
Utah State Medicaid Health
Information Technology Plan
Version 2022 Final – 7.1
Submitted to CMS 05/04/2022
2
State of Utah Medicaid
Health Information Technology Plan (SMHP)
Table of Contents
Table of Contents ........................................................................................ 2
SMHP Revisions Table ................................................................................. 4
SMHP Introduction ...................................................................................... 5
Plan Purpose ...................................................................................... 5
How the SMHP is Organized ................................................................ 5
SMHP Plan Scope ........................................................................................ 5
Detailed Activities for Implementation ................................................. 5
Promoting Interoperability Program ..................................................... 5
HITECH Administrative Matching Funds ............................................... 8
Ongoing Initiatives ............................................................................. 9
SMHP Plan Background ............................................................................. 10
State HIE/HIT Governance Structure .................................................. 10
Current State HIE & HIT Initiatives ..................................................... 11
Current HIE/HIT Activities and Funding Sources .................................. 11
Utah Grant Funding Sources Table ..................................................... 12
Utah Health Resource and Services Administration Grants ................... 13
Other Current Complementary Activities ............................................. 13
Populations with Unique Needs .......................................................... 15
Utah Assumptions on Federal Dependencies ....................................... 16
SMHP Plan Development ........................................................................... 16
MITA Approach ................................................................................. 16
SMHP Workgroup .............................................................................. 20
Governance Review ........................................................................... 20
Utah’s “Historical” HIT Landscape ............................................................. 21
Governance Landscape ...................................................................... 21
Provider Landscape ........................................................................ 23
Adoption of Certified Electronic Record Technology ............................. 23
Medicaid Promoting Interoperability Payments .................................... 25
EHR Systems .................................................................................... 25
Broadband Initiatives ..................................................................... 27
Broadband Grants Received ............................................................... 27
Current Broadband Coverage ............................................................. 27
Broadband Challenges in Rural Areas ................................................. 28
HIE Challenges .................................................................................. 28
Public Health .................................................................................. 29
Legislative Landscape .................................................................... 30
Utah Medicaid Operations & Systems Support Landscape ............ 33
Appeals Process ................................................................................ 36
Payment Offset ................................................................................. 37
Audits ............................................................................................... 37
Recoupment process for payments ..................................................... 37
Other HITECH Funding Opportunities ................................................. 38
HITECH Funds to Promote HIE connections with Medicaid Providers..... 40
Pediatric Patient Portal ...................................................................... 40
Controlled Substance Medication Integration ....................................... 41
Newborn Screening ........................................................................... 42
Electronic Physician Orders for Life Sustaining Treatment (ePOLST) ..... 42
Falls Prevention ................................................................................. 43
3
Utah’s “Programmatic” HIT Landscape ...................................................... 43
Governance Landscape ...................................................................... 44
Provider Landscape ........................................................................... 44
Legislative Landscape ........................................................................ 44
Utah Medicaid Operations Landscape.................................................. 44
Promoting Interoperability Program Activities Table ............................. 46
Core Administration Activities Table .................................................... 47
Administration and Oversight ............................................................. 48
Sanctions & Licensing Verification ...................................................... 48
Hospital-Based Determination ............................................................ 49
Provider Attestation Overall Content Verification .................................. 49
AIU Verification ................................................................................. 53
MU Verification .................................................................................. 53
State Specific Changes to MU ............................................................. 53
Certified EHR Technology Verification ................................................. 54
Collection of MU Data ........................................................................ 54
Attestation Goals ............................................................................... 54
Final Environmental Scan ……………………………………………………………………56
Future Pursuits .....................................Error! Bookmark not defined.
Decomissioning the SLR and Other Cloesout Activities .......................... 58
Interoperability and Patient Access Rule Implementation ..................... 58
Death Certification............................................................................. 59
Social Determinants of Health ............................................................ 59
Other Strategic Health IT Goals .......................................................... 60
Applicable Road Maps & Work Flow Diagrams ........................................... 61
Attachments & References Not Hyperlinked .............................................. 61

4
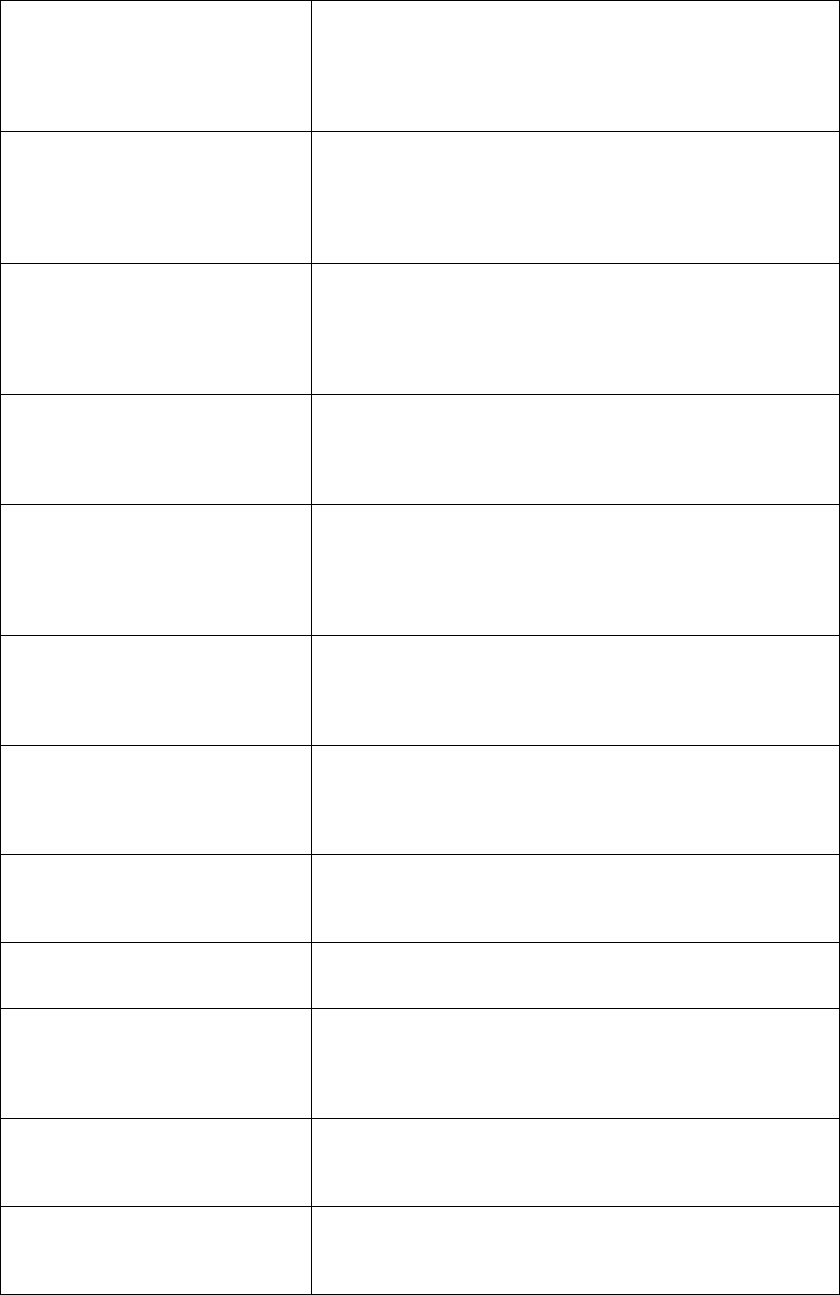
SMHP Revisions Table
This page is dedicated to providing a summary of the changes made to Utah State
Medicaid HIT Plan (SMHP) document.
SMHP Section
Description of Change
Date
Requested
by State
Date
Approved
by CMS
1.0 Original
Submission to CMS
12/23/10
1.1 Revised
CMS requested additional
information on appeals process
and hospital payments process
1/31/11
2.0 Original
Submission to CMS
11/22/2013
3.0 Original
Submission to CMS
11/01/2014
4.0 Original
Submission to CMS
09/30/2016
12/13/2016
4.1 Addendum
Stage 3 2015-2017 modifications
02/13/2017
04/25/2017
5.0 Original
Submission to CMS
06/30/2019
08/05/2019
5.1 Revised
CMS requested additional
information on HIT Landscape,
provider correspondence, state
systems, MITA, funding streams,
and audit strategy
09/25/2019
11/05/2019
6.0 Original
Annual update submission to CMS
12/16/2020
7.0 Original
Final update submission to CMS
3/31/2022

5
SMHP Introduction
Plan Purpose
This document represents an update of Utah’s State Medicaid Health Information
Technology Plan (SMHP). The overall purpose of the plan is to improve interoperability
across the continuum of care on behalf of Medicaid recipients. As a first step, the Utah
Department of Health Division of Medicaid & Health Financing (DMHF) has assumed
responsibility for administering an efficient Medicaid Promoting Interoperability (PI)
Incentive Payment Program to eligible providers and hospitals, thereby encouraging the
adoption of certified EHR technology to promote health care quality and the exchange
of health care information. In follow up to the EHR deployment to hospitals and eligible
providers, DMHF is moving towards the identification of other Medicaid providers who
have historically been ineligible for the Medicaid EHR Incentive Payment Program.
The primary focus of our SMHP is to continue engagement with eligible Medicaid
providers and facilities in order to improve coordination of care, electronic exchange of
information across the continuum of care, and provide an electronic infrastructure for
the development of HIT related population health applications through 2021. Utah is also
committed to carefully and appropriately executing closeout activities for this program,
as directed by the Centers for Medicare and Medicaid Services (CMS) in recent guidance.
How the SMHP is Organized
Various stakeholders from our community have provided input to this plan. The Utah
Department of Health DMHF will continue to work with stakeholders, thereby enabling
the pursuit of specific initiatives that encourage the adoption and meaningful use of
certified EHR technology and electronic exchange across the continuum for the
improvement of health care quality. This SMHP has been aligned with the recommended
sections identified in the SMHP companion guide as of June 2015 SMHP Overview
Template OMB Approval Number: 0938-1088. Guidance from the Final SMHP Template
dated June 2020 has also been consulted.
SMHP Plan Scope
Detailed Activities for Implementation
Based on the requirements defined in the Federal Regulation 42 CFR Parts 412, outlining
Medicare and Medicaid Program Electronic Health Record Incentive Program s and the
letter received February 29, 2016 (SMD#16-003) regarding the availability of HITECH
Administrative Matching funds, the State Medicaid HIT Plan is to provide CMS with details
regarding the necessary activities, processes and timelines for the proposed aims.
Promoting Interoperability Program
Utah developed and maintained the necessary systems to collect the attestations for the
first year’s Adopt, Implement or Upgrade (AIU) payments. Utah began accepting
meaningful use attestations in December 2012 for eligible hospitals and January 2013
for eligible professionals.
The key activities for Utah’s Promoting Interoperability Program are as follows:
1. Continue to interface with CMS regarding payments made to eligible providers
using their developed National Level Repository (NLR) system
2. Process payments on schedule and provide notification of approval/denial for
incentive payments
6
3. Maintain a Web site for Provider Registration and FAQs
4. Develop communication materials about the EHR Incentive Program and/or EHR
adoption/meaningful use
5. Conduct provider outreach activities
6. Staff a provider help-line and dedicated e-mail address/phone
7. Monitor and review current CMS policies, propose recommended changes or
inclusion of new policies and procedures, and develop and update FAQs
8. Validate volume thresholds, payment calculations, meaningful use, quality
measures, and provider credentials throughout the life cycle of the program
9. Analyze and report on program statistics regarding payments made, meaningful
use and clinical quality measures
10. Provide financial oversight and monitoring of expenditures to combat fraud
waste and abuse in the program
11. Provide financial oversight and monitoring of expenditures for Meaningful Use
Public Health Reporting partnerships
12. Public Health Registry activities to support providers in meeting Promoting
Interoperability Measures and the practical use of clinical registry data.
The EHR incentive program requested and received approval for funding to support meaningful
use activities with public health partners within the Department of Health in 2013. Funding in the
current IAPD approved September 16, 2020 supports the following meaningful use duties through
calendar year 2021:
Utah Statewide Immunization Information System (USIIS)
• Work with UDOH IT resources to specify and test enhancements to USIIS processing rules,
database structure and interface engine in order to meet Stage 3 requirements of bi-
directional interfaces, to include response to queries for evaluated immunization history
and forecast.
• Research, develop and unit test enhancements to USIIS data exchange infrastructure to
meet Stage 3 requirements of bi-directional interfaces, to include:
• Interface engine enhancements;
• HL7 2.5.1 message processing: interpreting received QBP message profile Z34
and responding with RSP message profile Z32 – for all possible scenarios;
• HL7 2.5.1 message processing: interpreting QBP message profile Z44 and
responding with RSP message profile Z42 – for all possible scenarios;
• Message exception and error handling; and
• Database writing.
• Support CQMs CMS 117v8 and CMS147v9 with enhanced system patient matching and
deduplication process, and develop provider portal to display metrics on patient population
immunization status.
• Work with EHR vendors to develop, test and validate new EHR-USIIS HL7 2.5.1
immunization interfaces.
• Manage and track on-boarding eligible hospitals and providers with EHR-USIIS HL7 2.5.1
immunization interfaces.
• Work with eligible hospitals and providers during on-boarding EHR-USIIS interfaces to
attain data quality compliant with Meaningful Use and to deploy their interfaces into
Production.
7
• Support eligible hospitals and professionals in their Meaningful Use registration for the
Immunization Public Health Measure and to provide notification of pass or fail.
• Run data quality reports and conduct data quality consulting for EHs and EPs registered
for Medicaid incentive programs with EHR-USIIS HLT 2.5.1 interfaces.
• Ensure that development and deployment of interface infrastructure comply with state
and department requirements with respect to software development, change
management, and security processes.
Informatics and Public Health Reporting
• Work with EHR vendors and state Department of Technology Services (DTS) to create
interfaces for the exchange of electronic data.
• Test and validate interfaces to ensure compliant ELR, syndromic surveillance, or case
reporting message.
• Aggregate incoming Syndromic Surveillance feeds from eligible hospitals.
• Create Syndromic Surveillance export for BioSense.
• Provide requirements for cCDA parsing and case report process development.
• Act as ELR Coordinator to manage and support meaningful use attestations for eligible
hospitals.
• Manage and track onboarding process.
• Perform data validation and quality assurance on data feeds from eligible hospitals and
providers.
• Manage ELR and case report exception queue.
• Fix message errors in HL7 messages and case reports.
• De-duplicate and merge HL7 messages.
• Create and provide attestation memos.
• Follow up with participants who have registered intent to participate to keep
work/progress moving forward.
• Implement and upgrade web-service and interfaces for EHs and EPs that have (or are in
process of) setting up public health reporting interfaces by creating interfaces in the Mirth
Interface Engine and setting up mappings for message structure and vocabulary.
• Coordinate regularly with UHIN as several EHs and EPs that report data are members of
the cHIE (UHIN) and UHIN sends the data feed to UDOH on behalf of the EH and or EP.
• Maintain UDOH MU public health reporting website.
• Maintain and enhance MU registration system as needed.
o Syndromic Surveillance specific activities, including: Create SyS export for the
BioSense-Essence (CDC managed SyS system).
o Coordinate with Syndromic Surveillance Epidemiologist in the Bureau of
Epidemiology to manage the SyS data feed going to BioSense-Essence.
o Act as SyS Coordinator to manage and support MU activities for EHs and EPs.
o Develop analysis, visualization, and reporting infrastructure for usage of SyS data.
• Electronic Laboratory Reporting specific activities, including:
o Import EHR local codes for each EH.
o Create mappings from local codes to master codes.
o Manage ELR messages processed into the Electronic Messaging Staging Area
(EMSA) application: Identify and fix message errors, deduplicate and merge
messages.
o Ongoing management of local and master vocabulary and code lists and rules
engine in EMSA.
o Develop analysis, visualization, and reporting infrastructure for usage of ELR data.
• Electronic Case Reporting (eCR) specific activities, including:
o Create data vocabulary mapping from eCR messages into EMSA and Utah’s
disease surveillance system.
o Design, develop, and implement the capacity to accept and process electronic
case reports for EHs and EPs as required by MU stage 3.
8
o Upgrade EMSA (including eCR specific rules engine) to automatically process MU
compliant case report messages.
o Enhance data model to accept additional data elements contained in case reports.
o Develop rules to accept and process MU compliant case report messages.
o Develop data matching and de-duplication process to merge case reports with
existing system data that are specific to case reporting.
o Develop analysis, visualization, and reporting infrastructure for usage of eCR data.
o Manage eCR messages in EMSA.
o Identify and fix message errors in eCR messages.
o De-duplication and merging of eCR messages.
o Provide guidance with the processing of eCR messages when manual review of
message is needed.
o Ongoing management local and master vocabulary and code lists.
o Ongoing management of eCR based rules engine in EMSA.
o Develop mapping to disease surveillance system.
• Develop data matching and duplication process to merge case reports with ELR messages.
• Implement and upgrade web service and interfaces for eligible provider and hospital
systems for ELR and Syndromic Surveillance.
• Create interfaces in the Mirth Interface Engine.
• Assist with on-boarding new facilities by mapping messages structure and vocabulary.
HITECH Administrative Matching Funds
In the past Utah has received two State Innovation Model (SIM) Design Grants from the
Center for Medicare and Medicaid Innovation (CMMI.) In 2013, Utah was awarded its
first State Innovations Model (SIM) Grant from CMMI to begin the process of putting the
previous policy discussions into action. The Utah SIM Executive Policy Group, led by Lt.
Governor Greg Bell, was the governing body of these Innovation efforts . This governing
body collaborated with 120 community leaders (business, the health care delive ry
system, health work force education, Utah’s mental health systems and government) to
continue the work that began at the 2011 Summit. During that phase, three use cases
were prioritized by the policy leaders to include behavioral health integration, obe sity
and diabetes reduction and advance care planning at the end of life.
In 2015, Utah was awarded a second SIM Model Design grant ($2 million) to develop a
State Health Systems Innovation Plan. A draft of that plan was submitted to CMMI July
31, 2016. The plan is organized around the three prioritized cases identified above and
focuses on six infrastructure issues, one of which is Health Information Technology.
Recommendations and priority projects from the SIM work are being integrated into this
SMHP as deemed appropriate.
The key activities for HITECH Administrative Matching Funds are as follows:
1. Identify list of potential HIT projects .
2. Prioritize according to SIM recommendations.
3. Identify Fair Share of Medicaid population impacted .
4. Identify list of Medicaid providers who were not eligible for MU incentive program .
5. Identify source of matching funds.
6. Develop cost analysis for individual projects .
9
7. Develop IAPD application for each of the projects .
8. Secure matching funds.
9. Submit IAPD for each of the projects.
We believe that appropriate business processes, staffing, and system s support are in
place to ensure continued success with these key activities .
Ongoing Initiatives
As recognized by CMS, continued development of the SMHP is an iterative process and
the Utah Department of Health DMHF is committed to updating the plan. Our plan is to
continue with the successful administration of incentive payments for all stages of the
program, and to support and encourage continued participation in the program in Utah’s
provider community. Additionally, we are seeking to integrate the SIM recommended
HIT projects as they are identified and are consistent with the HITECH Administrative
Funding opportunities.
The decision to pursue each of these initiatives is contingent upon continued
coordination with our community partners and will be referenced in future iterations of
Utah’s SMHP & IAPD. Some of the ongoing initiatives and identified proje cts are listed
below:
1. Require all providers receiving incentives to connect with public health
databases in an effort to meet meaningful use (i.e. laboratories, immunization
registry, etc.).
2. Continued Development and expansion of the Department of Health Master
Patient Index (DOHMPI).
3. Initiate an independent evaluation of the EHR incentive program .
4. Implement a quality assurance program for Utah’s fee for service providers .
5. Coordinate efforts of the State’s Digital Health Services Commission who has
assumed the role of the HIT Governance Consortium.
6. Collaborate with other neighboring states HIE’s (i.e. ID, WY, NV, AZ, CO, MT
etc.). Utah’s cHIE has operational connections with HIEs in CO, OR, ID, NV,
AZ, NE, OK, AR, MI, IN, IA, KY , ND, WV, MD, SC, LA, OH and AL. Utah cHIE is
partially connected to systems in CA, WA, MT, TN, TX and WY.
7. Develop and support IAPD applications as determined to be appropriate
through the application of HITECH.
8. Work with neighboring states including Idaho, Nevada, and Arizona on cross-
state line interoperability criteria
10
SMHP Plan Background
State HIE/HIT Governance Structure
The Utah Department of Health DMHF has worked closely and collaboratively with HIT
stakeholders throughout our State. They are an engaged group of stakeholders assisting
DMHF to increase EHR adoption and utilization in Utah. Multiple entities compose this
stakeholder group, each contributing to the task of improving healthcare in Utah through
the use of EHRs.
Currently Dr. Navina Forsythe, PhD, MPA is the Director for the Center for Health Data
and as the lead staff for the Governor-appointed Utah Digital Health Service Commission.
The Digital Health Services Commission is a governor -appointed statutory policy advisory
body. Its mission is to facilitate and promote the adoption and secure and efficient use
and exchange of electronic health information as a means to reduce healthcare costs,
enhance quality, increase access, and improve medical and public health services. The
Digital Health Services Commission coordinates strategically with many partners to
advance Health IT strategic goals and Objectives.
Utah Health Information Network (UHIN) is a non-profit group dedicated to the secure
use of healthcare data and the creation of software solutions for the healthcare
community. UHIN offers a full-service clearinghouse, operates Utah’s clinical Health
Information Exchange (cHIE), and provides analytics and business intelligence. UHIN is
a source of healthcare education events and other training opportunities for the
healthcare community. The Utah Department of Health and Utah State Medicaid have
representatives that serve on the UHIN Board of Directors.
The Utah Partnership for Value-Driven Health Care is a regional health improveme nt
collaborative comprised of multiple healthcare stakeholders including payers,
purchasers, and providers. This partnership aims to advance higher value healthcare in
Utah. Some current high-priority focuses of this group include advanced care planning,
healthcare affordability, aligning quality metrics for medical professionals, and
transparency. Several different workgroups work to address specific topics of importance
within the Utah healthcare community.
The Utah PI Program gets significant collaborative support from coordination with other
states who have also implemented the CNSI eMIPP state level registry. Michigan, Illinois,
Washington and Utah regularly discuss technical issues and best practices. States share
information on CMS interpretations of final rules and discuss implementation strategies
for system or program changes. Since these states share the same core product, the
work and cost of functionality upgrades or CMS-mandated updates to measures or other
participation requirements can be shared among all states.
PI Program staff meets periodically with public health staff. Working closely with Utah’s
immunization registry, syndromic surveillance, electronic laboratory reporting, and
clinical data repository group streamlines the process of co nfirming provider participation
and progress towards public health reporting measures.
According to UHIN’s website, the CHIE now has over 100 million clinical messages for
over 7.24 million unique patients. Connections are in place to receive data from 95%
of hospitals and 90% of large clinics in Utah. They also confirm 236,000 Clinical
Summaries pulled from the HIE in July 2020 and 786,000 CHIE Alerts in that same
month. (CHIE Alerts provide notifications when a patient is admitted to, or discharged
from a hospital or emergency department.)
Utah’s cHIE is a statewide entity. It is a 501c3 not -for-profit organization. The main
business model is a full-service clearinghouse. UHIN became an HIE in 2009. The cHIE

11
established connections with HIE partners in Arizona and western Colorado to form a
Patient-Centered Data Home. This allows providers from any of the three HIEs to get
notifications and patient summaries when their patients have an encounter across state
lines.
Current State HIE & HIT Initiatives
While many HIT initiatives in Utah are relatively mature, we realize a great deal of work
remains to advance the statewide use of HIT and clinical health information exchange.
The Utah Health IT Strategic Plan (2016-2020) details our strategic goals, objectives,
current and planned efforts to promote a sustainable statewide HIE architecture for
improved quality, efficiency, and reduced health care costs. This plan is being followed
by all of the Digital Health Services Commission partners and stakeholders in order to
provide consumers and their health care providers with credible, secure , and accurate
health information at the lowest possible cost. A list of HIT initiatives coordinated
across the Utah community and mapped to the Office of the National Coordinator (ONC)
can be found in the Attachments section (USIM Grant and Strategic Plan.)
Utah’s approach to HIT has been based on statewide cooperation and regional sharing,
strong executive leadership, and legislative reforms. This history, along with a relatively
high penetration of EHR and Hospital Information Management Systems (HIMS), has
enabled a market-driven HIE. Based on information from the Health IT Dashboard, an
estimated 85% of all outpatient primary care practices in Utah have adopted certified
EHR systems. This is slightly above the national average of 80%.
Current HIE/HIT Activities and Funding Sources
The State of Utah has received more than $45 million dollars in state and federal funding
to support our current HIE and HIT initiatives. When the initial SMHP was written in
2010, the following tables were representative of the funding received. This table has
been made current as of 2020.
Utah Medicaid maintains separate coding strings to separate the different funding
sources for regular MMIS funding and HITECH funding. All HITECH/HIE programs are
assigned individual Units to identify the specific HITECH project and program code S9I*
(followed by the federal fiscal year). Program code S9I* indicates the enhanced 90/10
match for HITECH. MMIS expenses are recorded using program codes that start with X**
and then vary depending on the federal match they qualify to receive. These Units an d
their program codes are monitored for incorrect coding, as well as MMIS expenses that
may have incorrectly received an invalid program code. The state ’s accounting system,
FINET, is set up to require a valid Unit and matching program code when transactio ns
are initiated. HITECH units only accept S9I* program codes, and MMIS units don't allow
program codes starting with S9I*. Reports are generated regularly to identify any
expenditure coding strings that aren't consistent with predetermined coding criteri a.
12
Utah Grant Funding Sources Table
Grant #1: Beacon Community
Grant awarded to HealthInsight –
Utah’s Regional Extension Center
Funding Amount = $15,790,181
In 2010, Utah received a Beacon Community Grant from the
ONC for HIT. The focus of this grant will be to improve adult
diabetes care management in Salt Lake, Summit and Tooele
Counties, by increasing availability, accuracy and transparency
of quality reporting, connecting providers to the State’s HIE
and fostering better collaboration with community partners.
Grant #2: ARRA Regional Extension
Center Technical Assistance
awarded to HealthInsight – Utah &
Nevada’s Regional Extension Center
Funding Amount = $6,917,783
In 2010, as the Regional Extension Center for Nevada and
Utah, HealthInsight provides federally-subsidized technical
assistance on a priority basis with physician office practices to
offer hands-on, one-on-one customized assistance selecting
and effectively using electronic health records to improve care.
Grant #3: State Health Information
Exchange Cooperative Agreement
Program awarded to the Utah
Department of Health
Funding Amount = $6,296,705
In 2010, the Utah Department of Health received this funding
to build upon existing efforts to advance regional and state-
level health information exchange while moving toward
nationwide interoperability. The majority of this funding was
sub-contracted to UHIN, the state’s designated clinical health
information exchange vendor.
Grant #4 CHIPRA Quality
Demonstration Grant awarded to
the Utah Department of Health
Funding Amount = $10,277,360
In 2010, The Utah Department of Health received this funding
to use HIT to coordinate care for children in Utah & Idaho
through Medical Homes and share immunization data between
both States’ HIE’s.
Grant #5 HRSA Public Health
Clinical Information Exchange with
Providers
Funding Amount = $1,200,000
In 2009, UHIN, the University of Utah and the Utah
Department of Health collectively applied for and received
funding to develop Utah’s Newborn Screening Clinical Health
Information Exchange which will allow users to share test
results of newborn hearing and blood screenings with a child’s
primary care medical home.
Grant #6 NIH – Statewide Master
Patient Index (MPI) for Health
Funding Amount = $2,000,000
In 2009, a research grant was issued to the University of Utah,
Intermountain Health Care, Utah Department of Health and
UHIN to develop and pilot a better framework for a statewide
MPI to enhance the capacity of the cHIE and better support
healthcare treatments, payments and public health uses.
Grant #7 Department of Agriculture
Broadband Availability Survey
Funding Amount = $300,000
In 2009, the Utah Department of Technology Services received
funding to conduct a survey in places where broadband is
unavailable and create opportunities for collaboration at a
community level to use HIT and information exchange to
achieve health care gains.
Grant #8 CMS Medicaid Meaningful
Use Planning Grant
Funding Amount = $400,000
In 2010, Utah Medicaid received a planning grant to develop
the SMHP and IAPD to administer EHR incentive payments for
the meaningful use of EHR’s and clinical information exchange.
Grant #9 ONC – Health IT
Workforce Development
Funding Amount = $3,364,798
In 2010, Salt Lake Community College, with eight other states,
received funding to develop and promote health information
non-degree training opportunities for health IT professionals.
Grant #10 CMS/CMMI – State
Innovation Model planning grant
Funding Amount = $$942,4582
This Round 1 model design grant afforded Utah to gather
policy leaders around the core infrastructure issues and
examine the evidence. This effort resulted in the prioritization
of three use cases (behavioral health integration, obesity and
diabetes reduction, and advance care planning at end of life).
Grant #11 CMS/CMMI – State
Innovation Model design grant
Funding Amount = $2,000,000
A second round of funding for model design work has resulted
in a set of specific recommendations addressing 6
infrastructure issues associated with the three prioritized use
cases.
Grant #13 ONC – Community
Health Information Exchange
Funding Amount = $100,000
UDOH, UHIN and Intermountain developed the electronic
exchange for the newborn hearing screening results and
follow-up diagnostic reports between providers, HIE and public
health program.
13
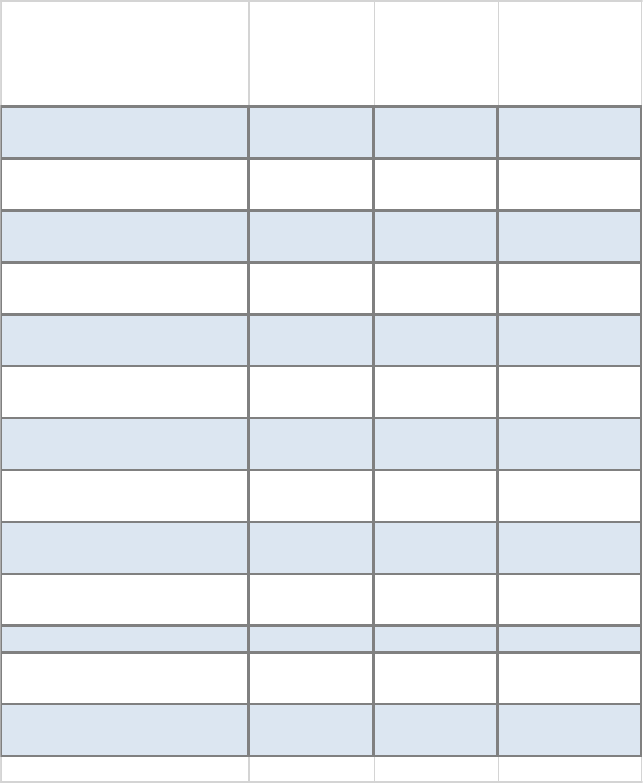
Utah Health Resource and Services Administration Grants
A number of Federally Qualified Health Centers (FQHCs) across the State received funding from
HRSA in 2018. The funds are set aside for the United States Department of Health and Human
Services (US DHHS) HRSA under the ARRA to expand healthcare services to low-income and
uninsured individuals through its health center program. These grants will support ongoing and
expanded EHR implementation projects in addition to HIT enhancement projects. The project goals
include improved healthcare quality, efficiency, and patient safety achievements through the use
of technology. No recent updates to this funding are available at the time of this submission.
HEALTH CENTER GRANTEE
EHR
REPORTERS
1
CLINICAL
QUALITY
IMPROVERS
2
ADVANCING
HEALTH
INFORMATION
TECHNOLOGY
3
BEAR LAKE COMMUNITY
HEALTH CENTER, INC.
$5,000 $0 $6,000
CARBON MEDICAL SERVICE
ASSOCIATION, INC.
$5,000 $9,326 $4,000
COMMUNITY HEALTH
CENTERS, INC.
$0 $52,001 $6,000
ENTERPRISE VALLEY MEDICAL
CLINIC, INC.
$5,000 $18,284 $6,000
GREEN RIVER MEDICAL
CENTER
$5,000 $0 $6,000
MIDTOWN COMMUNITY
HEALTH CENTER
$5,000 $0 $6,000
MOUNTAINLANDS
COMMUNITY HEALTH CENTER
$5,000 $19,309 $6,000
PAIUTE INDIAN TRIBE OF
UTAH, THE
$5,000 $15,771 $5,000
SOUTHWEST UTAH
COMMUNITY HEALTH CENTER
$5,000 $15,878 $6,000
UTAH NAVAJO HEALTH
SYSTEM, INC.
$5,000 $17,437 $6,000
UTAH PARTNERS FOR HEALTH $5,000 $22,569 $6,000
WASATCH HOMELESS HLTH
CARE/4TH ST. CLINIC
$5,000 $10,604 $3,000
WAYNE COMMUNITY HEALTH
CENTERS, INC.
$5,000 $13,186 $4,000
1
EHR Reporters employed EHRs to report on all CQM data for all of the health center's patients
2
Clinical Quality Improvers made at least a 10% improvement in one or more CQMs between 2016
and 2017
3
Advancing HIT for Quality Awards recognize health centers that utilized HIT systems to increase
access to care and advance quality of care.
Other Current Complementary Activities
The robust HIT infrastructure Utah has built will optimize our ability to access accurate
information on health care quality indicators. This information supports transparency of
quality and cost, which can be used for health payment reforms.

14
DMHF has funded the Center for Health Data and Informat ics’ Health Informatics
Program (HIP) through an IAPD to develop the Department of Health Master Patient
Index (DOHMPI). HIP has successfully completed the first use case to link the death
records with the Medicaid eligibility records and send the death no tification to Medicaid.
HIP is planning the DOHMPI next use cases such as death notification for Medicaid
providers or identity validation for Medicaid newborns.
From 2010-2013 the State of Utah advanced statewide use of HIT and clinical health
information exchange to improve health care quality and reform by using ARRA funds
awarded through the Statewide Health Information Exchange Program (UHIN), HIT
Regional Extension Center, and Beacon Community Program (Comagine.)
UHIN has issued over 4,000 health care providers a clinical health information exchange
(cHIE) user name and password to exchange clinical health information for treatment
purposes at the point of care. They have expanded cHIE services to include electronic
prescribing, laboratory orders and results delivery, and medical history to support
meaningful use. They have developed a sustainable governance and business model to
operate the cHIE and have plans to integrate public health data exchange with clinicians
thereby reducing the burden on providers, increasing timely and complete reporting for
population health.
Comagine (previously HealthInsight), is a Medicare Quality Improvement Organization
(QIO), functioned as the HIT Regional Extension Center (REC) for Utah , and serves as
the Agency for Healthcare Research and Quality (AHRQ) Chartered Value Exchange for
the state as well. They provided technical assistance, tools and resources to maximize
the use of CEHRT. They also counseled participating providers regarding retention of
appropriate records for future audit. HealthInsight provided on-site assistance to clinics
and consulted on vendor selection and system implementation. They also provided
assistance to current EHR users in workflow redesign, audit documentati on and
meaningful use. This arrangement through the ONC was from March 2010 to July 2016
and resulted in 852 Utah providers attesting for 90 days of meaningful use with either
the Medicare or the Medicaid incentive program. An additional 150 providers rece ived
assistance with the adoption/implementation/upgrade step of the program but hadn’t
yet achieved meaningful use. Grant assistance for this support declined. However,
HealthInsight remains an important resource for Utah EPs looking for assistance with
the Security Risk Assessment. The organization offered different levels of support with
this measure based on provider needs. HealthInsight staff guided EPs through HIPAA
self-assessment or provided a full-support remote risk analysis. HealthInsight partnered
with an award-winning privacy and security software solution called HIPAA One.
Utah Medicaid is a partner with the Utah All Payer Claims Database (APCD) managed by
the Office of Health Care Statistics. The APCD became operational in 2013 and receives
a monthly data feed amounting to approximately 50-65 million claims annually. The data
is from the private sector as well as Medicaid and provides a detailed resource for medical
researchers, public programs, and other authorized users. Utah’s APCD is able to analyze
episodes of care from statewide health insurance claims, allowing a view of the complete
course of patient care from initial diagnosis through treatment and follow -up. Utah’s
APCD is a robust source of data and is capable of answering questions such as:
• What was the patient’s diagnosis and treatment?
• When was the patient diagnosed and who made the diagnosis?
• Where did the patient receive treatment?
• How much did the patient’s care cost?
• Did the patient receive treatment expected by the standard of care?
• What is a patient or cohort’s risk profile?
15
All the contributing and necessary parties are aligned and have a common vision for how
HIE and HIT are implemented throughout the state of Utah. Utah’s Medicaid PI Program
will continue to be built upon this solid foundation and the program manager and staff
will help pursue initiatives that encourage the adoption of certified EHR technology and
audit for its meaningful use.
Populations with Unique Needs
The Utah PI program has benefited populations with unique needs in several ways. When
the CQM selections were expanded for program year 2014, providers had the option of
reporting on several new measures that were more applicable to pedi atric populations.
This change gave Utah pediatricians incentive to focus on meeting these measures and
allows clinics to focus on improving care for specific pediatric populations such as
children with asthma and children being treated with attention defi cit/hyperactivity
disorder medication.
See section “HITECH Administrative Matching Funds to Promote HIE connections with
Medicaid Providers” for details on the Pediatric Patient Portal project which is intended
to provide specific technical resources to the families of children with complex medical
conditions.
Utah Medicaid also has additional programs that focus specifically on the unique needs
of Utah children.
Children’s Health Insurance Program
The Children’s Health Insurance Program (CHIP) is a state health insurance plan for
children who do not have other insurance. It provides well -child exams, immunizations,
doctor visits, hospital, emergency care, prescriptions, hearing and eye exams, mental
health services and dental care. Preventative services (well-child visits, immunizations,
and dental cleanings) do not require a co -pay.
Child Health Evaluation and Care (CHEC)
CHEC is Utah’s Early and Periodic Screening, Diagnostic and Screening (EPSDT) program
for children ages birth through twenty who quali fy for Medicaid. It provides preventative
medical and dental care for children enrolled in Medicaid. Medicaid ensures that each
child has access to necessary check-ups. This program also encourages parents to
establish a medical home for their child.
Benefits include preventative physicals, hearing and vision screenings, mental health
care, as well as access to all necessary immunizations. If there are additional medical
concerns, CHEC works with the doctor to ensure the child is given appropriate and
necessary care. CHEC dental provides preventive care. This includes two dental
examinations per year, x-rays, sealants, fluoride and necessary restoration work.
Baby Your Baby
Baby Your Baby (BYB) is temporary medical coverage for low -income, pregnant women
who qualify. BYB covers pregnancy-related outpatient services provided by any Utah
Medicaid Provider. It does not cover the delivery of the baby. The goal of this program
is to reduce infant mortality by assisting Utah women to obtain early and frequent
prenatal care.
Autism Related Services
16
Autism related services are available to Medicaid patient under the age of 21 who qualify
for CHEC services. These services help develop, maintain or restore the functioning of a
person with an autism spectrum disorder (ASD). A service called Applied Behavior
Analysis (ABA) is available to assist with behavioral issues. In addition, there are other
types of services such as speech, occupational and physical therapy that may also help
a person with ASD.
Children’s Medicaid Waiver Programs
Several waiver programs are operated under the Utah Home and Community Based
Services which add specific benefits for pediatric populations:
Medically Complex Children’s Waiver. This program provides medical assistance to
children age 0-18 who are medically complex, and meet the following criteria: children
who have 3 or more specialty physicians, children who have 3 or more organ systems
involved in their disability, children who are not meeting age-appropriate milestones for
their activities of daily living, and children with a disability designation from the Social
Security Administration or from the State Medical Review Board.
Waiver for Technology Dependent Children. This program supports children and families
and ensures the availability of services and supports for technology dependent children
so that they can be cared for in their homes.
Utah Assumptions on Federal Dependencies
This section includes the assumptions where the path and timing of Federal initiatives
and plans have dependencies based upon the role of CMS (e.g., the development and
support of the R&A System), ONC or other federal organizations.
The Utah Department of Health (UDOH) is dependent upon federal CMS for the review
and approval of all SMHPs and IAPDs submitted to request federal funding for the Utah
Medicaid PI Program. UDOH relies on federal CMS to maintain the Registration and
Attestation System as operational support for provider participation in the program. The
agency is also dependent on funding used for contractual support of outreach and
application development services.
UDOH is also dependent upon federal CMS and the ONC for the distribution and
clarification of the Final Rule regarding the Utah PI Program and MU criteria. Finally
UDOH is dependent upon the ONC for the certification requirements of EHR systems so
that Utah providers can ascertain that they are utilizing CEHRT .
SMHP Plan Development
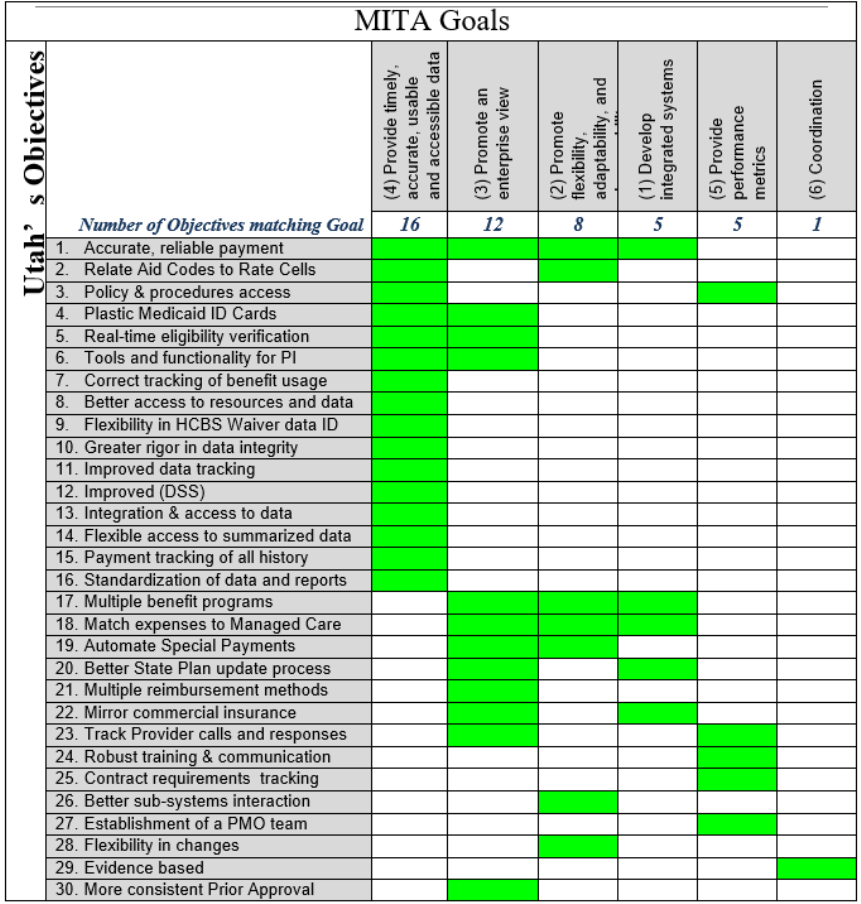
MITA Approach
Utah assumed a Medicaid Information Technology Architecture (MITA) approach to
determine the “Historical” (formerly known as “As-Is”) and the “Programmatic” (formerly
known as “To-Be”) HIT landscape and has created a roadmap for the
administration/oversight of the HIT incentive program. The SMHP Overview Template
was followed in great detail and was critical in assisting the planning team.
Critical Milestone
By
Initiated Internal Review of SMHP & IAPD
December 2, 2010
Submitted I-APD & SMHP to CMS – Version 1.0
December 31, 2010
Hired/Designated Program & DTS Staff
January 31, 2011
Created System Technical Requirements for Making Payments
February 28, 2011
17
Received I-APD & SMHP approval from CMS
February 28, 2011
Designed & Developed System for Making Payments
March 31, 2011
Completed Integration Testing
May 30, 2011
Completed Issue(s) Resolution
June 30, 2011
Conducted Provider Outreach, Trained & Implemented Regarding
the Application Process
June 30, 2011
Hired/Designated Remaining Program Staff
July 31, 2011
Accepted Applications for EHR Incentive Payments from
Providers
September 1, 2011
Made First Set of EHR Incentive Payments to Providers for AIU
November 18, 2011
Made First Set of EHR Incentive Payments to Hospitals
December 16, 2011
Developed System Definitions & Requirements for Meaningful
Use Stage 1
January 1, 2012
Submitted Revised IAPD – Version 2
July 1, 2012
Created System Technical Requirements for Meaningful Use
Stage 1
May 15, 2012
Designed & Developed System for Making Payments for
Meaningful Use Stage 1
December 7, 2012
Completed Integration Testing
November 15, 2012
Completed Issue(s) Resolution
November 28, 2012
Submitted & Received a SMHP Amendment for Meaningful Use
Stage 2 Rule Changes for 2013 (in attachments section)
January 23, 2013
Made first MU incentive payments to hospitals
February 1, 2013
Made first MU incentive payments to providers
March 8, 2013
Submitted audit strategy and approved (in attachments section)
May 30, 2013
Submit Revised I-APD – Version 2.0
September 16, 2014
Submit Revised SMHP Version 3.0
November 1, 2014
Create System Technical Requirements for Meaningful Use Stage
2 for 2014 Implementation
August 7, 2014
Submit updated audit strategy Version 3.2
9/30/2014
Design & Develop System for Making Payments for Meaningful
Use Stage 2
April 1, 2015
Make Stage 2 MU incentive payments to providers
April 1, 2015
Make Stage 2 MU incentive payments to hospitals
April 1, 2015
Submit revised IAPD Version 3.0
November 6, 2015
Replace current Oracle Solution with CNSI’s HIT Incentive
Product eMIPP
July 1, 2016
Launch approved screens for 2015 Modified Stage 2
requirements – EH
July 1, 2016
Launch approved screens for 2015 Modified Stage 2
requirements – EP
July 1, 2016
Plan and develop IAPD projects according to Medicaid criteria,
SIM priorities and matching funds opportunity
September - December
2016
Submit updated SMHP version 4.0
September 2016
Request for Proposal through state purchasing process to solicit
a program auditor
December 2017 –
March 2018
Launch approved changes to SLR mandated by OPPS final rule
dated 10/14/16
March 2018
Submit series of IAPD amendments staged according to priorities
January 2017-2021
Operationalize IAPD initiatives
January 2017-2021
Submit serious of IAPD amendments staged according to
priorities
January 2017-2021
18
Request for Proposal through state purchasing process to solicit
a program auditor
December 2017 –
March 2018
Launch approved changes to SLR mandated by OPPS final rule
dated 10/14/16
March 2018
Submit revised IAPD
August 21, 2018
Develop and Submit Audit Strategy
March 2019-July 2019
Implement SLR changes mandated by 2019 IPPS rule
June 27, 2019
Submit revised SMHP Version 5.0
June 30, 2019
Submit Audit Strategy Version 4.0 for CMS review
July 30, 2019
Submit IAPD-U
August 7, 2019
Make Stage 3 Meaningful Use Payments
February 2020
Submit HIE Project update IAPD
November 2019
PFS and IPPs Updates to eMIPP
June 29, 2020
Submit IAPDU
July 30, 2020
Submit updated SMHP Version 6.0
December 2020
Submit updated Audit Strategy
December 2020
Submit final SMHP Version 7.0
March, 31 2022
Submit final Audit Strategy
March 31, 2022
Utah Medicaid completed a full Medicaid Information Technology Architecture State self -
assessment (MITA Framework 2.0) in December 2008. This was an important evaluation
to take place at the beginning of discussions regarding replacement of the legacy MMIS.
The Division determined that the replacement MMIS must meet the following general
objectives:
• The MMIS must align with Federal and State laws, regulations, and guidelines .
• The MMIS must “work” from a functional perspective and must adhere to the
requirements defined by the Division.
• The MMIS must be flexible, adaptable, and responsive (timeliness and ease of
change).
• The MMIS must be supported by an adequate (appropriate) change control
environment.
• The architecture for the MMIS must support a rules-based environment.
• The MMIS must support the elimination, reduction, or automation of manual
processes.
• The architecture for the MMIS must allow for the integration of software/systems
that support business needs.
• The MMIS must provide accurate, meaningful, and timely reporting.
• The MMIS must be implemented in a timely manner consistent with a robust, well -
maintained project plan.
• The MMIS must support evidenced-based outcome functionality.
Based on these requirements a number of functional objectives were identified. These
functional objectives are guiding principles for the functionality required of the CNSI
PRISM MMIS.
Functional objectives:
19
On February 2, 2012 The Utah Department of Health received approval from CMS for
both the IAPD securing enhanced federal funding and the Request for Proposal (RFP) for
the core system replacement. In August 2012 the Department named CNSI as the
successful bidder.
The Department named the new MMIS “PRISM” (Provider Reimbursement Information
System for Medicaid). Requirements validation and design are ongoing for this enormous
project, and progress has been made in a series of releases.
20
The completed major releases as of 8/30/2020 are summarized below:
March 2014 Release 1 – New Medicaid website and Eligibility Lookup Tool
August 2014 Release 2 – HealthBeat Data Analytics Dashboard Tool
July 2016 Release 3 – Provider Enrollment and Electronic Medicaid Incentive Payment
Program (eMIPP)
June 2020 Release C1 provided enhancements to the Provider Enrollment system and
migrated the existing functionality including eMIPP to a cloud-based environment.
By 2023, full functionality including claims processing will be live in the PRISM cloud
product. At this time the state will pursue full certification of the MMIS, and a full MITA
State Self-Assessment will be completed.
SMHP Workgroup
In the planning process, the Utah Department of Health DMHF sought out and
incorporated input for the following stakeholder organizations :
1. Association of Utah Community Health Centers (AUCH) is the primary care association for
Utah whose members include Bureau of Primary Health Care (BPHC) grantees and other
providers who strive to meet the needs of the medically underserved.
2. HealthInsight, now Comagine, is a Medicare Quality Improvement Organization (QIO) and
HIT Regional Extension Center (REC) for Utah and serves as the Agency for Healthcare
Research and Quality (AHRQ) Chartered Value Exchange for the State as well. They host
our State’s HIT Task Force meetings, where grant and project managers from the State
HIE program, statewide clinical health information exchange (cHIE), Beacon Community,
Medicaid HIT Incentives and CHIPRA Quality Improvement Project meet monthly to
coordinate overlapping issues and project interdependency.
3.
Utah Health Information Network
(UHIN) is our statewide Health Information Exchange
infrastructure (HIE). A list of participating healthcare entities in UHIN’s Clinical Health
Information Exchange (cHIE) can be found in the Attachments section of this SMHP along
with a recent cHIE update that lists UHIN’s accomplishments, plans, risks and financial
status.
4.
Utah Hospital Association (UHA) represents member hospitals and all ten healthcare
systems operating in the State of Utah.
5.
Utah Department of Health Office of Public Health Informatics,
whose mission is to
coordinate and support Utah's e-health initiatives and to facilitate development of
systematic applications of information, statistics, and computer technology for Utah's
public health surveillance, health service and learning.
6.
Utah Department of Technology Services,
which is Utah’s consolidated IT resources
organization that provides technical support to our MMIS and other business operations.
Governance Review
The SMHP was reviewed by key Utah Department of Health and DMHF management prior
to submission to CMS.

21
Utah’s “Historical” HIT Landscape
Governance Landscape
The Utah Department of Health is the single State agency for the Medicaid and CHIP
programs. The Division of Medicaid and Health Financing serves as the Medicaid and
CHIP administrative agency within the Department of Health. All of Utah’s state-level
public health agencies also co-reside within Utah Department of Health.
The Utah Department of Health has the statutory responsibility to adopt standards for
the electronic exchange of clinical health information between healthcare providers and
third party payers that are for treatment, payment, healthcare operations, or public
health reporting, as provided for in 45 C.F.R. Parts 160, 162, and 164, Health Insurance
Reform: Security Standards. The Utah Digital Health Service Commission serves as an
advisory board regarding statewide health IT and clinical Health Information Exchange
(cHIE). Dr. Navina Forsythe PhD, MPA, Director for the Center for Health Data and
Informatics and the lead staff for the Digital Health Service Commission, has been
designated the State Health HIT Coordinator. Utah Medicaid participates in Utah Digital
Health Services Commission meetings on an ad hoc basis as needed.
The governor of Utah selects 13 members for this comm ission, with representatives from
the following areas:
(a) a physician who is involved in digital health service;
(b) a representative of a health care system or a licensed health care facility as that term is
defined in Section 26-21-2;
(c) a representative of rural Utah, which may be a person nominated by an advisory committee
on rural health issues created pursuant to Section 26-1-20;
(d) a member of the public who is not involved with digital health service;
(e) a nurse who is involved in digital health service; and
(f) eight members who fall into one or more of the following categories:
(i) individuals who use digital health service in a public or private institution;
(ii) individuals who use digital health service in serving medically underserved populations;
(iii) nonphysician health care providers involved in digital health service;
(iv) information technology professionals involved in digital health service;
(v) representatives of the health insurance industry;
(vi) telehealth digital health service consumer advocates; and
(vii) individuals who use digital health service in serving mental or behavioral health
populations.
Historically, the information technology professional involved in digital health service
((iv) above) is a representative from the Utah Health Information Network which
operates Utah’s health information exchange.
The State Health IT Coordinator and the Director for the State Innovation Model Design
Grant were given an opportunity to contribute to the SMHP. The Commission and SIM
grant has worked with the following partners and organizations.
Representing Organization Names
Government: Utah Department of Health, including Utah Medicaid Program, Utah
Department of Technology Services, Utah Department of
Insurance, State Office of Education, Veterans Administration Salt
Lake Medical Center, Utah Association of Local Health Officers,
Private: Utah Health Information Network
22
Clinical/Hospital: Intermountain Healthcare, University of Utah Health Sciences
Center, HCA/MountainStar Hospitals, Central Utah Clinic, Utah
Hospitals and Health Systems Association, Utah Medical
Associations, ARUP Laboratories
Insurers: Deseret Mutual Benefits Administrators, Public Employee Health
Plans, Regence Blue Cross Blue Shield, SelectHealth, Molina Health
Plans
Communities: Utah Chartered Value Exchange at HealthInsight, Association for
Utah Community Health, Utah Association for Home Health
Care/Utah Hospice and Palliative Care Organizations, Utah
Pharmacists Association, Utah Health Care Association, Utah
Telehealth Network and Utah Indian Health Advisory Board
Education & Research: University of Utah
Utah Medicaid was one of the founding organizations for UHIN and has participated in
UHIN’s governance since its founding in 1993. UHIN as previously mentioned is the
State’s designated HIE Vendor. They have a stat ewide geographic scope to support Utah
Medicaid in the HIT incentive project. UHIN is governed by a Board of Directors. Emma
Chacon, Medicaid Operations Director and Heather Borski, Deputy Director of the Utah
Department of Health both sit on the UHIN board and also serve on the UHIN Board
Executive Committee. The UHIN Board also has oversight over UHIN’s administration of
the cHIE.
UHIN is central to the State’s HIT & HIE initiatives and activities, including the exchange
of billing and clinical information. The Utah MMIS receives claim data from providers via
UHIN and provides Medicaid recipient data through UHIN for exchange with participating
providers. At this time, UHIN is in production for laboratory results delivery and initiating
a pilot for the query function. The Department of Health, Center for Health Data and
Informatics routinely convenes with UHIN and receives monthly updates. In addition, a
UHIN representative serves as one member of the Utah Digital Health Service
Commission in the capacity of an information technology professional involved in digital
health service.
In 2012, as the result of HB 141, all of Utah’s Medicaid and CHIP lives were opted in to
the state’s HIE. As of 12/31/2015 there were 446,641 CHIP and Medicaid lives enrolled in the
cHIE. An additional 2,651 members have requested to be opted out of the cHIE.
The USIIS Program supports the Health Information Technology Plan by working with
eligible providers (EPs) and eligible hospitals (EHs) in their efforts toward su bmitting
immunization data to USIIS, the Utah Statewide Immunization Information System.
USIIS supported Meaningful Use from its inception, providing
documentation/instructions, online registration, secure methods for submitting data and
status notices used by EPs, EHs and the Medicaid Program for attestation purposes. The
USIIS Program also worked with Electronic Health Record system vendors used by Utah
EPs and EHs to develop, test and approve for release HL7 interfaces that comply with
MU stages and goals. Advances attained during this time include implementing 40 new
interfaces for EHR systems used by Utah EPs and EHs and implementing three additional
secure transport methods—including submission via the Utah clinical health information
exchange (cHIE). The USIIS Program has assisted over 1,200 EPs and EHs through all
stages of Meaningful Use, and has on-boarded 236 EPs and 32 EHs for Stage 2/Modified
Stage 2. Furthermore, the USIIS Program has developed data quality reports and a
23
process to periodically provide data quality assessments and guidance to EPs and EHs
as they continue to submit immunization data to USIIS.
Our public health partners, including Electronic Laboratory Reporting, Syndromic
Surveillance, Immunization Reporting, and Cancer Registry Reporting developed a joint
website dedicated to Public Health Reporting for Meaningful Use . Electronic case
reporting is now an option on this site as well. This is a starting point for eligible
professionals and eligible hospitals to obtain information, technical specifications,
deadlines, and to register to conduct testing or exchange with these agencies. One
registration form is used for all areas. This process is in collaboration with Promoting
Interoperability Program within the Division of Medicaid and Health Finance.
In order to support ongoing efforts towards public health reporting and Meaningful Use,
the Promoting Interoperability program has entered into Memoranda of Understanding
with these public health partners, which will allow HIT funding to pay for our public
health partners’ staff time that is dedicated specifically to Meaningful Use. This is
detailed in Utah’s most recent IAPD. The registration process is for Utah Eligible
Professionals and Eligible Hospitals intending to apply for the Medicaid and/or Medicare
EHR Meaningful Use incentive programs for all meaningful use stages. The registration
process is managed online and can be accessed with the following link
http://health.utah.gov/meaningfuluse/
Provider Landscape
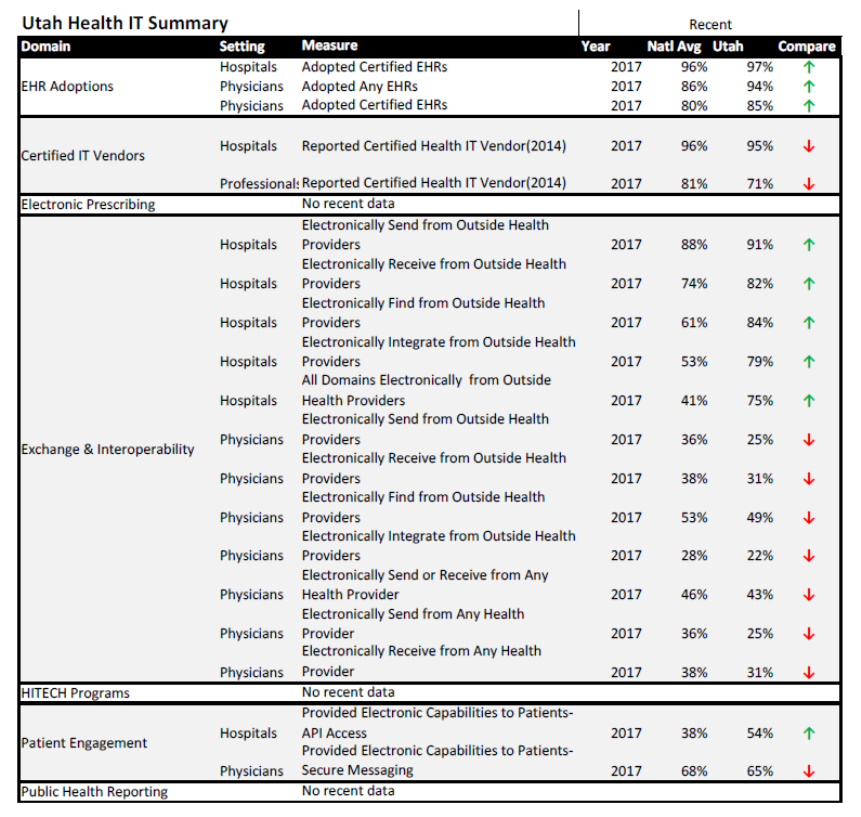
Adoption of Certified Electronic Record Technology
This table shows how Utah compares to the national average on measures of health
information technology adoption and utilization. Data was obtained from the Office of
the National Coordinator. Data below is from 2017 and is the most current dataset available
through the ONC. While Utah appears to be performing especially well regarding hospital adoption
of HIT, office physician adoption of HIT is slightly below the national average.
(https://dashboard.healthit.gov/apps/health-information-technology-data-summaries.php)
24
25
Medicaid Promoting Interoperability Payments
The following Utah providers and hospitals have received Medicaid PI payments for either
adopting, implementing or upgrading to certified EHR technology or for achieving
meaningful use
Utah has paid year one incentives to over 1100 unique EPs. Of these providers, 699
unique EPs have received at least one meaningful use payment. As of 12/31/2021, 218
EPs have received their sixth and final payment for participating in the program. For
eligible hospitals, 44 year one payments have been made and 43 hospitals from that
group have demonstrated meaningful use. Twenty-five of these hospitals have completed
all four years of the incentive program.
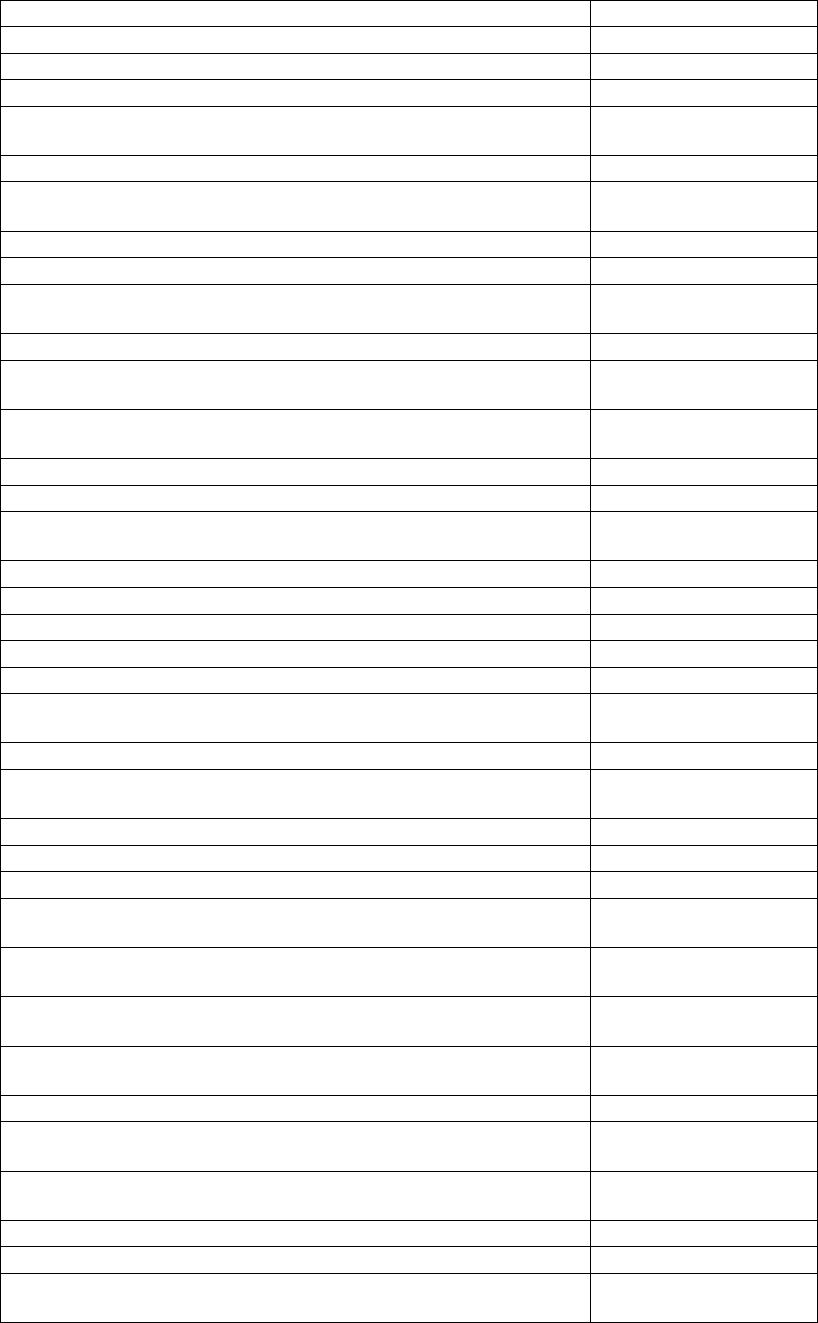
EHR Systems
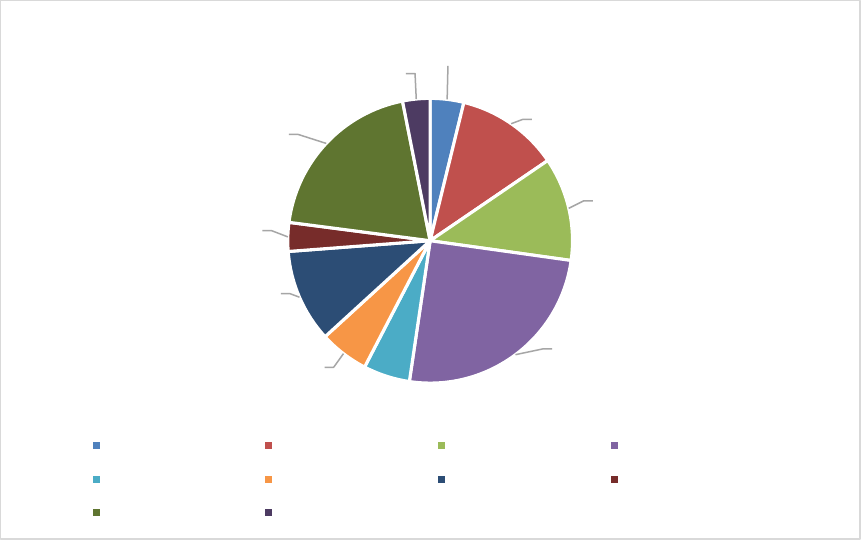
The chart below depicts the utilization of EHR Systems in use in the State of Utah. The
information was derived from attestations. Across the life of the program EPs have used
a wide range of certified EHRs, however as the meaningful use stages have progressed,
the bulk of program participants are tied to larger healthcare clinics and systems so we
see much less variety in the CEHRTs being used to attest. The CEHRT utilization for
program year 2019 shows this clearly. The two largest health systems in Utah, University
of Utah Healthcare and Intermountain Healthcare, use Epic and Cerner systems,
respectively.
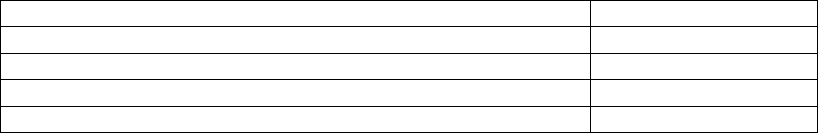
Year Total Payment Total Year Total Payment Total
2011 141 2,769,594.00$ 2011 9 6,311,660.00$
2012 320 5,720,518.00$ 2012 17 10,674,127.00$
2013 578 8,944,857.00$ 2013 39 21,508,546.00$
2014 567 6,614,451.00$ 2014 41 16,847,952.00$
2015 374 4,087,091.00$ 2015 14 3,096,693.56$
2016 319 4,000,673.00$ 2016 15 1,010,126.00$
2017 229 1,906,828.00$ 2017 11 618,096.00$
2018 284 2,382,837.00$ 2018 1 6,925.00$
2019 155 1,283,504.00$ 2019 1 6,925.00$
2020 147 1,229,669.00$ 2020 -- --
2021 106 889,668.00$ 2021 -- --
EP by Program Year
EH by Program Year
26
Attesting providers reported using over 40 different EHR products over the course of the
program, including some smaller, home-grown products. The majority of providers attesting for
later stages Modified Stage 2 and Stage 3 used Epic, Cerner, Athena Clinicals or eClinical Works.
Utah has made incentive payments to 44 unique eligible hospitals. Of these facilities, 23
belong to one large health system and use the Cerner product. The state’s other large
health system uses the Epic product. Smaller facilities have attested using Meditech,
Medhost, and Chart Access EHRs.
There are 12 Federally Qualified Health Centers (FQHC) in Utah, encompassing 29
different clinic locations. All of these FQHCs have adopted certified EHRs and all have
attested for incentive payments. Approximately 180 FQHC providers have received over
420 incentive payments. The program has seen a good return rate for these providers
with many providers receiving 4, 5, or 6 years of payments . FQHC dentists have really
benefited from the administrative support from their clinics’ participation in the incentive
program. FQHC dentists represent the bulk of the Utah’s dental meaningful users.
Utah’s Veterans Affairs Medical Center (VAMC) in Salt Lake City is a formal organizational
member of the UHIN and the cHIE project. The VAMC successfully completed a project
in partnership with UHIN that allows patient summaries to be exchanged bi -directionally.
The process is working well but does require two separate consents from the patient in
order for data to be exchanged. They have also been working on projects for direct
connection of home health information as well as the sharing of care plans.
Tribal participation in the Promoting Interoperability program remains very limited. Utah
Navajo Health Systems, the Paiute Indian Tribe of Utah and the Goshute Tribe of Utah
all had EPs who began participation in the PI program. However, participation from this
group has dwindled and the program does not expect to have any tribal healthcare
groups achieve Stage 3 meaningful use. Utah paid one tribal hospital as well, Blue
Mountain Hospital, which received 3 years of incentive payments.
AthenaClinicals Total
4%
Cerner Total
12%
eClinical Works Total
12%
Epic Total
25%
Epic Combo Total
5%
Greenway Total
6%
Help2 Total
10%
NextGen Total
3%
Other Total
20%
Practice Fusion Total
3%
CEHRT Products Over the Course of the Program
AthenaClinicals Total Cerner Total eClinical Works Total Epic Total
Epic Combo Total Greenway Total Help2 Total NextGen Total
Other Total Practice Fusion Total
27
Broadband Initiatives
Widespread broadband Internet capabilities are essential for the s uccess of HIE
implementation. The sections below describe a number of initiatives supporting the
expansion of Internet access across the State of Utah, enabling the healthcare
community’s ability to participate in HIE.
Broadband Grants Received
• Since 2010, The State of Utah Broadband Project has been awarded $5,196,025
in federal grants for Utah's Broadband Initiative.
• Another $31,048,683, accounting for 0.9% of all federal infrastructure grants,
was awarded to broadband infrastructure projects in Utah.
• Since 2011, access to a wired connection of at least 10mbps has improved
from 90.2% to 97.1% of Utahns.
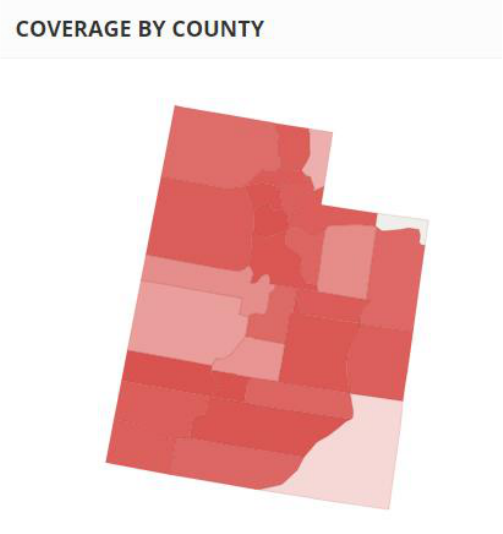
Current Broadband Coverage
According to BROADBANDNOW, 100% of Utahns have access to mobile broadband
service and 97.9% have access to fixed wireless service. There are now 13 9 broadband
providers in Utah. However, there are still geographic areas, where access to broadband
is more limited. Current gap statistics include:
• 108,000 people in Utah are without access to a wired connection capable of
25mbps download speeds.
• The population of Daggett County, Utah does not have any wired internet
providers available, and only 4% of county residents have access to 25mbps
download speeds.
• The population of San Juan County also has limited access to sufficient download
speeds, with only 25% of the county residents able to obtain 25mbps service.
• Another 45,000 people in Utah do not have any wired internet providers available
where they live.
A broadband speed of 25mbps or faster is accessible to 96.1% of Utahns, while 93.6%
have access to broadband of 100mbps or faster. Additionally, a broadband speed of 1
gigabit is accessible to 30.2% of Utahns, wireline service is accessible to 98.5%, fiber-
optic is accessible to 32.9%, cable is accessible to 90.7% and DSL is accessible to 96.3%.
Utah is rated as the 29th most connected state and averages 69.5mbps state-wide. More
information and statistics can be found at https://broadbandnow.com/Utah.
28
Utah’s Broadband: Stats & Figures BROADBANDNOW. Last updated September 1, 2020.
Broadband Challenges in Rural Areas
Given the infusion of broadband infrastructure and connectivity funding in recent years,
access to broadband internet is not a significant challenge to HIT or HIE in most rural
areas. There are pockets in rural Utah where broadband internet access is less affordable
due to limited connectivity options (fiber, wireless, or cable) and lack of competition due
to limited Internet Service Providers (ISP) in the territory. 11 of 29 counties in Utah have
only two ISPs, and one rural county has only one ISP.
HIE Challenges
Utah has a state-designated health information exchange called the Clinical Health
Information Exchange (cHIE.) The CHIE provides a patient -centric record that can be
accessed by disparate providers. cHIE services such as Admission/Discharge/Tr ansfer
alerts and Direct Secure Messaging are designed to help Utah healthcare providers
achieve interoperability. Though the count of Utah healthcare locations connected to the
cHIE continues to increase, a large proportion of locations do not invest fina ncially in
the advanced features of the HIE, or they lack awareness of the availability and benefits
of HIEs. Healthcare organizations like long term care and behavioral health have had
limited opportunities for connectivity subsidies and that makes afford ability among
certain health care sectors more challenging.
Internet access and acceptable speeds are not major issues affecting the Utah HIE;
however, the data being exchanged today is mostly summary only. Internet bandwidth
may become a greater challenge as bidirectional exchange increases, or as larger files
such as imaging results become more common.
Without a mandate or legislative requirement, creating a business case for HIE continues
to be an issue. Larger health systems have historically been re sistant to share data
outside of their networks and affiliations. Additionally, larger EHRs like Epic and Cerner,
29
associated with Utah’s two largest health systems, have the ability to function like an
HIE now and that can reduce the need/demand for a broa der based or statewide HIE.
Public Health
As part of demonstrating meaningful use, EPs and EHs must make connections with two
public health registries. In Utah several of these registries are housed within the
Department of Health in the Division of Disease Control and Prevention (DCP). The Utah
PI program has financially supported efforts by these public health partners to interface
with participating providers. The Utah Statewide Immunization Information System
(USIIS), Syndromic Surveillance Reporting, Electronic Laboratory Reporting (ELR) and
Electronic Case Reporting. These public health entities maintain a meaningful use
registration site for tracking registration, onboarding activities and active engagement.
Funding for certain activities performed by public health staff that support the PI
program have been budgeted into the current IAPD. Some activities that are funded to
support PI public health reporting are:
• testing, validating and maintaining interfaces ;
• working with EHR vendors to create and validate compliant HLT messages;
• data validation and quality assurance;
• tracking onboarding processes and progress;
• providing memos to confirm Active Engagement status for participating providers;
• maintaining a public health Meaningful Use website with a central registration for
all supported state registries;
• infrastructure enhancements to support new requirements for additional stages
of Meaningful Use such as bi-directional interfaces.
Utah is pleased with the results of these activities. Close part nerships with these
registries allow program staff to confirm compliance with these measures as part of pre -
payment verifications. The active engagement memos are uploaded to support the
meaningful use attestations. Other public health data achievements th at have been
supported as part of meaningful use are:
• USIIS has developed interfaces with 63 distinct EHR systems.
• Facility participation in immunization record reporting increased 57% from 2012 -
2016.
• Immunization records processed into USIIS via EHR interface have increased
429% from 2012-2016 and an additional 260% from 2016 to 2021.Adult
immunization records in USIIS have increased 126% from 2012 -2016.
• USIIS processes over 250,000 immunization history queries (an increase of over
400% from 2016) on a weekly basis as part of a bi-directional interface that was
mandated for Stage 3 Meaningful Use. This peaked to over 300,000 queries per
week during COVID. Approximately 35% of those queries included an
immunization forecast.
• Utah was the first state to implement Docket mobile phone app for consumer
access to immunization records. This application also supports the Smart Health
Card QR code standard, supporting COVID travel and immunization record
sharing.
• Reliability of EHR-USIIS connections has been increased by improving error
handling and automating many processes that had previously required manual
interventions.
• 36 hospital laboratories have been onboarded for electronic lab reporting and all
emergency departments in Utah have been onboarded for Syndromic
Surveillance.
• The percent of ELR messages added to the communicable disease surveillance
system has increased from 65% to 99%. This has allowed the program to reduce
30
manual data entry personnel by 2 full-time employees. Without ELR it would
have been impossible for us to collected the detailed level of information on
COVID testing, which has driven much of our intervention efforts and policies.
Syndromic surveillance can now track several diseases and injuries that they were
previously unable to track due to the low volume of data, including influenza,
COVID-19, opioid overdoses, firearm-related injuries and non-fatal suicide
attempts.
• Collection of negative lab test data allows insight into screening rates and
improves identification of false positive lab results.
• Surveillance data obtained electronically is timelier. For instance, DCP is now able
to monitor Influenza-Like-Illness data for influenza surveillance during the
influenza season and will allow for a larger component of monitoring COVID-19
activity as the state moves into the “Steady State” COVID response .
• Syndromic surveillance data related to opioid overdose can now be collected in
nearly real time which improves public health response to opioid events.
• Electronic case reporting partnerships with Utah’s largest hospital system are
actively collecting incidents of several disease conditions: Chlamydia, Gonorrhea,
Pertussis, Salmonella, and Zika virus and reports these results to jurisdictions as
well as notifying the initial reporter.
Legislative Landscape
Utah health policymakers acknowledge that health information technology (HIT) and
health information exchange (HIE) are two driving forces to transform health systems.
To ensure that health care reform leads to better health care, the Utah legislature passed
the following legislation to improve efficiency and quality of health care and reduce cost
since 2005. It was important to include bills since 2005 because of the continual impact
they have. To reinforce the importance of legislative bills as it pertains to HIT and HIE,
the following table is being provided:
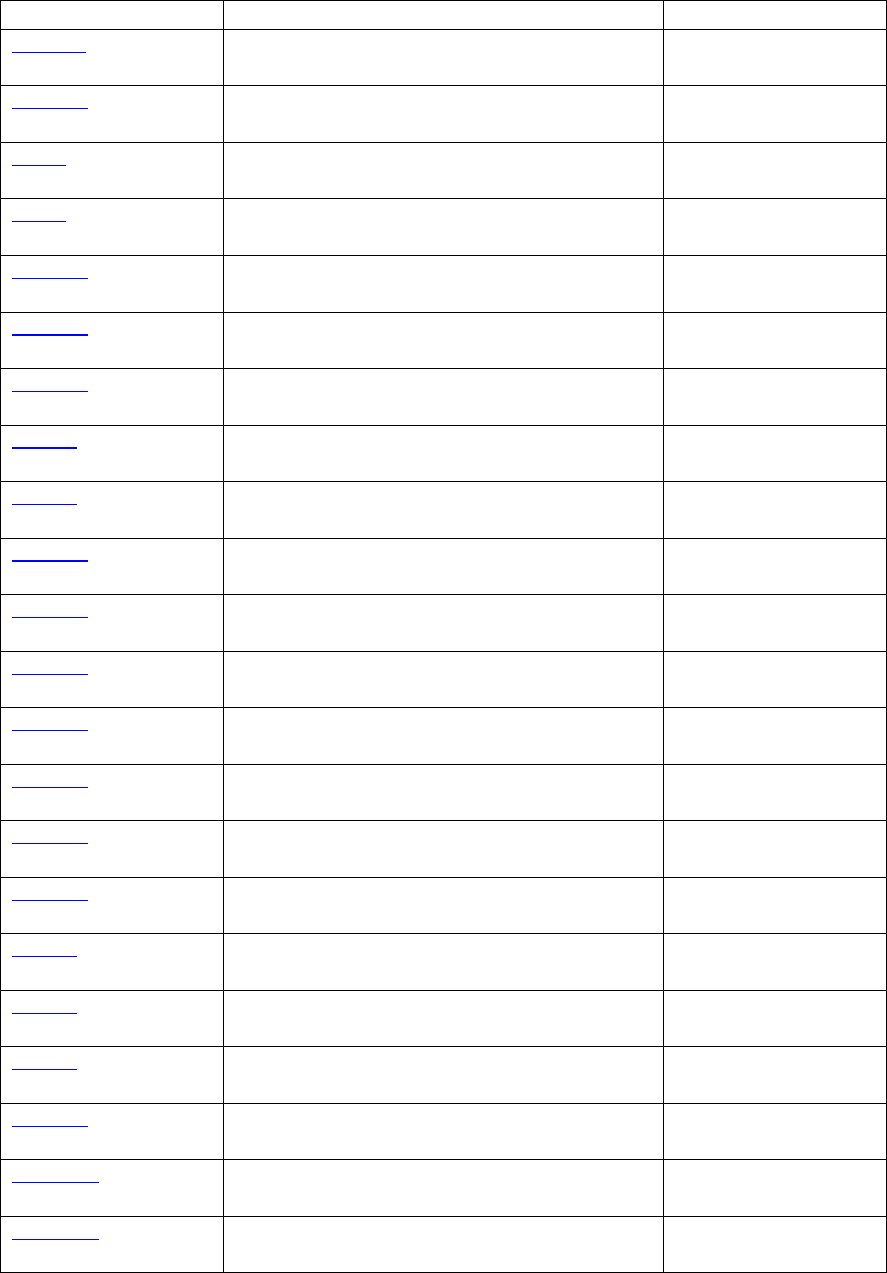
31
Bill No. & Sponsor
Bill Title
Year Passed
S.B. 132
Christensen, A.
Health Care Consumer’s Report
2005
H.B. 137
Daw, B.
Pain Medication Management and Education
2007
H.B. 6
Menlove, R.
Controlled Substance Database Amendments
2007
H.B. 9
Morley, M.
Health Care Cost and Quality Data
2007
H.B. 133
Clark, D.
Health System Reform
2008
H.B. 326
Curtis, G.
CHIP Open-Enrollment
2008
H.B. 119
Daw, B.
Controlled Substance Database Amendments
2008
H.B. 24
Menlove, R.
Amendments to Utah Digital Health Service
Commission Act
2008
H.B. 47
Menlove, R.
Standards for Electronic Exchange of Clinical
Health Information
2008
H.B. 188
Clark, D.
Health System Reform – Insurance Market
2009
H.B. 106
Daw, B.
Controlled Substance Database Amendments
2009
H.B. 331
Dunnigan, J.
Health Reform--Health Insurance Coverage in
State Contracts
2009
H.B. 128
Menlove, R.
Electronic Prescribing Act
2009
H.B. 165
Newbold, M.
Health Reform--Administrative Simplification
2009
H.B. 294
Clark, D.
Health System Reform Amendments
2010
H.B. 186
Menlove, R.
Controlled Substance Database Revisions
2010
H.B. 52
Newbold, M.
Health Reform - Uniform Electronic Standards -
Insurance Information
2010
H.B. 18
Daw, B.
Health Reform – Cost Containment
2011
H.B. 19
Dunnigan, J.
Insurance Law Related Amendments
2011
H.B. 128
Dunnigan, J.
Health Reform Amendments
2011
H.B. 0404
Ipson, D.
State Health Insurance Amendments
2011
H.B. 0046
Menlove, R.
Electronic Personal Medical Records
2012
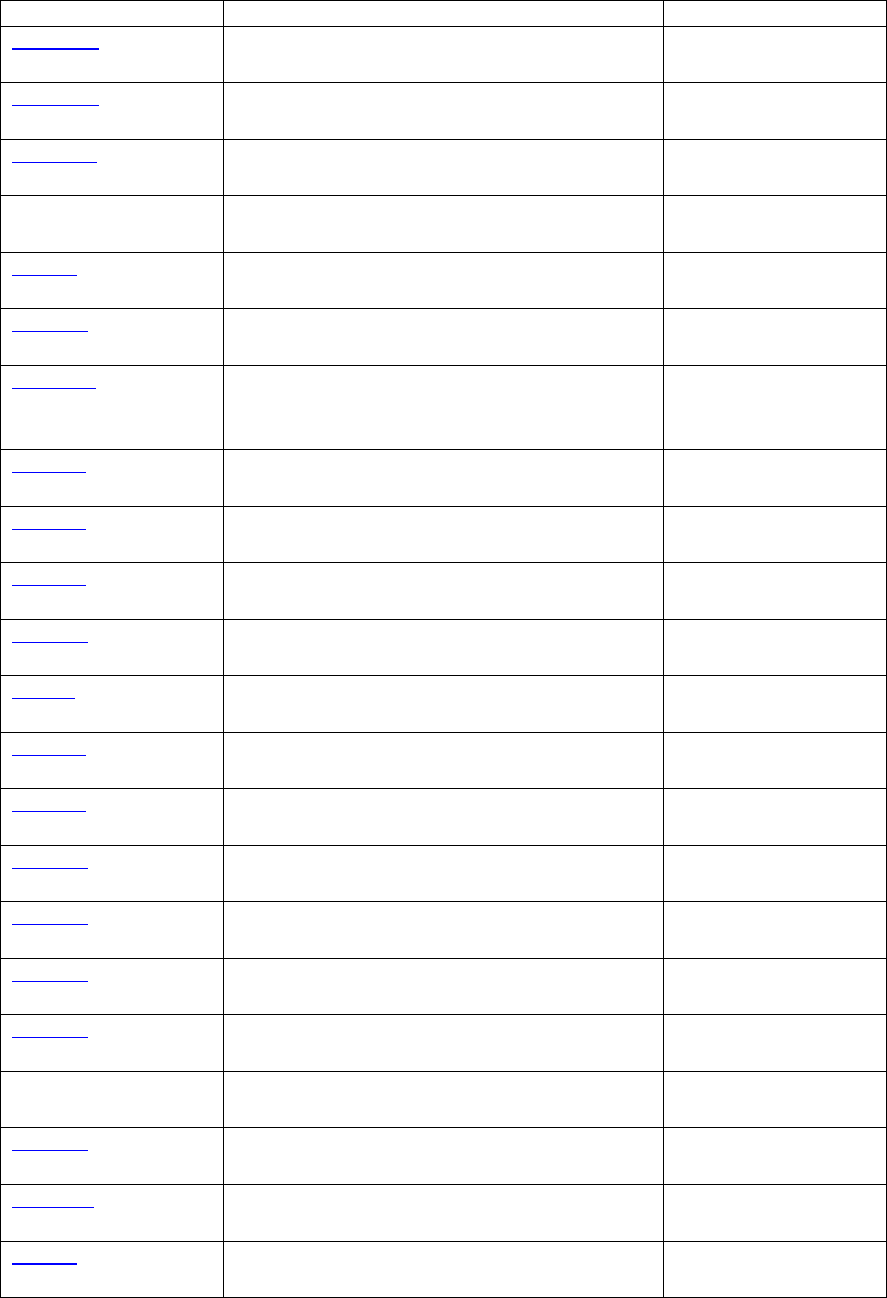
32
Bill No. & Sponsor
Bill Title
Year Passed
H.B. 0450
Dee, B.
Health Insurance Amendments
2012
H.B. 0475
Ray, P.
Medicaid Amendments
2012
S.B. 0085
Christensen, A.
Medicaid Cost Control Amendments
2012
H.B. 25
Barlow, S
Patient Identity Validation
2012
H.B. 42
Valentine, J.
Repeal of Health Insurance Mandate Review
2013
H.B. 364
McCay, D.
Nullification of Federal Health Care Law
2013
H.C.R. 10
Adams, J.
Concurrent Resolution on the Patient
Protection and Affordable Care Act and State
Health Care Reform
2013
S.B. 213
Knudson, P.
Employer Association Health Plan Amendments
2013
S.B. 242
Hillyard, L.
Health Insurance Market Amendments
2013
S.B. 142
Weiler, T.
Small Employer Health Insurance Amendment
2014
H.B. 141
Dunnigan, J.
Health Reform Amendments
2014
S.B. 71
Harper, W.
Informed Consent Amendments
2014
S.B. 251
Shiozawa, B.
Amendments to Medicaid and Health Care
2014
S.B. 272
Davis, G.
Expansion of Medicaid Program
2014
H.B. 114
Ward
Controlled Substance Reporting
2016
H.B. 239
McKell
Access to Opioid Prescription Information via
Practitioner Data Management Systems
2016
H.B. 149
Daw
Death Reporting and Investigation Information
Regarding Controlled Substances
2016
H.B. 310
Thurston
Utah Statewide Immunization Information
System Program
2017
S.B. 150
Eliason
Utah Statewide Stroke and Cardiac Registry
2018
H.B. 461
Christensen
Patient Access to Medical Records
Amendments
2018
H. B. 158
Daw
Controlled Substance Database Revisions
2018
H.B. 77
Daw
Health Information Exchange Amendments
2019
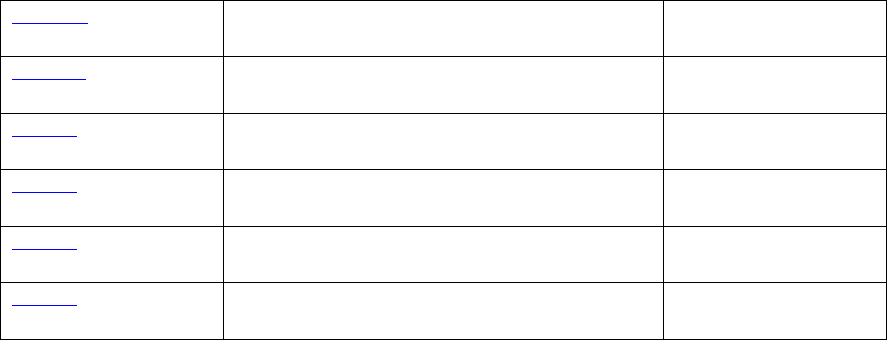
33
H.B. 313
Ballard
Telehealth Parity Amendments
2020
S.B. 138
Vickers
Pharmacy Benefit Manager Revisions
2020
H.B. 15
Ward
Controlled Substance Amendments
2021
H.B. 85
Hall
Controlled Substance Database Access
2021
H.B. 19
Elias
DNA Specimen Analysis Amendments
2022
H.B. 21
Handy
School and Child Care Center Water Testing
Requirements
2022
The Utah legislature has shown its support of HIT initiatives in Utah. We feel that our
Medicaid program and our HIT/HIE partners have received all the needed legislation to
continue and move forward with our EHR Incentive Payment Program into the future.
Additional supportive legislation is likely t o be considered in the next session.
Utah Medicaid Operations & Systems Support Landscape
Utah Medicaid is committed to educating providers, promoting the EHR incentive program
and working with UHIN and HealthInsight to meet the goal of an increase in numbers of
medical professionals using certified EHR technology.
Utah Medicaid Bureau of Medicaid Operations has a provider training program. This
program has been used to help educate providers on the Medicaid PI Program.
Additionally, Medicaid has a web site that Medicaid providers can use to find the right
entity for questions about EHR, cHIE and the Medicaid PI Program. The PI program
maintains a dedicated page of the Medicaid website. The page includes information on
registration and enrollment, auditing, eligibility, payment process, public health
reporting measures, training, and other helpful material including a provider user guide
and frequently asked questions. This site also links to the current version of the SMHP.
The Utah Medicaid PI Program is staffed by a Health Program Manager, with a Health
Program Specialist who processes the provider and hospital attestations. Oversight is
provided to this group from the Assistant Bureau Director for the Bureau of Managed
Health Care. Program staff is readily available to answer the Provider Hotline, and
interact with providers on a daily basis answering questions or addressing technical
issues with the attestation site. This Hotline number also appears on every screen that
providers/hospitals encounter when they are completing an attestation.
In 2013, the State of Utah selected a new MMIS replacement vendor. The vendor is CNSI
and the Utah MMIS replacement system is called PRISM (Provider Reimbursement
Information System for Medicaid). CNSI has customized a software solution package
outside of PRISM titled the Electronic Medicaid Incentive Payment Product (eMIPP.) The
decision to use CNSI’s eMIPP product was based on the fact that it is a pre -built, “off-
the-shelf” solution that would integrate simply with the PRISM infrastructure. We feel
confident that this solution has improved the user experience for incentive program
participants, and streamlined reporting and payments.
Currently the states of Michigan, Washington, Illinois and Maryland use eMIPP to
administer their Medicaid PI Program. Sharing this solution with other states offers an
additional benefit. The cost of programming any changes resulting from future CMS final
34
rules can be split among these states. The State of Utah completed requirements
gathering and system design for a Utah implementation of eMIPP. The State and CNSI
determined it would be best to implement the eMIPP product at the same time as the
Provider Enrollment module. Despite some development delays, eMIPP went live in July
2016. The previous Oracle solution has been retired, however, the requirements
documentation used to build it have been retained and used as a resource as needed.
Although eMIPP was implemented in July 2016, Utah continued to make PI payments to
EPs and EHs from our legacy system. At this time we anticipate that Medicaid claims and
payments will be live in the PRISM cloud based solution in January 2023. If this milestone
is achieved prior to the completion of post-payment audits, then PI payments resulting
from audit or appeals processes will be processed through these new mechanisms.
Program staff works closely with state DTS and participates in the testing process. The
DTS resources needed for maintenance, development, testing and implementation of the
eMIPP payments are in place and funding is outlined in the most recen t IAPD.
The following technical work is supported by CNSI and is considered integral for an
administration of the EHR Incentive Payment Program.
CNSI scope of work for the eMIPP product includes :
• Maintaining a two-way Interface between eMIPP and the NLR so that new
provider records and updates can be received from the NLR, and payment
requests, payment records, audits and appeals can be communicated to
the CMS NLR.
• Developing and testing user interface screens used by eMIPP providers
and state personnel.
• Maintaining and updating all meaningful use requirements to conform with
CMS regulatory changes and program updates.
Cost estimates for state technology solutions supporting the payment process may be
found in the State’s current HIT IAPD. Any work that CNSI performs is being paid for by
the MMIS replacement IAPD that Utah has in place.
All of the 2013 changes to Stage 1 Meaningful Use that were outlined in the Stage 2
legislation were implemented on schedule. The state also successfully programmed
screens and implemented the required changes for 2014, including the CEHRT Flexibility
Rule. The changes were approved by CMS at the time of implementation.
Utah’s PI program was delayed in implementing the changes outlined in the CMS Stage
3 Rule dated October 2015. The rule change was announced late in the program year
and required significant programming changes to implement. The State of Utah was
preparing to adopt a new MMIS system which included a new state level system. The
decision was made to delay implementation of the Stage 3 changes until the new MMIS
system went live July 1, 2016. The State of Utah accepted 2015 attestations from 7/1/16 -
10/31/16.
At the time of eMIPP go-live 7/1/2016, the Modified Stage 2 Meaningful Use modification s
were completed and approved by CMS for program year 2015. This incorporated all Stage
3 modifications for program years 2015-2017.
The system updates necessary to facilitate the 2017 changes mandated by the Outpatient
Prospective Payment Program rule and the Medicare Quality Payment Program rules went
live in eMIPP in March of 2018. This necessitated an extension of the tail period for 2017
attestations until 6/30/2018. The 2017 changes involved the following updates:
35
• Providers can select Stage 3 as an option when they are entering their meaningful use
details.
• The meaningful use reporting period was changed to 90 days for all providers.
• Modifications were made to some of the measure calculation time frames to
ensure that the actions included in the numerator must occur within the EHR
reporting period.
• As the definition of Meaningful EHR User has been updated by CMS, language in
the attestation release acknowledged by providers at the time of submission has
been updated to include additional statements.
The system updates necessary to facilitate the CQM alignment changes outlined in 2019
through the Physician Fee Schedule final rule were implemented September 27, 2019.
Additional minor changes for the 2021 reporting period were implemented June 29, 2020
which accommodate the possibility that the attestation may be submitted prior to the
completion of the Security and Risk Assessment. Due to updates to the broader MMIS
that were being implemented and tested at the same time, the PI program requested
and administered an extended tail period ending June 30, 2020.
Since July of 2016, providers attest through the new eMIPP system. The provider will
access the CMS National Level Registry (NLR) and register for the program . They receive
an invitation to attest in eMIPP when this record is received by the state. (Returning
providers receive notifications to enter eMIPP for attestation based on yearly deadlines
applicable to the provider’s stage of participation.) The provider proceeds to the PRISM
provider portal and logs into eMIPP where the provider will be able to apply and submit
eligibility information, attestations and complete other required forms. Proof of
purchase, adoption or upgrade along with the provider’s MU report cards will be
requested upon attestation and will be retained by the program manager as part of the
initial file created and housed in Utah Medicaid’s eMIPP module.
The state user in the EHR reviewer role has access to these attestations and will review
all supporting documentation and perform prepayment verifications. eMIPP does an
automated check of the ONC national registry of certified EHR technology to confirm the
certification number reported in attestation. The eMIPP system has established business
rules based on the meaningful use measure specifications to do automated analysis on
numerators and denominators submitted with the attestation. The system does frequ ent
sanction checks against local and national databases to identify any providers who should
not be allowed to participate or who may require additional review.
If additional information is needed to support patient volume or meaningful use , the
reviewer will request this information. The reviewer also has the functionality to reject
the provider attestation so that the provider can make corrections. Once the file is
determined to be complete and eligible the EHR reviewer recommends the provider for
payment. The approval of the payments is handled in the EHR approval role which is
currently assigned to an assistant bureau director in the DMHF.
Upon approval in eMIPP, the D16 duplicate payment check interface will check CMS for
permission to pay. This interface runs daily. If the record passes the duplicate payment
check then an interface sends all information necessary for the payment request to the
legacy MMIS system. This interface will also run on a daily basis, however checks are
only issued in the legacy MMIS once per week on Fridays. The program is mindful that
payments must be made within 45 days of notification to CMS. The program uses the
existing Special Payments functionality in the legacy system to accomplish these
payments. On Tuesday of the following week MMIS will send the status of the payment
and the warrant number back to the eMIPP system. Upon receipt of this information

36
eMIPP will process the D18 to notify CMS that payment was issued. The D18 interface
also runs daily.
Incentive payments for eligible providers who have a minimum of 29.5% (rounded to
30%) patient encounters paid by Medicaid, will then be eligible to receive an incentive
payment of $21,250 in his/her first year payment and $8,500 in subsequent years.
For pediatricians who apply and are considered eligible they would receive up to the
maximum allowable amounts of $14,167 in the first payment year and $5,667 in
subsequent years. If the pediatrician is not hospital based and can demonstrate that
they meet the minimum 30% threshold, they will qualify to receive the full incentive of
$21,250 in his/her first year payment and $8,500 in subsequent years.
Hospitals incentive payments are calculated by program staff using the prescribed
formula provided by CMS. Hospitals meeting Medicare meaningful use may be deemed
eligible for Medicaid incentive payments. Eligible hospitals will receive a t otal gross
payment over the course of four years. Their payment will consist of the $2,000,000
base plus a per discharge amount based on the Medicaid share of patients seen.
Hospitals will receive fifty percent of the payment in the first year and forty percent in
the second year, and five percent the last two years. In addition to requesting discharge
data from the 12-month period that ends in the Federal fiscal year before the hospital’s
fiscal year, hospitals will have to include in their registration their full, legal business
name, national provider identifier (NPI), business address/phone, tax payer identification
number (TIN) and CMS certification number and certified technology. All Utah hospitals
have been informed of the 2016 deadline to make th eir initial application for payment.
Appeals Process
Utah Medicaid PI Program providers may choose to appeal denials based on:
• Incentive payment amounts
• Provider eligibility determinations
• Demonstration of adopting, implementing, and upgrading, and MU eligibility for
incentives
• Adverse post-payment audits
The appeal process is initiated by the provider filing a written, signed request for appeal
with the Department's Administrative Hearings unit within 30 calendar days after the
date of the Department’s Denial Notification. These administrative hearings are governed
by the Utah Administrative Code, R410-14-5.
The request for appeal shall include: 1. A State Fair Hearing Request form 2. A copy of
the Denial Notification issued by the Department 2. A brief statement of the issue on
appeal 3. Documentation supporting the appeal request.
The hearing request and the subsequent scheduling of the hearing(s) will be tracked by
PI Program Manager and the Administrative Hearing Unit’s secretary until a
recommended decision is made. A final decision letter is prepared by an administrative
law judge who has reviewed the action, the issues, the findings of fact, the conclusions
of law and has documented the disposition, and the reasons fo r the disposition in a Final
Agency Order that is signed by the State Medicaid Director (or his/her designee.) The
Director may affirm, reverse, modify or remand the Recommended Decision for further
findings. This Final Agency Order will include details about subsequent appeal processes
to be used if the petitioner disagrees with the Final Agency Order.
37
After the Final Agency Order is signed by the Director, the original is sent to the
petitioner or his representative by certified mail with a return receipt and copies are sent
to other interested parties. Appeals related to incentive payment amounts or audit
findings that adjust or recoup payment amounts will be reported to the CMS NLR via E8
transactions which are triggered within eMIPP when appeals are started and finalized.
Payment Offset
The State of Utah does not use incentive payment money to offset any amounts that are
owed back to Medicaid, due to the differences in funding sources. Instead, program staff
check to ensure providers are not in credit balance with Medicaid. This check occurs at
the beginning of attestation processing and again before requesting permission to pay.
In the event that a provider who is eligible for an incentive payment is found to be in
credit balance, staff will work with provider administrators to ensure that the credit
balance is resolved prior to approving the payment. The great majority of providers will
receive their full payment via mail within two weeks of having their attestation approved.
Audits
Each Provider that receives an EHR Incentive payment is eligible for an audit. For each
stage of the incentive program, the program will audit a minimum of 10% of Eligible
Professionals and 10% of Eligible Hospitals who have received EHR incentive payments.
As of 2019, auditing has been outsourced to Myers & Stauffer, LC. All providers are
notified at the time of attestation of the requirement to retain the necessary
documentation for this payment and are advised that they may be required to furnish
this information to the program or its representative in the event of an audit. As of
December 31, 2021, Myers and Stauffer had audited 281 incentive payments and
identified five instances where payment was made incorrectly. As of June 30, 2016, the
OIG had audited 198 incentive payments and identified 12 instances where payment was
made incorrectly. Meaningful use Audits for dually-eligible hospitals were delegated to
CMS up through program year 2015. The state will take over the audits for dual eligible
hospitals starting with the 2016 program year. The Utah Audit Strategy was submitted
to CMS as a separate document. All audits, with or without negative findings, will be
reported to CMS via automated E-7 interface transaction triggered by audit statuses from
within the eMIPP state level registry.
Recoupment process for payments
When an overpayment or improper payment is identified due to audit findings the
following procedures will be followed.
The audit finding letter will notify the provider of the amount that needs to be repaid
and provide an address for returning a check to Utah Medicaid. Providers will have 30
days to appeal the audit findings, and 60 days to make payment or make payment
arrangements with Medicaid. This letter will be simultaneously shared with the Bureau
of Financial Services so that financial management has the date of the findings and can
ensure repayment of federal funds within 365 days. This timeline will be observed
regardless of any delays or difficulties with recovering the amount owed.
Once the check for the recouped amount is received by incentive program staff, this will
be returned to HITECH funds. The recouped amount will be returned to CMS through the
State's normal draw process and reported as an overpayment on Utah's next quarterly
CMS-64 report. The payment adjustment will also be reported to the CMS NLR via D18
transaction.
38
The repayment and reporting process will also be followed in the event of provider se lf-
reported refunds, where there is no audit finding.
Other HITECH Funding Opportunities
We are integrating the SIM recommended HIT projects as they are identified and are
consistent with the HITECH Administrative Funding opportunities. In this process,
Medicaid provider types have been identified across the continuum of care. The goal of
HITECH 90/10 IAPD applications is to reach out to these providers around specific use
cases. A current list of potential projects prioritized in the SIM process with b rief
descriptions is found in table below.
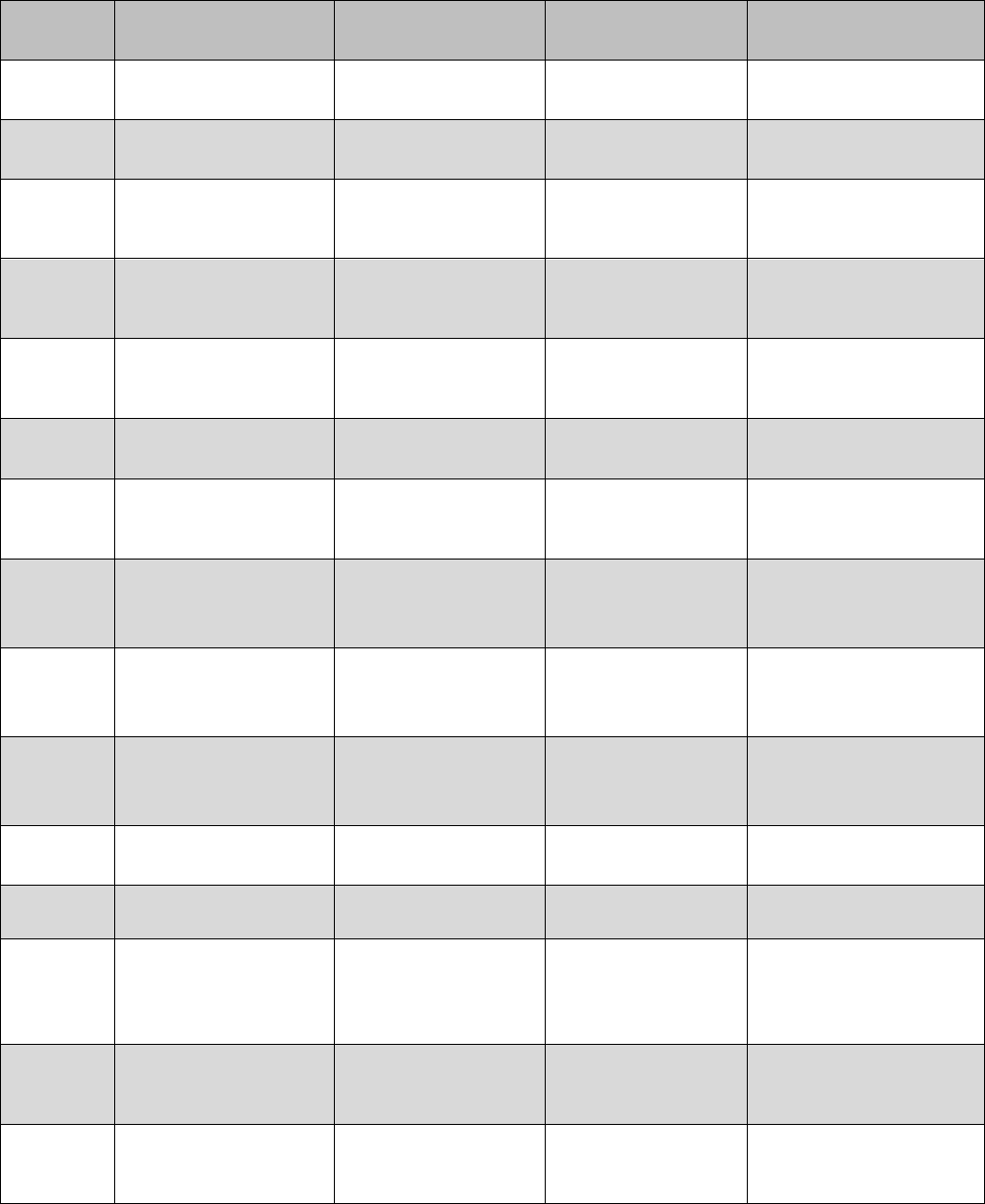
39
Project
Project Description
Medicaid Project
Description
Providers Types
Matching Source
ePOLST
Connect all SNF to
cHIE
Onboarding Medicaid
Providers
Long Term Care
Providers
SNF civil money
penalties
ePOLST
Upload ePOLST from
SNF to PH registry
Query Exchange
Long Term Care
Providers
SNF civil money
penalties
ePOLST
Connect all EMS
agencies to cHIE
Onboarding Medicaid
Providers
Emergency Medical
Provider Service
Providers
BEMS grant $$
ePOLST
Provide EMS Access to
ePOLST at POC
Query Exchange
Emergency Medical
Provider Service
Providers
BEMS grant $$
ePOLST
Provide ED
departments access
ePOLST at POC
Query Exchange
Emergency Medical
Provider Service
Providers
BEMS grant $$
CSDB
Connect CSDB to CHIE
Onboarding Medicaid
Providers
Pharmacies
CSDB general funds
CSDB
Provide Access to
CSDB at POC
Query Exchange
Emergency Medical
Provider Service
Providers
CSDB general funds
Ped BH
Summary
Connect all BH
providers to cHIE
Onboarding Medicaid
Providers
Behavioral Health
Providers
BMI/Department of
Pediatrics
Ped BH
Summary
Upload PED BH
Summary
Query Exchange
Behavioral Health
Providers
BMI/Department of
Pediatrics
Ped BH
Summary
Provide access to PED
BH Summary at POC
Query Exchange
Behavioral Health
Providers
BMI/Department of
Pediatrics
THsISU
Establish Governance
and Service Provision
Health Information
Services Provider
Community-Based
Providers
Business Case/Providers
MPI
State MPI
Provider Directories
Community-Based
Providers
General fund
Medicaid
Expansion
Expansion of Medicaid
coverage to
correctional,
homeless, MH/SUD
Onboarding Medicaid
Providers
Correction Heath
Providers
General fund
Trauma
Registry
Electronic Health
Record reporting to
Registry
Public Health System
development/connec
tion
Community-Based
Providers
BEMS funding
EMSC
Registry
Electronic Health
Record reporting to
Registry
Public Health System
development/connec
tion
Community-Based
Providers
BEMS funding
40
HITECH Funds to Promote HIE connections with Medicaid Providers
In the Medicaid Directors Letter dated February 29, 2016, CMS expanded the scope of
expenditures that are eligible for the 90 percent matching rate. In response to this
funding change, the State of Utah requested HIE funding for th ree projects which will
help the state achieve the following goals:
• Connect more providers to Utah’s HIE.
• Improve the data quality and availability of data in the HIE by facilitating
improvements in the master person index and by minimizing manual process es
in newborn screening.
• Enhance the interoperability of EHRs.
• Enhance coordination of care among providers of primary care, specialty care,
behavioral health care, various therapies, and community-based services.
• Enable the health information exchange of controlled substance medications to
EP EHR systems.
• Improve outcomes for newborns by expediting interventions for certain
conditions.
• Improve outcomes for pediatric patients with complex medical conditions .
• Enhance provider clinical decision making.
Pediatric Patient Portal
The State has identified a slow progression of HIE utilization and adoption among
providers who care for children with complex conditions, delaying its anticipated impact
on the quality, costs, and outcomes of patient care in this pop ulation. To address the
slow progression of HIE utilization, the State initially developed a Pediatric Patient
Summary (PPS), a web-based platform where clinicians and parents can collaborate to
maintain a succinct, accurate, and up-to-date compilation of relevant information about
children and youth with special health care needs (CYSHCN). The State also operates its
Medical Health Portal, which offers guidelines, information, tools and other resources for
clinicians, their teams, and caregivers to improve the care of CYSHCN, and their families,
along with directories of local service providers.
The project was approved by CMS on 8/30/2017. It will address the challenges to the
use and value of the Clinical Health Information Exchange (cHIE) to the target ed
providers by embedding the PPS into EHR systems as an app compliant with SMART and
FHIR standards. In addition, the project will redesign, develop, and implement its
organization, content, and content management, data structure, and utilities and to
integrate access to its resources into the PPS.
The pediatric patient portal will support:
• The utility and value of Utah’s Clinical Health Information Exchange (cHIE) for
behavioral health providers, and other non-traditional users of HIE, particularly
those who care for children and youth with chronic and complex conditions,
including physical, occupational, and speech/language therapists, home health,
public health, emergency medical services, substance abuse providers, and the
parents/guardians/caregivers of those children
• Coordination of care among providers of primary care, specialty care, behavioral
care, various therapies, and community-based services
• Clinical decision making, particularly in long -term management of chronic
conditions
41
• Engaging and enrolling the range of providers of care for Medicaid -enrolled
children and youth, particularly those not currently us ing HIE
• Engaging patients and/or their parents/guardians/caregivers in understanding
their conditions, in self-care, and as partners in coordinating care and improving
outcomes
This project offers unique benefits to clinicians and patient families:
• User-friendly, efficient presentation of a concise summary of essential
information from different institutions about children with chronic and complex
conditions;
• Features to support Care Team Management and collaborative Care Planning that
enables engagement of parents/guardians and sharing through HIE, Direct, and
pdf;
• Integrated access within the PPS to information from the MHP to support primary
care, care coordination, specialty collaboration, patient/family education, shared
decision-making, and access to relevant professional and community providers to
address clinical and related needs as well as social determinants of health ;
• Collaboration with UHIN, Medicaid, and other payers to enhance information
available on potential clinical providers; may be translatable to other states’ HIEs
and Provider Directories;
• App integrated into and launchable seamlessly within Epic; piloted also in Cerner,
and potential for other FHIR-compliant EHRs (will be explored for those popular
with Community Health Centers);
• MHP currently collaborating with 6 states to present local service provider
directories, some of which have already expressed interest in the PPS -MHP app
for their state; the app may enhance interest of other states in collaborating.
Several agencies were able to work together successfully to develop an app with
aggregated data from multiple sources that helps physicians treating children and youth
with special health care needs. A family app was also developed to allow families of
CYSCHN to also view the information. Some objectives were not met, such as the ability
for families to enter, store, and share comments within the app. Some of these shortfalls
came from miscommunications and understanding among the parties, such as the cHIE
not having a patient-facing portal. All parties expect to maintain and expand the use of
the PPS and Family PPS over the coming years.
Controlled Substance Medication Integration
The Controlled Substance Database (CSD) contains all dispensed controlled substance
medications for all Utah patients, and the CSD is used by the State’s Prescription Drug
Monitoring Program (PDMP) and Medicaid to analyze controlled substance usage. The
CSMI project will develop the infrastructure necessary to integrate with the CSD to
enable health information exchange between the CSD and Medicaid Eligible Providers
(EPs). This will most significantly, allow for enhanced care coordination of Medicaid
eligible patients receiving controlled substance medications, such as opioids, while also
enabling opportunities for EPs to meet medication reconciliation, health information
exchange, and clinical decision support Meaningful Use (MU) objectives and related
electronic clinical quality measures (eCQMs), as a part of the PI Program. This effort
also supports expanded onboarding of non-traditional EPs, such as Medicaid pharmacists
and prescribers. CMS approved this project on 2/20/2018
The four main areas of this project are:
42
• Develop master person linkage within the states Controlled Substance Database
(CSD) as required for HIE to link medication records to Medicaid patients within
EHR systems for care coordination, medication reconciliation and clinical decision
support.
• Develop web API layer to support HIE between the CSD and external systems to
extract and transform controlled substance medications to be consumable into
Medicaid eligible EHR systems.
• Onboard new eligible providers and EHR systems to the clinical Health
Information Exchange (cHIE) to support EPs meeting MU objectives and eCQMs.
• Develop enhanced analytics for use in clinical decision support and care
coordination
The CSMI project moved forward the state’s desire to better integrate EHRs and the
PDMP to streamline medication management and prescribing workflows. The University
of Utah’s research helped inform which CSD and EHR changes would be most effective.
Lastly, the DOPL was successful in expanding their CSD integrations with healthcare
entities around the state. The project experienced legal challenges and unforeseen
staffing issues due to COVID and turnover that prevented some objectives from being
completed. DOPL and UDOH intend to further improve the PDMP.
Newborn Screening
Newborn Screening (NBS) saves lives through the early identification and timely clinical
management of babies born with life threatening disorders. However, identification
through screening, diagnostic testing, short-term clinical management, and long-term
clinical management relies on inefficient system infrastructure that delays timely
identification of babies at risk, compromises care, and results in significant cost burdens.
This project focuses on improving NBS infrastructure to improve infants’ health
outcomes. CMS approved this project on 7/23/18.
This project will build on and expand the utility and features of the cHIE and Utah
Department of Health Master Person Index (DOHMPI) to improve the NBS process.
Features within the cHIE that will be improved and/or developed include the Patient
Lookup Service, Order Receiving Service, Patient -Provider Relationship Manager, NBS
Result Distribution Service, and Provider Repository.
This project has three main areas:
• Establish HIE for NBS related data between EHRs and the laboratory information
management system (LIMS) at the Newborn Screening Program (NSP) b y
leveraging Utah’s Clinical Health Information Exchange (CHIE).
• Develop HIE for genomic data from NSP LIMS to EHRs.
• Establish NBS long-term follow-up to enhance clinical decision making for NBS
disorders.
Electronic Physician Orders for Life Sustaining Treatment (ePOLST)
Clinical health information exchange for end-of-life care is one of the Utah Health
Information Technology Strategic goals. The ePOLST project (approved September 10,
2019) is focused on design, development, and implementation of a HIE -based application
to enhance the utility, value, and use of HIE in the care and engagement of Medicaid -
insured patients with serious illness or frailty. This application will enable long term and
post-acute care Medicaid providers, and caregivers to access and share Physician Orders
for Life Sustaining Treatment (POLST.) This project aims to share advanced directives
using SMART on FHIR interoperability standards, which will further integrate data from
provider EHRs into the cHIE.
43
The minimum project objectives were met and the ePOLST HITECH project has improved the
infrastructure in Utah for coordinating care for patients with serious illness. Workflows have been
modernized to make documentation and sharing of POLST easier for participating facilities. Utah
plans to continue training and expanding the use of ePOLST in the state now that the systems
have been updated and tested to support more streamlined workflows.
Falls Prevention
This project, approved September 10, 2019 is targeted to older adults 65 years and older
who are dual eligible beneficiaries (Medicaid/Medicare) at high risk for future falls. An
older adult who falls, calls 911 for assistance, and is not transported to the Emergency
Department is at high risk for another fall. However, the records from non-transport EMS
calls are not shared with insurance companies, healthcare providers, or care managers
at Area Agencies on Aging. This represents a missed opportunity to prevent future falls,
repeat EMS calls, and hospitalizations.
Since EMS non-transport calls are not billable, healthcare providers, insurers, and Area
Agencies on Aging are not aware when their patients/ beneficiaries have fallen, but not
suffered an injury. Agencies and healthcare providers are unable to initiate a
preventative fall risk management program.
This project will integrate Bureau of Emergency Medical Services (BEMS) assessment
data for non-transport fall calls for older adult who are 65 years and older to the Utah
Clinical Health Information Exchange (cHIE). Within cHIE, BEMS data will be matched
with electronic health record data using patient name and zip code of residence. Alerts
of the fall can then be sent to Medicare Advantage plans, healthcare providers and case
managers at Area Agencies on Aging that are currently providing care, or medical
insurance, for the individual.
The Falls project provided an automated way for Falls event data to flow from an EMS
vendor to the Department of Health to the state’s cHIE. This allows the cHIE to inform
providers of these Falls events of which they would have otherwise been unaware. UHIN
also developed a home health hub that will be a convenient way to coordinate home
health services among agencies and providers that does not require signif icant effort to
setup by each participating entity.
Utah’s “Programmatic” HIT Landscape
Utah Medicaid worked directly with our stakeholders to record the “ Historical” landscape
(formerly known as the “As Is” landscape) and develop the “Programmatic” landscape
(formerly known as the “To-Be” landscape). As identified in our first iteration of the
SMHP, we will continue to facilitate payments to eligible providers and hospitals.
Medicaid will also continue to work with our established partners on current and future
projects that bring us closer to our long-term HIT/HIE goals. These goals include:
providing credible information to consumers so they make informed health care
decisions, reviewing provider quality data, seeing all Utah clinicians meaningfully use
HIT, and connecting to our State’s HIE to report timely and accurate public health data
to improve population health. We will also seek to increase interoperability across the
continuum of care of Medicaid providers which may include but , is not limited to
onboarding, provider directories, secure electronic messaging, query exchange, care
plan exchange, encounter alerting, public health systems development , and the provision
of health information services.
44
Governance Landscape
Utah has appropriate HIT governance and partnerships in place as noted in the above
‘As-Is’ section. The State’s Digital Health Service Commission includes broad
representatives. Medicaid is a member of the UDOH Meaningful Use Workgroup including
all public health partners from Immunizations, Syndromic Surveillance and Lab Reporting
and Cancer Registry.
Provider Landscape
In the later stages of the PI program, the focus has naturally shifted from
outreach/onboarding. As described elsewhere in this document, several factors are
contributing to a narrowed base of participating providers. No new providers have started
year one of the program since program year 2016. Changing requirements and the
difficulty (and costs) to continue to meet the meaningful use measures have made this
program less accessible to smaller, independent providers and groups who may lack the
administrative and technical support that is needed. The providers who remain in
participation with the PI program are well experienced with this program. Supporting
these types of attestations consists less of training and outreach and more of technical
support.
Program staff have developed strong relationships with the provider community who
receive these payments. We are focused on keeping them informed of updates and
deadlines, and reinforcing their responsibility to submit accurate information and
maintain proper documentation for the PI incentive payments.
Legislative Landscape
As noted in the ‘As-Is’ section, the Utah Medicaid Program and our HIT/HIE partners
have received all the needed legislation to continue to move forward with our EHR
Incentive Payment Program. As Utah continues to implement the EHR Incentive Program
new legislation may be required to insure broader access to medical data for
professionals, hospitals, public health programs and entities in order to make informed
decisions that will improve the health care outcomes for the citizens of Utah.
Utah legislature has passed a bill to expand Medicaid coverage for adults and some of
the most at risk populations. The increase of Medicaid recipients may have the effect
of increasing the number of providers with sufficient Medicaid patient volumes to attest
for Meaningful Use.
Utah Medicaid Operations Landscape
In order to continually and successfully initiate payments to eligible providers and
hospitals, certain business processes and documents (i.e. attestation/registration forms)
have been developed, staff hired and provider outreach and education about the program
has occurred. The EHR Program Manager continually engages with stakeholders and
other Utah Department of Health and Department of Techn ology Services (DTS) staff to
produce deliverables and meet milestones so payments can continue to Utah eligible
providers and hospitals.
The State of Utah compiled requirements and documentation for a Request For Proposal
(RFP), with the intention of selecting a specialized audit vendor to support the Medicaid
PI Program. The scope of work includes a comprehensive update (and maintenance) o f
the Utah Promoting Interoperability Audit Strategy, execution of post -payment audits,
professional support in evaluating hospital payment calculations, and other subject
matter expertise as required. The RFP was posted to the state procurement system on
45
12/26/17 and closed to respondents on 2/9/2018. After evaluating and scoring the
various responses, the PI program awarded this contract to Myers & Stauffer, LC on
3/20/2018. CMS approved the program’s request for funding these audit activities in the
IAPD which was approved December 6, 2018.
The following table identifies the business processes that have been developed, tested,
and documented by the designated program manager, program support staff , and DTS
staff. The table has been updated to reflect ongoing updates in the CNSI MMIS for the
following business processes:
46
Promoting Interoperability Program Activities Table
Specific
Business
Process or
Requirement to
Making PI
Payments
Oracle
Solution
Status
CNSI eMIPP
Status
Expected
Outcomes
or Products
Responsible
Staff
• Lead
• Support
Interface with NLR &
CMS regarding
payments made to
eligible providers
Sunset
date
7/1/2016
Fully functional as
7/1/2016.
A developed
system that
interfaces with
the National
Level Repository
(NLR)
Lead
DTS/CNSI -
Developers
EHR Program
Manager
Support
Medicaid Staff
Verify Medicaid
patient volume for all
applicants, provide
notification of
approval/denial for
incentive payments
Sunset
date
7/1/2016
Fully functional as of
7/1/2016
Attestation Form
and NLR
interfaces will be
in EMIPP.
Lead
DTS/CNSI -
Developers
EHR Program
Manager
Support
Medicaid Staff
Process payments to
providers and
hospitals, query
claims data base to
verify that providers
meet Medicaid
patient volume
Fully
functional
as of
10/1/2011
These functions will stay
in legacy until the claims
subsystem is functional,
target date currently
March 2022 for
payments to process
from PRISM.
Payments made
in timely manner
to eligible
providers,
validation of
patient volume
Lead
DTS/CNSI -
Developers
EHR Program
Manager
Support
Medicaid Staff
Create & maintain a
Web site for Provider
Enrollment & FAQs
7/1/16
Current site is fully
operational as of
10/1/11 with continual
updates throughout the
life of the program.
The links and web
based trainings for
eMIPP are available as
of 7/1/16
Website is
running with
continuous
updates
Lead
EHR Program
manager
Support
State DTS
Continue to develop
communication
materials about the
EHR Incentive
Program and/or EHR
adoption/meaningful
use
12/1/14
Ongoing
Communication
strategy & plan
that covers the
new look and
feel of EMIPP
will begin a few
months in
advance of
switching to
EMIPP
Lead
EHR Program
Manager
Support
Medicaid staff
Conduct provider
outreach activities for
HITECH
interoperability
projects
Ongoing
Ongoing
Webinars,
meetings, and/or
presentations
conducted
Lead
EHR Program
Manager
Support
HealthInsight
47
Core Administration Activities Table
Specific Business
Process or
Requirement to
Making PI
Payments
Expected
Start Date
Continue
or End
Date
Expected
Outcomes or
Products
Responsible
Staff
• Lead
• Support
Installed a provider
help-line/dedicated e-
mail address/phone
Ongoing
Ongoing
The EHR Program staff
respond to calls,
emails &
correspondence
regarding technical
issues, program
parameters,
enrollment validation &
disputes (not appeals)
Lead
DTS -
Developers
EHR Program
Manager
Support
Medicaid Staff
Monitor & review
current CMS policies,
propose recommended
changes or inclusion of
new policies &
procedures, develop &
update FAQ’s for
dispute resolutions,
keep screens and
business processes
current
Ongoing
Ongoing
Effective business
process models
supported by
stakeholders, plus
technical system
support changes as
necessary & a
consistently updated
SMHP & IAPD
Lead
EHR Program
Manager
Support
CNSI
Validate volume
thresholds, payment
calculations, meaningful
use, quality measures &
provider credentials
throughout the life cycle
of the program.
3/1/15
Ongoing
Queries to calculate
Medicaid patient volume
are now run directly from
the data warehouse.
Reviewer initiates this
process manually.
Lead
DTS/CNSI -
Developers
EHR Program
Manager
Support
Medicaid Staff
Review of administrative
activities & expenses of
Medicaid provider health
information technology
adoption & operations;
financial oversight &
monitoring of
expenditures including
provider enrollment
procedures for
combating fraud waste
& abuse in the program
Ongoing
June 2016
Compliance with the
following:
42 CFR § 495.364
42 CFR § 495.366
42 CFR § 495.368,
§455.15, §455.21
Lead
EHR Program
Manager
Support
Utah’s Office of
Inspector
General,
Medicaid Staff &
HealthInsight
Staff
Collaboration with Public
Health Partners and
cross continuum
interoperability
Ongoing
Ongoing
Public health reporting
for syndromic
surveillance, lab
reporting and
Immunizations
Lead
EHR Program
Manager
Support
Public Health
Partners
Maintenance of State
Audit Plan, execution of
post-payment audits for
PI incentive payments
by professional audit
staff
4/1/19
9/30/23
Compliance with the
following:
42 CFR § 495.364
42 CFR § 495.366
42 CFR § 495.368,
§455.15, §455.21
Lead
Myers & Stauffer
LC
Support
EHR program
staff
48
Administration and Oversight
Sanctions & Licensing Verification
Once a provider has enrolled at the CMS web site the registration s are sent to the state
by the next business day. Federal sanction verifications are completed on a registration
before being sent to the State.
In response to the B6 provider registration records received from CMS each day, eMIPP
performs automated validation checks (provider type, sanctions, death match,
provider/payee relationship, Medicaid enrollment) and notifies the provider via email to
complete their attestation.
For eligible providers, eMIPP will transmit a D16 ”intend to pay” transaction to CMS daily.
Once eMIPP receives the daily response from CMS, the requested payment amount is
validated, and a second sanctions check is performed.
To ensure that payments are not made to payees who are in credit balance status, review
staff query a system report from finance that checks for any balances owed to Medicaid.
The report is generated on a weekly basis. Confirmation of no credit balance is made at
the start of prepayment review and on the day of attestation approval. This verification
is stored in the eMIPP review comments. If a provider is found to be in credit balance,
staff advises on how to investigate and correct the situation and does not recommend
for payment until the balance is cleared. Medicaid does not offset or deduct the PI
incentive payment in any way due to concerns about different funding sources. The
entire payment is issued to the payee NPI that the provider has listed at the CMS national
level registration.
The PRISM Provider Credentialing Service (PCS) is an automated process that looks for
sanctions or other issues in the Medicaid provider profile. This automated check runs at
the time of PRISM enrollment and usually on a monthly basis thereafter. The eMIPP
reviewer triggers PCS manually when reviewing the attestation as an additional sanction
check. PCS performs the following verifications:
• National Provider Identifier (NPI) and related taxonomies through the National
Plan and Provider Enumeration System (NPPES);
• Drug Enforcement Agency number (DEA) numbers are assigned by the DEA to
providers who write prescriptions;
• Clinical Laboratory Improvement Amendments (CLIA) certification
numbers managed by the Centers for Medicare & Medicaid Services (CMS);
• In State and Out of State Professional Licenses;
• Social Security Number (SSN) assigned by the Social Security Administration;
• Federal Employer Identification Number (FEIN) assigned by the Unites
States Internal Revenue Service;
• State and Federal Vital Statistics; specifically date of death;
• American Board of Medical Specialties (ABMS) Board Certifications;
• Sanctions (OIG, CMSMED, SAM, MCSIS, Other State Sanctions);
• Other sanctions includes SAM and MED.
Utah confirms an active license during the attestation review process and uploads the
results to the eMIPP file. The reviewer also ensures that any disciplinary actions noted
on the license are reflected the in the PRISM provider enrollment file.
In addition to these verifications, eMIPP reviewers verify pediatrician training, when
appropriate, for pediatricians qualifying with a patient volume percentage below 30%,
but greater than or equal to 20%. If possible, pediatric board certification is verified
49
using the American Board of Pediatrics. Pediatric residency training is sometimes
confirmed using a physician faculty biography. Pediatricians may also qualify if the
Medicaid enrolled provider serves a patient base that consists of 80 percent or greater
of patients under the age of 18 (age of the patient at the time the service is rendered .)
An additional manual check is performed by sending provider name and NPI to Utah’s
Office of the Inspector General prior to payment. This prevents the program paying a
provider with a fraud investigation not otherwise visible in the PRISM system.
Hospital-Based Determination
During Utah’s pre-payment audit, a query of patient encounters determines if the Eligible
Professional (EP) is considered as hospital-based. If 90% or more of patient encounters
for the reporting period were performed in POS 21 and 23, then the provider is
determined to be hospital-based and is not eligible to receive an incentive payment.
EPs are also required to answer an eligibility question, “Hospital -Based provider? (Y/N)”.
The eMIPP system advises providers at the time of attestation that “Hospital based
eligible professionals must provide less than 90% of their services as inpatient hospital
discharging physician or emergency room physician to be eligible for the incentive
program. Hospital based is refined to exclude from the definition those EPs who are not
furnishing professional services “through the use of the facilities and equipment,
including qualified electronic health records, of the hospital.”
Provider Attestation Overall Content Verification
Provider attestation content prepayment review is performed by incentive program staff.
Reviewers follow a checklist developed for their process which consists of both manual
and automated validations. Providers with incorrect or missing information are re jected
with reviewer’s comments noted.
Eligibility Tab:
• Validate 90-day date range
• Did the provider include organizational encounters?
• Does the provider practice in an FQHC or RHC?
• Note the Medicaid encounters and total encounters
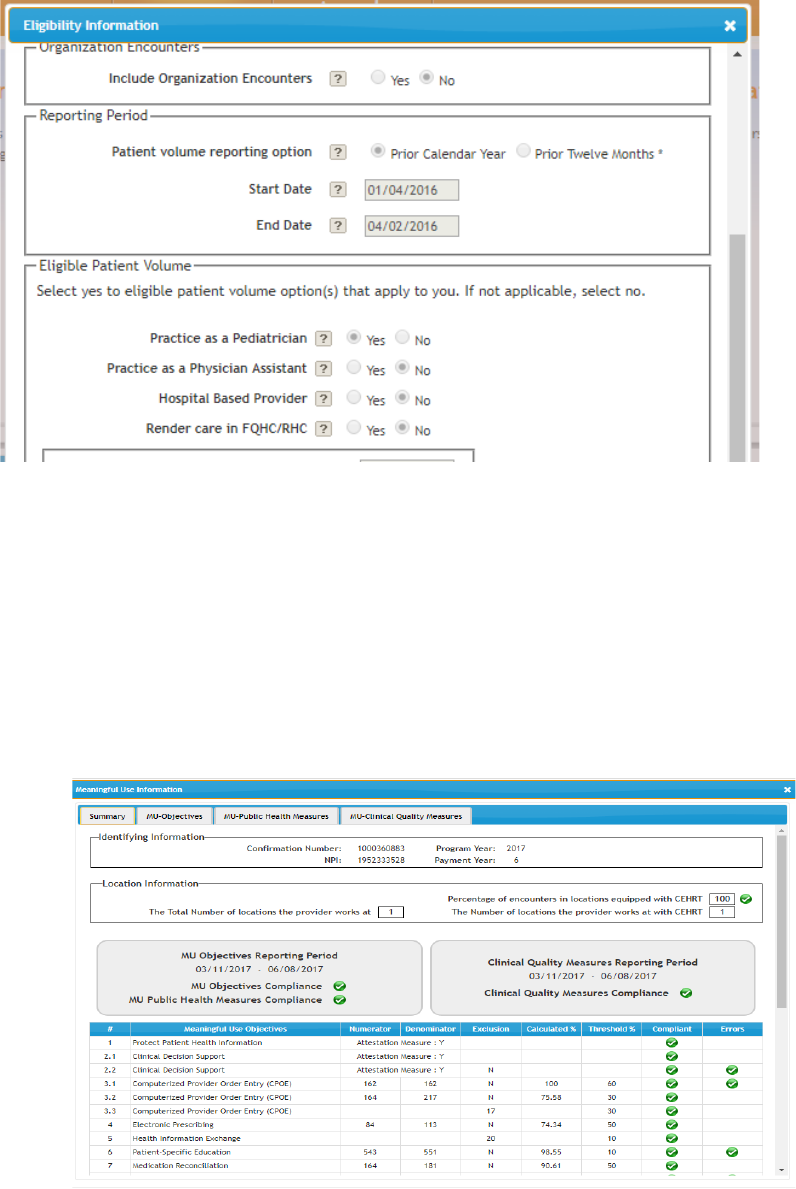
50
Meaningful Use Tab:
• Verify CEHRT questions in the location information section (compliance
recognized by a green checkmark, a red checkmark designates non -
compliance).
• Verify completion of MU Objectives Compliance, MU Public Health
Measures Compliance and Clinical Quality Measures Compliance
(compliance with meaningful use business rules recognized by a green
checkmark, a red checkmark designates non -compliance).
• Compare all meaningful use measures and exclusions entered match
provider’s meaningful use reports from certified EHR technology.
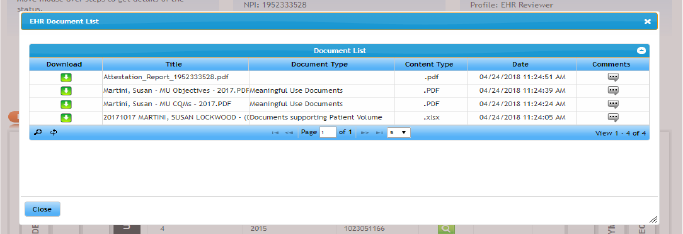
51
Upload Documents tab:
Providers may upload any documents they feel necessary for their attestation. State staff upload
other supporting documentation collected or generated during the review process.
Review tab:
Verify that patient volume is at least 20-29% for pediatricians or 30% for all other providers.
Verifying encounter data:
• Run query on NPI for selected 90-day range through data warehouse.
• Compare individual or group totals as necessary.
• Obtain additional documentation if not within 5% of attested Medicaid encounter
numerator.
• If the provider number is lower than DMHF’s number, they need to make sure that they
are counting every time that Medicaid is a valid insurance on a patient’s account. It doesn’t
matter if Medicaid is primary, secondary, tertiary or even if Medicaid paid $0.00.
• If Medicaid encounters from other states are needed to reach the eligibility threshold,
email a request to PI program counterpart in that state for a count of encounters.
• For providers who use global billing, or nurse practitioners who bill under a supervising
physician, the Medicaid claims are not always a good match for the provider’s attested
Medicaid numerator. In these cases a partial audit of patient eligibility is performed to
confirm that the Medicaid patient was eligible for Medicaid on the date of service.
Establishing Patient Volume Methodology
Methodology for Determining EP Patient Volume
All EPs (except EPs predominantly practicing in an FQHC/RHC) will calculate patient volume based
on encounters with patients eligible for Utah Medicaid or other state’s Medicaid program. The final
rule allows for an EP practicing predominantly in a FQHC or RHC to also include their CHIP patients
under the needy individual patient volume requirements.
Definition of an EP Medicaid Encounter
For purposes of calculating EP patient volume, a Medicaid encounter is defined as services
rendered on any one day to an individual where the individual was enrolled in a Medicaid program
(or a Medicaid demonstration project approved under section 1115 of the Act) at the time the
service was provided. It also includes Medicaid Managed Care Organization encounters and
encounters where Medicaid is the secondary payer.
52
Definition of an EP Needy Individual Encounter
For purposes of calculating patient volume for an EP practicing predominantly in a FQHC/RHC, a
needy individual encounter is defined as services rendered on any one day to an individual where
medical services were:
• Billed to Utah Medicaid;
• Furnished by the provider as uncompensated care (charity care); or
• Furnished at either no cost or reduced cost based on a sliding fee scale determined
by the individual’s ability to pay.
Calculating Eligible Professional Patient Volume
To calculate patient volume, providers must include a ratio where the numerator is the
total number of Medicaid patient encounters (or needy individuals for FQHCs and RHCs)
treated in any 90-day period in the previous year or the twelve months prior to the
attestation date, and the denominator is all patient encounters over the same peri od.
The numerator must consist of all patient encounters for Medicaid eligible patients during
the 90-day period; the denominator must consist of all patient encounters during the 90 -
day period.
To calculate Medicaid patient volume, EPs (except those p racticing predominantly in a
FQHC/RHC) must divide:
• The total Utah Medicaid patient encounters or out -of-state Medicaid
patient encounters in any representative, continuous 90-day period in the
calendar year prior to Program Year, or in the twelve months prior to the
attestation date; by
• The total patient encounters in the same 90-day period.
Data Sources for Patient Volume Verification
Utah runs SQL queries in the Medicaid data warehouse to verify patient volume. Medicaid
encounter counts s are compared to the Medicaid encounters attested to by the provider.
Since not all patient encounters generate a claim in the data warehouse, program staff
also sometimes will rely on verification of a portion of Medicaid patient eligibility on the
date of the reported encounter. This requires the provider to submit a roster of Medicaid
encounters from the patient volume reporting period. This patient roster is used for an
additional SQL query to confirm member eligibility for each month of the patient volume
reporting period. There are a number of Medicaid beneficiaries that cross state lines
into Utah for services, especially for specialty care with the University of Utah. The SMA
reaches out to other states’ HITECH staff to confirm member eligibility when approp riate.
The vast majority of these out-of-state beneficiaries are from states with a connection
to the cHIE.
FQHC/RHC Practice Predominantly Verification
The Utah Medicaid PI Program defines “practice predominantly in an FQHC/RHC” as
having 50 percent or more of the total patient volume for the EP over a six -month period
take place at a FQHC/RHC location. Program staff may request confirmation from the
FQHC clinic to establish the provider’s hire date with the FQHC and to establish that the
FQHC is the only practice site. The EP must also have a minimum 30 percent patient
volume attributable to serving needy individuals.
53
To support needy patient encounter totals, EPs at FQHCs are required to provide their
Uniform Data System (UDS) report, which is reported to the Health Resources and
Service Administration (HRSA). The encounters shown on the UDS report assist the
reviewer in their determination. RHC numbers are more difficult to verify. The usual
method of comparing encounters by NPI or TIN groupings and location of service is
generally utilized for the pre-payment verifications.
AIU Verification
Providers confirm adoption, implementation or upgrade (AIU) of certified EHR technology
in their first year by attesting to meeting the requirements for AIU. If the provider is
selected for post-payment audit, additional documentation will be required. Exa mples of
acceptable documentation include the following:
• Adoption: EHR contract, software license, receipt or proof of acquisition,
purchase order
• Implementation: EHR contract, software license, cost or contract evidence
• Upgrade: EHR contract, software license, receipt or proof of acquisition,
purchase order
MU Verification
The State will verify Meaningful Use through a number of automated system validations.
Business rules in the eMIPP product perform comparisons to look for possible data issues
such as measure that should have the same denominator, or denominators that should
be smaller subsets of other numbers. Review staff will compare the MU data submitted
to the reports generated by the certified EHR. Any data entry errors will be resolved
prior to payment. Documentation regarding engagement status with public health
registries will be confirmed directly with the state registries, or providers will be required
to submit documentation from external registries. The security risk assessment will be
collected prior to payment. Additional verification will also occur in post -payment audits.
These auditing procedures are not public, but will be submitted in a separate attachment
to this document.
State Specific Changes to MU
Utah requested an extension of the 2015 program year. The 2015 Modified Stage 2
regulations required a large number of changes to the SLR. At the time these were
announced the program was still operating out of our legacy solution. As the MMIS
replacement product and upgraded SLR (eMIPP) were scheduled to go live in July 2016,
the state could not justify the programming time and expense to update the legacy
system in time for the standard tail period. We applied for permission to extend the tail
period to September 30, 2016 and t his was granted by CMS staff on 3/22/2016.
An extended tail period was also requested for the 2017 program year. Due to the timing
of system upgrades, we were unable to accept the newest version of the meaningful use
measures until 4/7/2018. On February 28, 2018, CMS granted approval to extend our
tail period to 6/30/2018 to accommodate these upgrades.
The tail period for the 2019 program year was extended, with CMS permission, to
6/30/2020. This allowed us to work around some MMIS updates that made it impossible
for providers to update their Medicaid provider records for several weeks.
Due to the shortened MU reporting period for program year 2020, the attestation tail
period opened up on July 1, 2020. Providers had until 3/31/2021 to attest for 2020.
54
Eligible providers were invited to attest for program year 2021 as soon as their 2020
payment had been processed and 2021 attestations were accepted until 9/30/2021.
Utah will continue to consult with CMS regarding tail periods if additional modifications
are required.
Other than requesting these attestation deadline extensions, Utah has not implemented
any changes to the definition of Meaningful Use as it has been defined in federal
legislation.
Certified EHR Technology Verification
Entry of the EHR Certification number is required during attestation. The number is
verified via WSDL transactions (web calls) to the federal Office of the National
Coordinator (ONC) Certified HIT Product List (CHPL) web site. eMIPP automatically
verifies the program year of the certification as appropriate for the attestation. In some
instances reviewers request additional information regarding system name and version
so that the EHR certification number can be further validated. Post-payment audits may
include additional verification of the provider’s Certified Electronic Health Record
Technology. Please see the state’s Audit Plan for additional detail.
Collection of MU Data
Utah EPs and Medicaid-only EHs may submit their meaningful use data via eMIPP in three
ways: manually enter the data, complete a PDF form to be uploaded to eMIPP, or
electronically upload a QRDA file (which was extracted from the provider’s EHR system).
Information from dually eligible hospitals is received via a C5 transaction from CMS.
Utah made the decision not to require the QRDA submission. As QRDA becomes more
familiar to Utah providers, we had hoped that this method would become the more
prevalent method of providing meaningful use data. However, at this time a very small
group of providers have chosen this option and it is not likely that this will become a
significant data source for the Utah program.
Attestation Goals
As of the end of the 2016 program year, no new providers can begin participation in the
PI program. The pool of providers who can continue participation must have already
received at least one payment from Utah or from another state Medicaid agency. As the
pool of participants will no longer be growing, the program focus will shift away from
participation outreach and redirect to Stage 3 meaningful use education . Program staff
will continue to do education and outreach to returning participants to maximize
continued participation in the program.
Program participation for program years 2019-2021 is expected to trend slightly smaller
each year. This is due in part to the previously mentioned barriers to new participants,
but also the barriers posed by the more demanding Stage 3 measures. UDOH has
observed that as meaningful use stages have advanced, fewer sma ll group practices and
solo providers are able to continue participation. The bulk of participants come from
larger established practices who have extensive administrative support to assist with
monitoring progress toward meaningful use thresholds and to f acilitate attestation and
documentation.
55
The smaller pool of attestations going forward will allow UDOH to review attestations in
a timelier fashion. Providers will benefit from reduced waits for their incentive payments.
Reduced processing times also allow for the state to stay on schedule with program year
tail periods. As the eMIPP system does not allow for providers to have more than one
program year open at one time, so a provider cannot attest for program year 2019 until
the 2018 attestation has been paid or denied. Our goal will be to review and make all
payments for a particular program year before the tail period for the next program year
is scheduled to open. This will help the program stay on schedule as the 12/31/2021 end
date for PI program payments grows closer. This goal was met.
Final Environmental Scan
In 2021 Utah contracted with Myers and Stauffer LC to conduct Utah’s final
Environmental Scan (eScan). The eScan report uses various data sources, state surveys
and national surveys to capture the current Health IT and HIE landscape in Utah. This
report illustrates the State’s progress from inception of the PI program to present an
overall impact of HITECH on health IT adoption and utilization.
Since initiating the PI program in 2011 Utah has made great strides developing interoperability
and health data exchange. Some highlights of Utah’s progress in health IT include:
• From 2012 to 2016 immunization records processed through the Utah Statewide
Immunization Information System (USIIS) via EHR interfaces increased 429 percent.
• Over the years, EHR adoption has increased amongst all hospitals in Utah.
• cHIE covers 95 percent of hospitals and 90 percent of large clinics in Utah.
• Telehealth network and other community-based initiatives are actively addressing issues
such as health equity. In March of 2021, Utah Governor Spencer Cox signed a bill into
law that expands coverage of telehealth services to include mental health services.
To develop the 2021 Utah eScan, stakeholders were engaged to gain an understanding
of their goals, vision, challenges, and opportunities within the health IT and HIE
ecosystem. The primary method of data collection for this eScan was through the
distribution of a community survey. Supplementing the survey, the pr oject team
conducted key informant interviews with select representatives from state agencies and
community organizations.
A total of 392 survey respondents participated in the eScan (78% Urban and 22% Rural;
92% Medicaid providers, 6% non-Medicaid providers and 2% unsure). The survey
covered topics including EHR and Health IT Adoption, HIE and Interoperability, Patient
Portals, Broadband and Telehealth, Public Health Registries, Soc ial Determinants of
Health (SDOH) and COVID-19.
81% of respondents indicated using or implementing an EHR in 2021 compared to 59%
in 2010. 49% of respondents are entirely paperless and 43% primarily use EHR while
still maintaining some paper charts. 10% of respondents are currently participating in
the PI program. Stakeholders expressed that EHR vendors charging providers separate
fees to use additional features on an EHR has been a major barrier and impedes the use
of its maximum capabilities.
10% of respondents indicated currently participating in the PI program. The Utah PI
Program gave providers an opportunity to adopt technology and Utah saw a good mix of
participation from both large and small healthcare organizations. Many stakeholders
56
suggested that the PI Program helped booster relationships between state agencies,
community organizations, providers and patients.
Regarding Health Information Exchange in Utah, 48% of respondents still use phone/fax or mail
as their primary method of sending patient related data for care coordination. 47% of respondents
selected a lack of connectivity between EHRs as their main obstacle in exchanging clinical
information electronically with other health care providers. Stakeholders said UHIN’s cHIE is not
a robust, high volume area to exchange information. Multiple stakeholders mentioned technical
design, difficult user interface and cost associated EHR Integration as their main barriers to using
cHIE. 46% of respondents were not aware of the state HIE – UHIN cHIE. There is a significant
gap in interoperability between HIE and EHR systems in Utah.
One major change to the health IT landscape in Utah is access to and use of Patient Portals. Ten
years ago, logging into a patient portal was not common but today patients get to play more active
roles in their health care with the level of transparency patient portals can provide. 61% of
respondents offer online patient portals. 43% of respondents noted that their EHR does not offer
a patient portal. Respondents suggested that the top two functions patients use an online portal
for are appointment requests and to review their medical record.
Stakeholders mentioned that the increased use of technology has helped give public health some
leverage it didn’t have before. 32% of respondents submit information to disease registries
through EHR and 22% of respondents submit immunization to the USIIS registry through an EHR.
The pandemic helped shift provider perspective on the use of registries and need for live data. It
has led to the increased use of public health data to create dashboards, measure progress and
track metrics. 65% of respondents use telehealth to provide patient care and 87% plan to continue
offering telehealth services post-pandemic.
While the overall perception among community stakeholders is that Utah’s PI grogram has been
successful, ongoing improvements to the Health IT Landscape in Utah are possible. Unfortunately,
barriers still exist, primarily the initial provider cost of EHR implementation followed by recurring
costs of an EHR system. Other respondents noted “pharmacies all have different software vendors
that don’t integrate with healthcare provider EHRs. We waste a lot of time calling physician’s
offices to ask for clarifications. Having access to EHR would help pharmacists’ clinical judgment.”
Increased connection to UHIN cHIE is another major opportunity for improvement in Utah. 45.5%
of respondents were not aware of UHIN cHIE and 24.6% were aware but not interested in
connecting. Only 18.8% of respondents were fully connected to UHIN cHIE. Respondents who
were unaware of UHIN cHIE were asked to identify the top three out of 10 obstacles related to
exchanging clinical health data electronically (not through fax). The top three barriers were: lack
of connectivity between their EHR and other system, costs related to EHR integration, and
insufficient resources within the organization. For those respondents who were aware of or
connected to UHIN cHIE, they were asked to select the top three barriers related to connecting to
the HIE, specifically to exchange health data electronically with other organizations. The top
barriers included no direct HIE integration, insufficient resources, and organizations I share
patients with don’t use the HIE.
Many community-level stakeholders stated that Utah is behind in HIE adoption and utilization.
UHIN offers multiple product solutions to providers. Though cHIE is the state-designated HIE,
UHIN solutions are primarily used for eligibility, claims, and billing. Providers across the state have
exhibited openness and readiness to adopt the HIE if it demonstrates improved functionality (i.e.,
reliable alerts) and integrations with statewide systems and national systems (i.e., EHR vendors).
In some cases, providers are simply not using UHIN cHIE because their perception that it is lacking
57
provider/facility connection that would benefit them. Stakeholders expressed there is a general
frustration among providers due to UHINs lack of responsiveness or willingness to colloborate.
UHIN should conduct stakeholder outreach to understand and address these concerns.
At the conclusion of the 2021 survey, providers were given the option to submit an open response
stating how the COVID-19 pandemic and PHE has impacted their outlook on health IT and needs
for infrastructure and data sharing. The majority of open responses received touched on telehealth
and the increasing need to be able to access data remotely. Some noted that telehealth is cost
prohibitive for smaller rural facilities and how the pandemic has emphasized the need for improved
infrastructure. Many highlighted the benefits of virtual medicine: increasing access to care,
reduction of viral transmission, and reduced burden on existing workforce. Additionally,
stakeholders noted that while the pandemic encouraged creative approaches and innovation,
people have started thinking about leveraging technology in new ways outside of provider-patient
scenarios, like case management, driving under the influence education, and group therapy
sessions.
The full eScan is linked in the Attachments and Reference section at the end of this SMHP.
The Close of the Program and Future Pursuits
As discussed above, Utah has made great strides in the efforts to help p roviders across
the state take on electronic health records and continually improve the functionality of
these tools. Utah has also grown in the ability of our own systems to efficiently facilitate
the state’s HIT efforts. Going forward, we will continue to drive these efforts.
The findings of the Final Environmental Scan will be made available to stakeholders
including the HIE, UHIN. The SMA will encourage UHIN to make improvements to the
functionality and usefulness of the cHIE as well as general re sponsiveness and increased
provider outreach.
In 2023, the MMIS replacement project will go live. At that time, Utah Medicaid providers
will no longer be able to submit paper claims. As providers will be forced to submit
electronic claims, use of EHR or other electronic systems is encouraged by the SMA for
ease of claims submission as is registration and participation in the cHIE. The SMA
estimates 100% of Utah Medicaid providers will participate in the cHIE over the next five
years.
The Consumer Engagement Portal (Utah Medicaid’s Member Portal) will also go live in
2023. The Consumer Engagement Portal will be a secure portal much like the secure
patient portal options available through member’s providers’ EHR systems. Eligible
members over the age of 18 will be able to view and update member demographics, view
benefit, cost share and other insurance details. They will be able to track letters and
the status of inquiries, waiver applications and to file and track the status of complaints
and administrative hearings. The Consumer Engagement portal will allow them to track
health goals, fill out a Health Risk Assessment and track their favorite Medicaid providers.
Members will be able to securely email their providers’ information about themselves
from the portal. For member convenience, there will also be an app available for Android
and iOS mobile devices.
Utah Medicaid members will greatly benefit from increased access to their electronic
health information. The ability to track inquiries, applications, complaints and hearings
will furthers the long term goals of the Promoting Interoperability program by increasing
58
efficiency and giving members increased control and participation in their health records
and decision making. Better access to resources and data is a primary goal of the MITA
transition plan and we are pleased to offer these services to our members.
Utah Medicaid continues to analyze needs and opportunities for new initiatives in health
information exchange that will improve connectivity and coordination of care for Medicaid
patients and for Utahns in general.
Decommissioning the SLR and Other Closeout Activities
As the program sunsets, the SMA will work with CNSI to decommission the SLR and
retain program data for at least three years after the final annual report is submitted to
CMS. This process will take place following the completion of program activities related
to audits and appeals in FFY 2023. A HITECH Closeout Workgroup has been created to
track and complete closeout activities, including the decommission of the SLR.
While the program may be ending, policies and procedures are in place to continue much
of the tasks associated with this program. For instance, the SMA will still be able to
confirm if a provider is not sanctioned or is properly licensed and is monitored regularly
by SMA Provider Enrollment team. Should the state need to confirm if an eligible provider
is hospital based over the next five years, the state will use the same procedur es
documented in the Hospital-Based Determination section of the Administration and
Oversight section of this document. Claims and eligibility tools and queries created to
help verify patient volume will still be available to SMA staff over the next five y ears
should the SMA need to confirm minimum Medicaid patient volume thresholds for a
provider.
The SMA will be available for participant questions and concerns via email and the
program hotline for one full year after the completion of post -payment audits. Providers
who did not participate in the 2021 program year have been apprised that they are n o
longer eligible for additional payments via an automated email sent from eMIPP.
Historical program data, including the final SMHP will be available to providers and the
public on the Medicaid HIT website through June 2025.
The SMA will continue to closely monitor staff time and other activities related to HITECH
and use the appropriate funding strings to bill hours worked on HITECH activities as
opposed to MMIS or other activities. The MMIS replacement project continues and the
next phase is expected to be operational January 2023.
Interoperability and Patient Access Rule Implementation
The CMS Interoperability and Patient Access Final Rule was released March 9, 2020. The
final rule requires certain payers including Medicaid Fee-For-Service programs, Medicaid
managed care plans, and CHIP managed care entities, to provide patients with access to
their claims data, similar to the Blue Button 2.0 program, and requires a number of
actions by providers to improve interoperability. Utah Medicaid is currently in the
development and testing phase of implementing this required functionality.
Payer Responsibilities and Deadlines
• Patient Access API - Claims, Encounters, & Clinical Data: Make member
health information available to them through APIs connecting third party software
apps beginning July 1, 2021 go live October 2022
59
• Provider Directory API: Maintain and publish provider directory data through APIs
with latest updates beginning July 1, 2021 go live May 2022
• Payer to Payer Data Exchange: Exchange data set (of up to five years) to another
plan that currently covers the enrollee beginning January 1, 2023
• Increased Frequency of Federal-State Data Exchanges for Dually Eligible Clients:
From weekly or monthly, to daily exchange starting April 1, 2023
Additional projects that may be pursued in the future are listed below:
Death Certification
The Utah Department of Health recognizes the importance of timely and accurate death
reporting. When an individual dies, certification of the cause of death by a physician is
required before a death certificate can be registered with the state. Physician death
certification currently requires doctors to either complete a paper death certificate or
log in to a state’s web-based death registration system to complete the process. If this
project is pursued, the goal would be to improve the timeliness and quality of physician
death certification through a standards-based approach for physicians to certify deaths
from within their electronic health record (EHR) systems. By removing the need to log
in to a third-party application, this project will reduce the reporting burden on providers
and improve the timeliness of reports. It will also provide physicians with access to
relevant health history when entering cause of dea th information, resulting in higher
quality cause of death information.
Goals that this project would support:
• Decrease CMS spending by improving the timeliness and accuracy of death
reporting
• Identify at-risk populations for opioid deaths
• Improve the identification of leading causes of preventable death through higher
quality physician-provided cause of death information
• Reduce physician burden of reporting cause of death information and promote
meaningful use of Certified Electronic Health Record Tech nology (CEHRT).
• Improve the ability of hospitals to document patient mortality and report more
accurate eCQM measures.
Social Determinants of Health
Many factors affect the health of a person and a community. Access to quality healthcare,
educational access, economic stability, conditions in specific neighborhoods, and social and family
connections all play a role in a person’s overall health. This Social Determinant of Health (SDOH)
data is a valuable piece in understanding a person’s health risks and outcomes. Stakeholders in
Utah recognize the importance of this SDOH data and there is growing interest in the creation of
an API solution to capture this data and connect it with core clinical data in the United States Core
Data for Interoperability. Pairing this SDOH data with clinical data gives providers a robust set of
information for decision making.
Goals that this project would support:
• Improve individual and population health;
• Improve health equity;
• Improve public health services.
60
Other Strategic Health IT Goals
Through an iterative development process, the executive work group which is part of the State of
Utah Health IT Task Force has developed proposed goals and objectives for HIT within the State
of Utah. We hope to make significant progress towards these goals over the next five years. The
current HIT Strategic Goals from the Digital Health Service Commission include:
GOAL 1: ADVANCE THE HEALTH AND WELL-BEING OF INDIVIDUALS AND
COMMUNITIES THROUGH PERSON-CENTERED AND SELF-MANAGED HEALTH
OBJECTIVES:
• 1A. Increase use of individual health information for engagement and shared decision
making as part of the team – Enable individuals to understand and act upon available cost
and quality information
• 1B. Advance individuals’ abilities to “access, control and amend” their health information
• 1C. Increase adoption and use of patient portals and consumer-focused HIT
• 1D. Promote patient education and use of HIT tools for wellness and self-care
• 1E. Increase effective patient/consumer-mediated and generated exchange
• 1F. Advance individual’s access to and appropriate sharing of public health data
GOAL 2: STRENGTHEN HEALTH CARE DELIVERY TRANSFORMATION
OBJECTIVES:
• 2A. Increase HIT functions to support transparency of and access to quality and cost
information at the community and provider level to improve care
• 2B. Increase implementation of HIT functions to support innovative models of care that
promote high value health care – Medical Home, ACOs, Telehealth
• 2C. Increase use of electronic quality improvement tools and measurements that support
provider adherence to evidence-based guidelines, improved outcomes and reduced waste
• 2D. Support the use of health IT to help providers and communities to better serve high-
risk individuals and populations
GOAL 3: ENHANCE UTAH'S INTEROPERABLE HEALTH IT INFRASTRUCTURE
OBJECTIVES:
• 3A. Endorse basic guidelines for HIT standards that align with and strengthen national
certification requirements, including interoperability, to increase effective health
information exchange
• 3B. Protect privacy and security of electronic health information by increasing adherence
to federal electronic health information security guidelines in independent facilities and
practices
• 3C. Increase functionality and effectiveness of state-wide HIE (CHIE) and support
increased connections with other data sources including integrated delivery systems (IDS),
HIEs, and providers.
• 3D. Increase ability to exchange public health information with providers through various
exchange methods to improve population health
• 3E. Develop governance, access, and support for health data to be made available for
analysis and use
• 3F. Increase Utah’s influence on the national forums related to effective delivery of care
through HIT
• 3G. DHSC will attend conferences to promote interoperability work.
GOAL 4: SUPPORT INNOVATION AND APPLIED RESEARCH TO EFFICIENTLY
IMPLEMENT STATEWIDE HEALTH IT INITIATIVES
OBJECTIVES:
61
• 4A. Promote collaborative innovation and research to advance implementation, utilization
and improvement of health IT in public, private and academic settings
• 4B. Broaden statewide partnership and engagement in implementing the Utah HIT
strategic plan
• 4C. Disseminate evidence-based best practices to enhance statewide adoption of
technology solutions
Applicable Road Maps & Work Flow Diagrams
Utah HITECH Road
Map.pdf
Attachments & References Not Hyperlinked
Appeal Documentation
appeal letter
eMIPP.pdf
HearingRequest201
9.pdf
Environmental Scan
UT_eScan_Report_F
INAL_03-01-2022 (1).pdf
Provider Correspondence
provider approval
email.pdf
provider auto
re-enroll.pdf
provider denial
letter.pdf
provider request
for addtl info - reject.pdf
USIM Grant and Strategic Plan
Utah-HIT-Strategic-
Plan-2016-2020_9-4-2019.pdf
USIM Final
Deliverable Draft Final 07_31_2016 rev (1).pdf
