to the proportion of office-based physicians and non-
federal acute care hospitals that have achieved a “basic” level of electronic health record adoption. For more information about these measures, visit
http://healthit.hhs.gov/budget and view the Online Performance Appendix to the Fiscal Year 2012 President’s Budget Request to Congressional
Appropriations Committees.
ii
Consumers and Health Information Technology: A National Survey; April 2010, California HealthCare Foundation.
http://www.chcf.org/publications/2010/04/consumers-and-health-information-technology-a-national-survey
.
iii
Friedman, Charles P., Adam K. Wong, and David Blumenthal. "Achieving a Nationwide Learning Health System." Science Translational Medicine,
10 Nov. 2010. Vol 2.
iv
The “Meaningful Use” Regulation of Electronic Health Records. David Blumenthal and Marilyn Tavenner, August 5, 2010, New England
Journal of Medicine. http://www.nejm.org/doi/full/10.1056/NEJMp1006114
.
v
HHS Strategic Plan FY 2010-2015. US Department of Health and Human Services.
http://www.hhs.gov/secretary/about/priorities/priorities.html and the National Strategy for Quality Improvement in Health Care. US
Department of Health and Human Services, May 2011.
http://www.healthcare.gov/center/reports/quality03212011a.html
vi
Health IT Workforce Development Program. http://healthit.hhs.gov/portal/server.pt?open=512&objID=1432&mode=2.
vii
HHS/OMB Memorandum: Federal Agency Coordination on Health Information Technology (HIT), February 19, 2010.
http://www.whitehouse.gov/sites/default/files/omb/assets/memoranda_2010/m10-10.pdf.
viii
Stimulating the Adoption of Health Information Technology. David Blumenthal, M.D., M.P.P. N Engl J Med 2009; 360:1477-1479. April 9,
2009.
http://www.nejm.org/doi/full/10.1056/NEJMp0901592 .
ix Medicare Shared Savings Program: Accountable Care Organizations Proposed Rule published in the Federal Register on April 7, 2011
(76 FR 19528, 19652)
x
Sebelius Announces $42.5 Million for Public Health Improvement Programs through the Affordable Care Act.
http://www.cdc.gov/media/pressrel/2010/r100920.htm.
xi
Fair Information Practice Principles; Federal Trade Commission, June 25, 2007. http://www.ftc.gov/reports/privacy3/fairinfo.shtm.
xii
Nationwide Privacy and Security Framework for Electronic Exchange of Individually Identifiable Health Information; December 15,
2008.
http://healthit.hhs.gov/portal/server.pt/community/healthit_hhs_gov__privacy___security_framework/1173.
xiii
Accelerating Health Care Innovation to Achieve System-Wide Impact; Donald Berwick at the Brookings Institutions, October 18, 2010.
http://www.brookings.edu/~/media/Files/events/2010/1018_health_innovation/20101018_health_innovation_keynote.pdf.
xiv
Consumers and Health Information Technology: A National Survey; April 2010, California HealthCare Foundation.
http://www.chcf.org/publications/2010/04/consumers-and-health-information-technology-a-national-survey.
xv The Social Life of Health Information, 2011. Susannah Fox. Pew Research Center, May 2011,
http://www.pewinternet.org/Reports/2011/Social-Life-of-Health-Info.aspx
xvi Consumers and Health Information Technology: A National Survey; April 2010, California HealthCare Foundation.
http://www.chcf.org/publications/2010/04/consumers-and-health-information-technology-a-national-survey
.
xvii
Consumers and Health Information Technology: A National Survey, California Healthcare Foundation, April 2010.
http://www.chcf.org/publications/2010/04/consumers-and-health-information-technology-a-national-survey.
xviii
Achieving a Nationwide Learning Health System; Charles Friedman, Adam Wong, and David Blumenthal, Science Translational Medicine,
November 2010.
xix
The Digital Infrastructure for a Learning Health System: Foundation for Continuous Improvement in Health and Health Care -
Workshop Summary, Institute of Medicine, December 20, 2010.
xx
Grossman Claudia, Powers, Brian and McGinnis J. Michael, Digital Infrastructure for the Learning Health System the Foundation for Continuous Improvement in
Health and Health Care Series Summary, Roundtable on Values and Science-Driven Health Care, The Institute of Medicine’s Board on Studies under the
IOM Executive Office, Released May 23, 2011
Federal Health IT Strategic Plan 79
xxi
The Digital Infrastructure for a Learning Health System: Foundation for Continuous Improvement in Health and Health Care -
Workshop Summary, Institute of Medicine, December 20, 2010.
xxii
Designing a Digital Future: Federally Funded Research and Development Networking and Information Technology, President’s Council
of Advisors on Science and Technology, December 2010.
“Spotlight on Health Outcomes” Citations
Goal I: Use of EHRs provides information that can contribute to reducing heart attacks
1. P
ersell SD, Kho AN, Thompson JA, Baker DW. Improving hypertension quality measurement using electronic health records. Med Care.
2009 Apr;47(4):388-94.
2. Persell SD, Dunne AP, Lloyd-Jones DM, Baker DW. Electronic health record-based cardiac risk assessment and identification of unmet
preventive needs. Med Care. 2009 Apr;47(4):418-24.
G
oal I: Use of EHRs to perform medication reconciliation can contribute to reducing preventable hospitalizations
1. Br
ownstein JS, Murphy SN, Goldfine AB, Grant RW, Sordo M, Gainer V, Colecchi JA, Dubey A, Nathan DM, Glaser JP, Kohane
IS.Brownstein, et. al. Rapid Identification. Rapid identification of myocardial infarction risk associated with diabetes medications using
electronic medical records. Diabetes Care. 2010 Mar;33(3):526-31. Epub 2009 Dec 15.
G
oal II: Health IT can help enable information sharing to contribute to improving care coordination and reducing heart attacks
1. P
ersell SD, Kaiser D, Dolan NC, Andrews B, Levi S, Khandekar J, Gavagan T, Thompson JA, Friesema EM, Baker DW. Changes in
Performance After Implementation of a Multifaceted Electronic-Health-Record-Based Quality Improvement System.Persell Article. Med
Care. 2011 Feb;49(2):117-125.
G
oal II: Health IT can help provide information to enhance clinical decision making and can contribute to reducing preventable
hospitalizations
1. Be
rtoni AG, Bonds DE, Chen H, Hogan P, Crago L, Rosenberger E, Barham AH, Clinch CR, Goff DC Jr. Impact of a multifaceted
intervention on cholesterol management in primary care practices: guideline adherence for heart health randomized trial. Arch Intern Med.
2009 Apr 13;169(7):678-86.
2. Amarasingham R, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical
record data. Med Care. 2010 Nov;48(11):981-8.
G
oal IV: Empowering patients with health IT can contribute to reducing heart attacks
1. Scalvini S, Capomolla S, Zanelli E, Benigno M, Domenighini D, Paletta L, Glisenti F, Giordano A. Effect of home-based telecardiology on
chronic heart failure: costs and outcomes. J Telemed Telecare. 2005;11 Suppl 1:16-8.
G
oal IV: Empowering patients with health IT can contribute to reducing preventable hospitalizations
1. S
calvini S, Capomolla S, Zanelli E, Benigno M, Domenighini D, Paletta L, Glisenti F, Giordano A. Effect of home-based telecardiology on
chronic heart failure: costs and outcomes. J Telemed Telecare. 2005;11 Suppl 1:16-8.
2. Crossley GH, Boyle A, Vitense H, Chang Y, Mead RH; CONNECT Investigators. The CONNECT (Clinical Evaluation of Remote
Notification to Reduce Time to Clinical Decision) Trial The Value of Wireless Remote Monitoring With Automatic Clinician Alerts. J Am
Coll Cardiol. 2011 Jan 14.
G
oal V: A “learning health system” can contribute to reducing heart attacks
1. C
oloma PM, Schuemie MJ, Trifirò G, Gini R, Herings R, Hippisley-Cox J, Mazzaglia G, Giaquinto C, Corrao G, Pedersen L, van der Lei J,
Sturkenboom M; EU-ADR Consortium. Combining electronic healthcare databases in Europe to allow for large-scale drug safety monitoring:
the EU-ADR Project. Pharmacoepidemiol Drug Saf. 2011 Jan;20(1):1-11. doi: 10.1002/pds.2053. Epub 2010 Nov 8.
G
oal V: A “learning health system” can contribute to reducing preventable hospitalizations
1. A
marasingham R, et al. An automated model to identify heart failure patients at risk for 30-day readmission or death using electronic medical
record data. Med Care. 2010 Nov;48(11):981-8.

Federal Health IT Strategic Plan 80
2. Friedman, Charles P., Adam K. Wong, and David Blumenthal. "Achieving a Nationwide Learning Health System." Science Translational
Medicine, 10 Nov. 2010. Vol 2.
