STATE OF ILLINOIS
DEPARTMENT OF HEALTHCARE AND FAMILY SERVICES
STATE MEDICAID HEALTH INFORMATION
TECHNOLOGY PLAN 2022 UPDATE
MARCH 30, 2022 VERSION 5.0
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page iii
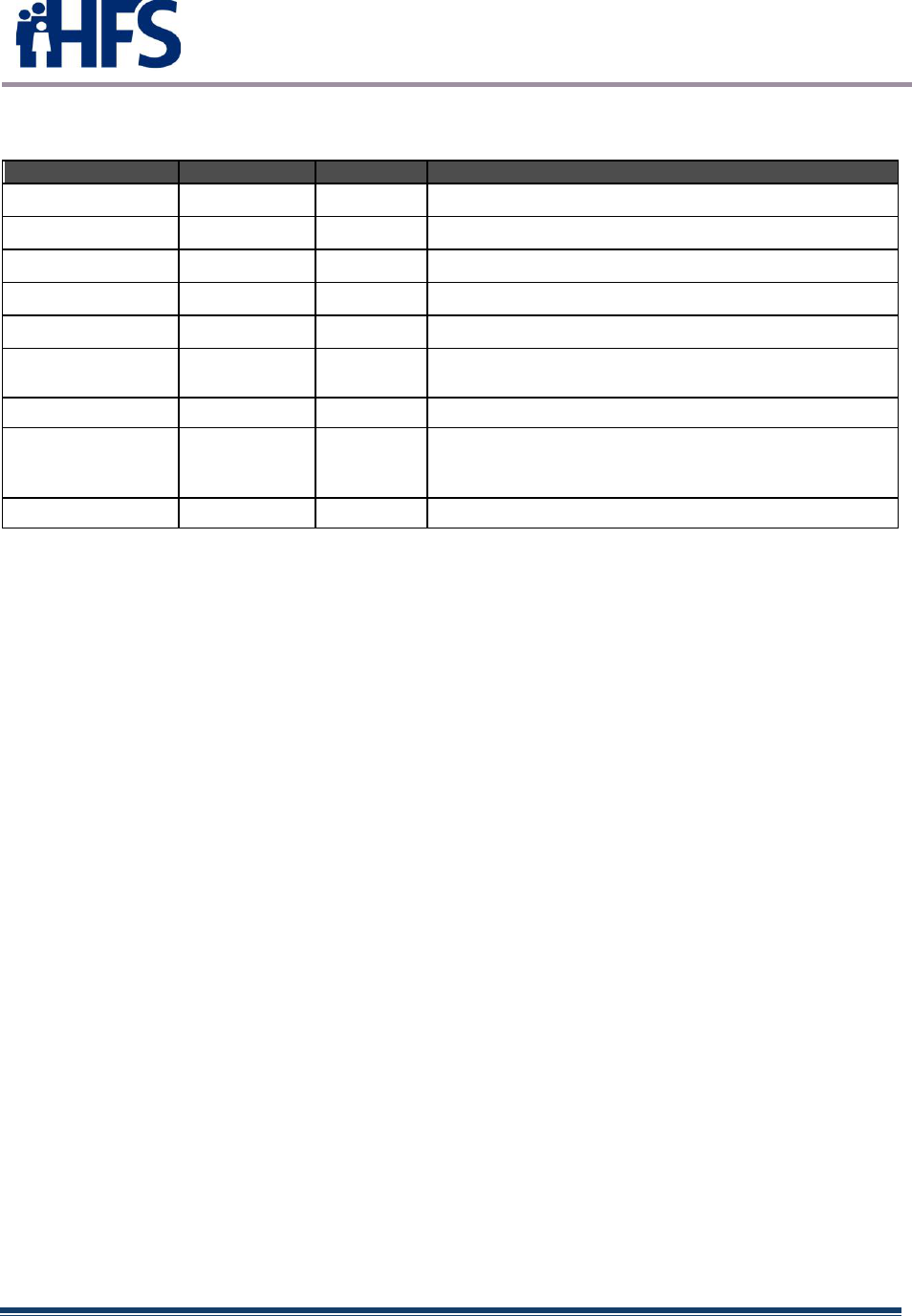
REVISION HISTORY
Version Number
Date
Reviewer
Comments
Version 1.0
04/07/2011
HFS
Initial CMS Submission
Version 2.0
07/01/2011
HFS
Address CMS Comments
Version 2.1
07/28/2011
HFS
Address CMS Comments
Version 2.2
09/23/2011
CMS
Address CMS Comments
Version 2.3
8/31/2012
HFS
Annual SMHP Update; address MU processes
Version 3.0
11/05/2013
HFS
Annual SMHP Update; address new technology
approach
Version 4.0
3/16/2018
HFS
Annual SMHP Update
Version 4.1
7/12/2018
HFS
Responded to CMS comments regarding populations
with unique needs (3.8), attestation tail period
request (4.10).
Version 5.0
3/30/2022
HFS
Final HITECH SMHP Update

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page iv
TABLE OF CONTENTS
1 EXECUTIVE SUMMARY .........................................................................................................1
1.0 BACKGROUND............................................................................................................1
2 CURRENT HIT LANDSCAPE ASSESSMENT – THE AS IS ENVIRONMENT .............................................3
2.1 PURPOSE ...................................................................................................................3
2.2 EHR ADOPTION .........................................................................................................3
2.2.1 ILLINOIS MEDICAID EHR INCENTIVE PAYMENTS..........................................................3
2.2.2 EHR SYSTEMS .....................................................................................................7
2.3 ILLINOIS BROADBAND INITIATIVES...................................................................................8
2.3.1 HIT/HIE CHALLENGES IN RURAL AREAS ..................................................................8
2.3.1.1 BROADBAND ACCESS ........................................................................................8
2.3.1.2 HIE CONCERNS ...............................................................................................8
2.3.1.3 CURRENT BROADBAND COVERAGE......................................................................8
2.4 HIT/HIE ENGAGED STAKEHOLDERS ............................................................................. 10
2.5 HIT/HIE RELATIONSHIPS WITH OUTSIDE ENTITIES .......................................................... 12
2.6 HIE GOVERNANCE STRUCTURE.................................................................................... 13
2.7 MMIS IN CURRENT HIT/HIE ENVIRONMENT.................................................................. 13
2.7.1 MMIS ............................................................................................................. 14
2.7.2 NIPS ............................................................................................................... 14
2.7.3 PHARMACY....................................................................................................... 14
2.7.4 HOSPITAL/DATA ENTRY ..................................................................................... 14
2.7.5 MARS (MEDICAID ANALYSIS AND REPORTING SYSTEM) .............................................. 15
2.7.6 RPR (RECIPIENT, PROVIDER AND REFERENCE)......................................................... 15
2.7.7 FINANCIAL RECOVERY AND ADMIN SYSTEMS ............................................................ 15
2.8 MMIS TO-BE ........................................................................................................... 16
2.8.1 IMPACT PHASE 1: EMIPP ................................................................................... 16
2.8.2 IMPACT PHASE 2: PROVIDER ENROLLMENT............................................................ 16
2.8.3 LATER PHASES OF IMPACT: PBMS AND FULL IMPLEMENTATION.................................. 16
2.9 HIT/MITA COORDINATION ....................................................................................... 17
2.9.1 SUMMARY OF KEY FINDINGS ................................................................................ 18
2.9.2 COMMON THEMES EMERGING FROM THE SS-A ........................................................ 19
2.9.3 CONCLUSIONS.................................................................................................. 19
2.10 SMA ACTIVITIES INFLUENCING THE EHR INCENTIVE PROGRAM........................................... 19
2.10.1 HEALTH TRANSFORMATION COLLABORATIVES ......................................................... 19
2.10.2 BEHAVIORAL HEALTH TRANSFORMATION ............................................................... 22
2.10.3 ILLINOIS HEALTH AND HUMAN SERVICES INNOVATION (HHSI2) .................................. 23
2.10.3.1 ISIP – ILLINOIS SHARED INTEROPERABILITY PLATFORM ............................................. 23
2.10.3.2 ISIP – PROGRAM ACTIVITIES ............................................................................... 23
2.10.3.3 ISIP – USE CASES AND RELATED PROJECTS ............................................................. 25
2.10.4 INTEGRATED CARE FOR KIDS (INCK) ..................................................................... 26

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page v
2.10.4.1 EGYPTIAN PUBLIC & MENTAL HEALTH DEPARTMENT ............................................... 26
2.10.4.2 ANN & ROBERT H. LURIE CHILDREN’S HOSPITAL OF CHICAGO .................................. 27
2.10.5 ELECTRONIC VISIT VERIFICATION (EVV)................................................................. 27
2.10.6 INTEGRATED ELIGIBILITY SYSTEM (IES) ................................................................... 29
2.10.7 ILLINOIS MEDICAID PROGRAM ADVANCED CLOUD TECHNOLOGY (IMPACT) ................. 31
2.10.8 HEALTHCHOICE ILLINOIS ADT .................................................................................. 32
2.10.8.1 HEALTHCHOICE ILLINOIS ADT DESIGN AND DEVELOPMENT ....................................... 32
2.10.8.2 HEALTHCHOICE ILLINOIS ADT IMPLEMENTATION.................................................... 33
2.10.8.3 COMPREHENSIVE MEDICAL PROGRAMS QUALITY STRATEGY ...................................... 34
2.10.8.4 HEALTHCHOICE ILLINOIS ADT FUTURE................................................................. 34
2.11 STATE LAWS OR REGULATIONS ................................................................................... 36
2.11.1 HEALTHCARE TRANSFORMATION COLLABORATIVES ....................................................... 36
2.12 INTERSTATE HIT/HIE ACTIVITIES ................................................................................ 36
2.13 PUBLIC HEALTH INTEROPERABILITY STATUS ................................................................... 37
3 HFS TO BE LANDSCAPE ..................................................................................................... 39
3.1 HIT GOALS AND OBJECTIVES ....................................................................................... 39
3.1.1 HIE AND PUBLIC HEALTH GOALS .......................................................................... 39
3.1.1.1 ENVIRONMENTAL SCAN HIGHLIGHTS ...................................................................... 39
3.1.1.2 HEALTHCHOICE ILLINOIS ADT ............................................................................. 40
3.1.1.3 ATTESTATIONS AND PAYMENTS ............................................................................. 40
3.2 SMA IT SYSTEM ARCHITECTURE................................................................................... 42
3.2.1 PROVIDER ENROLLMENT SYSTEM PROJECT.............................................................. 43
3.2.2 ENTERPRISE DATA WAREHOUSE (EDW) PROJECT .................................................... 44
3.2.3 BACKGROUND AND PURPOSE ............................................................................... 44
3.2.4 CLOUD APPROACH ............................................................................................ 44
3.3 GOVERNANCE STRUCTURES ........................................................................................ 46
4 ADMINISTRATION AND OVERSIGHT ............................................................................. 47
4.1 PROMOTING INTEROPERABILITY PROGRAM STATUS .......................................................... 47
4.2 AUDIT STATUS.......................................................................................................... 47
4.3 REMAINING ILLINOIS MEDICAID PROMOTING INTEROPERABILITY ACTIVITIES .......................... 48
5 EHR INCENTIVE PROGRAM AUDIT STRATEGY....................................................................... 49
6 HIT ROADMAP................................................................................................................ 50
6.1 PATHWAY TO POST-HITECH OPERATIONS ..................................................................... 50
6.1.1 COMPREHENSIVE MEDICAL PROGRAMS QUALITY STRATEGY........................................ 50
6.1.1.1 PURPOSE .......................................................................................................... 50
6.1.1.2 OBJECTIVES ...................................................................................................... 50
6.1.1.3 MISSION ........................................................................................................... 51
6.1.1.4 GOALS ............................................................................................................. 51
6.1.1.5 VISION FOR IMPROVEMENT – PROGRAM GOALS ........................................................ 52
6.1.2 HEALTHCHOICE ILLINOIS ADT.................................................................................... 54
6.1.3 PRESCRIPTION DRUG MONITORING PROGRAM ............................................................... 54

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page vi
6.1.4 PUBLIC HEALTH ....................................................................................................... 54
APPENDIX A: 2021 ILLINOIS ENVIRONMENTAL SCAN ..................................................................... 55
APPENDIX B: LIST OF ACRONYMS .............................................................................................. 56
APPENDIX C: EHR INCENTIVE PROGRAM TASKS.......................................................................... 61

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 1
1 EXECUTIVE SUMMARY
1.0 Background
The State of Illinois, Department of Healthcare and Family Services (HFS) has prepared
this State Medicaid Health Information Plan Update (SMHPU) to report on recent
activities completed by the Illinois Medicaid Electronic Health Record (EHR) Provider
Incentive Payment Program for its Medicaid Eligible Professionals (EPs) and Eligible
Hospitals (EHs), and to inform the Centers for Medicare & Medicaid Services (CMS) of
the progress made toward achieving the vision for transforming healthcare through
adoption and use of EHRs.
Federal CMS implemented through provisions of the American Recovery and
Reinvestment Act (ARRA) incentive payments to EPs, EHs, and critical access hospitals
(CAHs) participating in Medicare and Medicaid programs that are meaningful users of
certified EHR technology. The incentive payments were not intended as a reimbursement
but were made to incent EPs and EHs to Adopt, Implement or Upgrade to (A/I/U) certified
EHR technology. EPs and EHs participating in the Medicaid EHR Incentive Program
qualified in their first year of participation for an incentive payment by demonstrating that
they adopted (acquired and installed); implemented (trained staff, deployed tools,
exchanged data); or upgraded (expanded functionality or interoperability) a certified EHR
solution. Incentive payments were disbursed to providers who demonstrated Meaningful
Use (MU) for an additional five years culminating in 2021.
The Office of the National Coordinator (ONC) issued a closely related Final Rule that
specified the Secretary’s adoption of an initial set of standards, implementation
specifications, and certification criteria for EHR systems. Additionally, the ONC issued a
separate Rule related to the certification of Health Information Technology (HIT).
Goals for the national ONC program for HIE include:
• Enhance care coordination and patient safety
• Reduce paperwork and improve efficiencies
• Facilitate electronic information sharing across providers, payers, and state lines
• Enable data sharing using state HIE and the Nationwide Health Information
Network (NHIN)
Achieving these goals will improve health outcomes, facilitate access, simplify care, and
reduce costs of healthcare nationwide.
HFS continues to work closely with federal and state partners to ensure that the Illinois’
Provider Incentive Payment (PIP) Program fits into the overall strategic plan for the
ILHIE, thereby advancing both the state and national goals for HIE.
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 2
The State Medicaid Health Information Technology Plan (SMHP) was submitted for
consideration by federal CMS on September 23, 2011. The original SMHP was approved
by CMS on November 12, 2011. HFS submitted an annual SMHP Update (SMHPU) on
August 31, 2012, to identify the progress made toward EHR PIP Program goals and
objectives, changes that occurred during the first year of the program, and to provide an
update of planned changes in support of Meaningful Use (MU) Stage 1 attestation. The
SMHP Update was approved by CMS on December 5, 2012, followed by another SMHP
Update approved November 13, 2013. Three SMHP addendums were subsequently
approved, the last one approved by CMS on March 13, 2017. This addendum
documented changes made to the Illinois Medicaid EHR Incentive Payment Program and
systems due to Stage 2 and Stage 3 legislation. Also included were modifications to the
2017 OPPS rule and the 2017 IPPS rule. The most recent IAPD Update, which requested
final year funding f or Illinois’ ADT system implementation and other activities, was
approved on May 7, 2021. The most recent SMHP Update (version 4.1) was approved
September 18, 2018.
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 3
2 CURRENT HIT LANDSCAPE ASSESSMENT – THE AS IS
ENVIRONMENT
2.1 Purpose
This section describes the initiatives, activities, and resources available to the State of
Illinois and how the State is leveraging these existing initiatives, activities, and resources
already dedicated to HIT. In addition to providing a summary of current initiatives and
activities supporting HIT, data was also provided specific to the current rate of EHR
adoption across the State. An environmental scan (see Appendix A) provides baseline
data and guidance in the development of the HIT Roadmap.
2.2 EHR Adoption
2.2.1 Illinois Medicaid EHR Incentive Payments
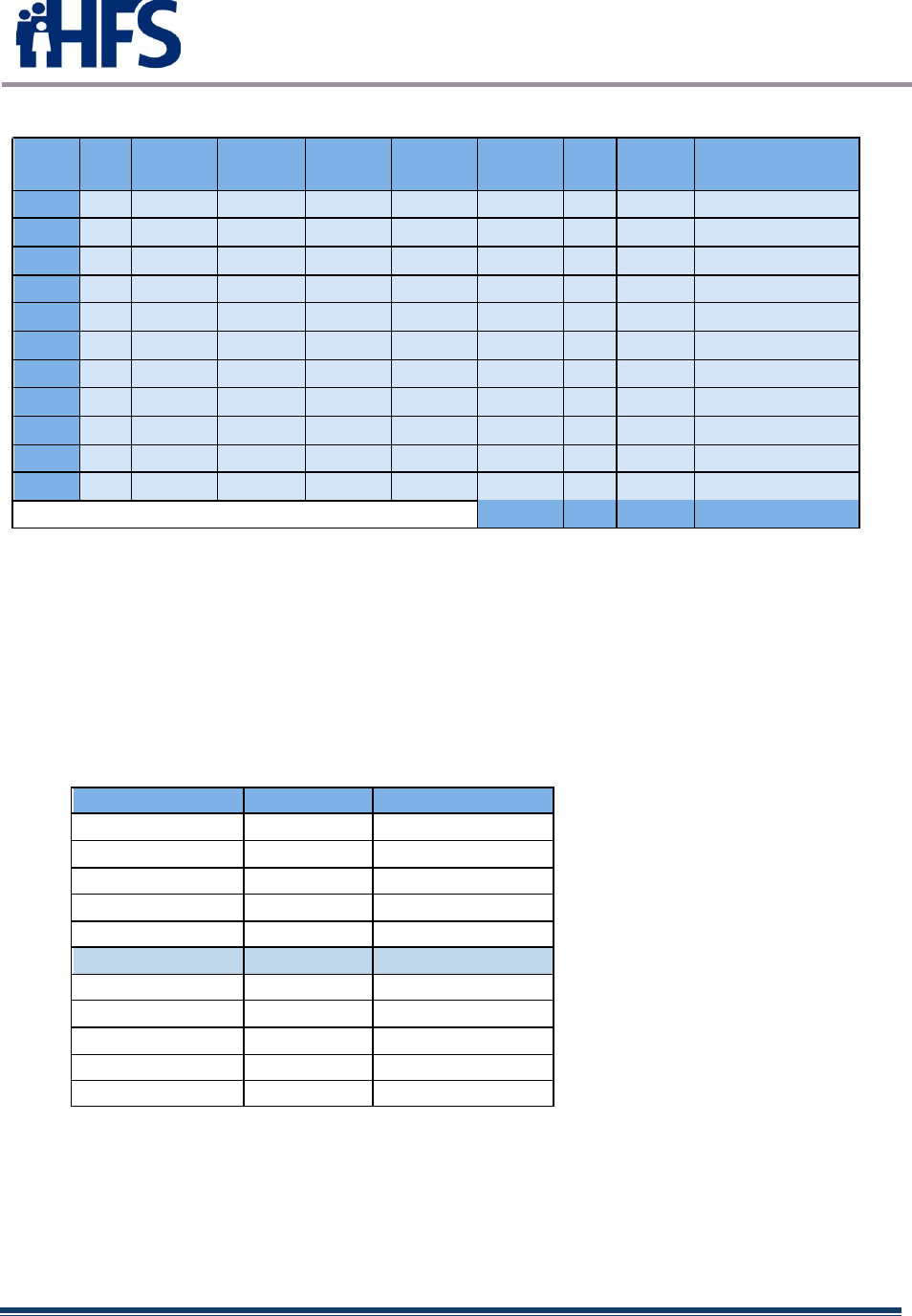
Illinois made its first Medicaid EHR Incentive payment in March 2012. See Figure 1 and
Figure 2 for a yearly breakdown of payments to Eligible Professionals and Eligible
Hospitals below.
Eligible Professionals
YEAR
AIU
MUYR1
MUYR2
MUYR3
MUYR4
MUYR5
MUYR6
MU
TOTAL
Payment
Amount
2011
2156
0
0
0
0
0
0
0
2156
$45,411,269.00
2012
1678
34
554
0
0
0
0
588
2266
$40,654,098.41
2013
1429
46
1475
451
0
0
0
1972
3401
$47,462,602.00
2014
1034
178
967
1129
288
0
0
2562
3596
$45,832,016.00
2015
994
183
1084
852
868
196
0
3183
4177
$50,220,858.00
2016
1270
163
813
800
708
737
170
3391
4661
$57,220,858.00
2017
0
0
739
604
639
506
545
3033
3033
$25,746,154.00
2018
0
0
172
624
533
559
452
2340
2340
$19,855,811.00
2019
0
0
103
84
274
194
223
878
878
$7,457,324.00
2020
0
0
75
101
122
237
162
697
697
$5,913,168.00
2021
0
0
17
70
103
120
205
515
515
$4,366,168.00
Figure 1 – IL Medicaid EP Payments
TOTAL
27720
350,140,326.41
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 4
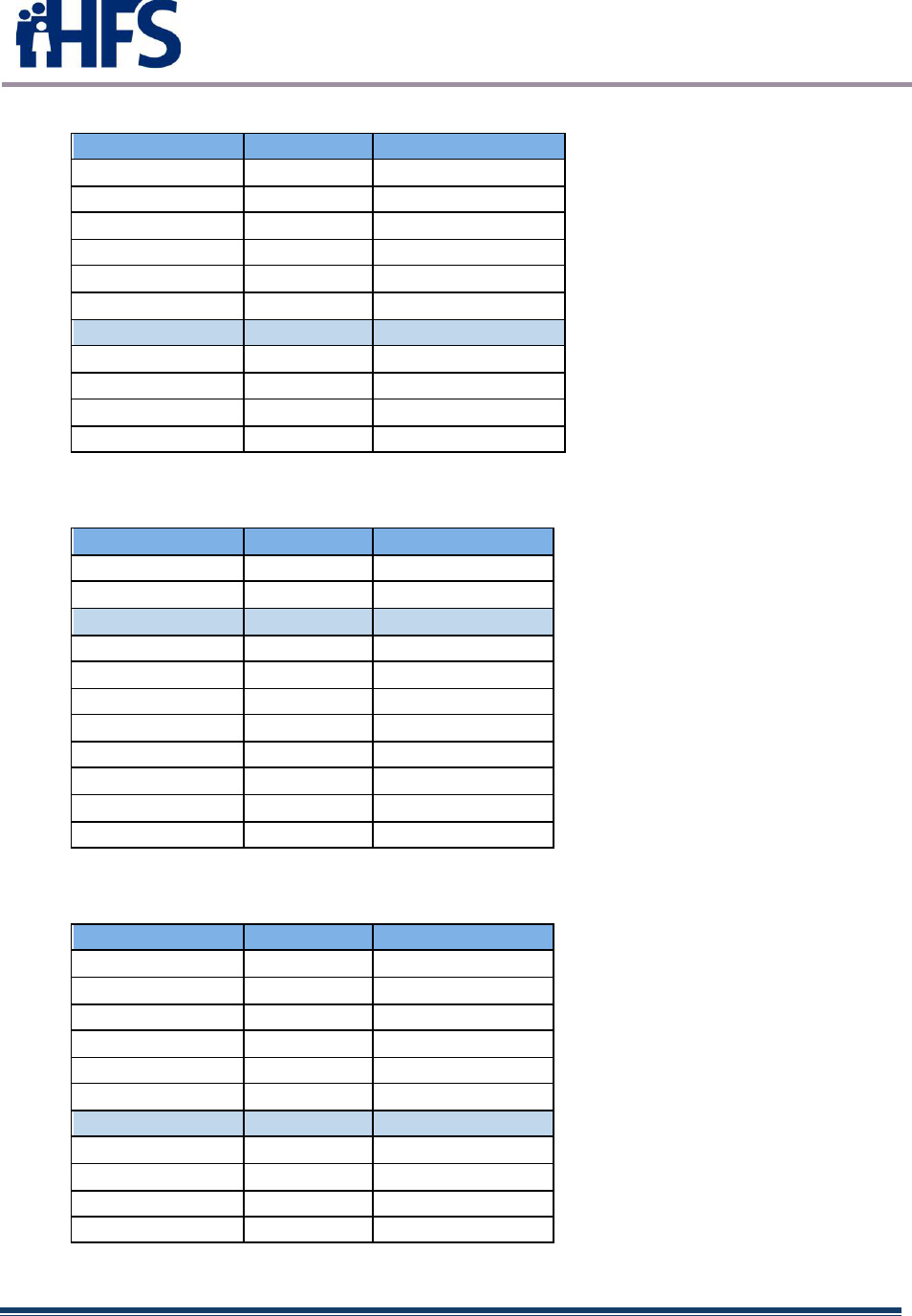
Eligible Hospitals
YEAR
AIU
MUYR1
MUYR2
MUYR3
MUYR4
MUYR5
MU
TOTAL
Payment
Amount
2011
58
34
0
0
0
0
34
92
$91,409,021.00
2012
35
22
67
0
0
0
89
124
$97,558,896.30
2013
12
10
78
65
0
0
153
165
$89,429,620.88
2014
3
0
23
77
14
114
117
$29,659,809.59
2015
0
0
5
21
16
0
42
42
$5,879,666.50
2016
0
0
2
6
3
1
12
12
$937,143.00
2017
0
0
0
2
0
0
2
2
$50,365.00
2018
0
0
0
0
0
0
0
0
$0.00
2019
0
0
0
0
0
0
0
0
$0.00
2020
0
0
0
0
0
0
0
0
$0.00
2021
0
0
0
0
0
0
0
0
$0.00
Figure 2 – IL Medicaid EH Payments
TOTAL
554
$314,924,522.27
Figures 3 -8 below detail the top ten state by payment for both the Medicare and Medicaid
Incentive program from January 2011 through March 6, 2022. This data was derived
from a NLR Microstrategy Payment Summary report, and no attempt was made to
decipher unique payment issues such as Check Void, Bank Info Received, EFT Failed,
etc. For this reason, the statistics below may differ slightly from the Illinois-specific
statistics shown in Figure 1 and Figure 2, which are deemed to be very accurate.
Medicare Only – EP Payments
State/Territory
Total Pymts
Total Amount
California
81,752
$750,431,130.04
Florida
65,647
$620,686,930.80
Texas
63,854
$597,618,455.74
New York
59,577
$550,281,963.79
Pennsylvania
58,451
$530,364,806.59
Illinois
52,508
$479,296,182.36
Ohio
49,150
$426,275,772.25
Michigan
40,652
$371,981,438.36
Massachusetts
41,560
$367,141,094.85
North Carolina
39,750
$359,887,239.42
National Totals
1,092,484
$9,938,256,259.92
FIGURE 3 – Medicare Payments Source: NLR – as of 3/7/2022
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 5
Medicare Only – EH Payments
State/Territory
Total Pymts
Total Amount
Texas
1984
$1,197,010,609.36
California
1392
$1,145,989,405.79
Florida
1128
$1,018,018,572.67
Pennsylvania
984
$785,033,739.98
New York
923
$795,432,536.91
Ohio
918
$21,649,025,920.95
Illinois
834
$672,540,006.85
Michigan
738
$559,894,574.16
Georgia
688
$1,982,567,129.67
Missouri
676
$410,069,879.28
National Totals
23,671
$38,355,061,203.85
FIGURE 4 – Medicare EH Payments Source: NLR – as of 3/7/2022
Medicaid Only – EP Payments
State/Territory
Total Pymts
Total Amount
California
59,721
$813,703,171.70
New York
50,241
$633,358,407.00
Illinois
27,582
$347,252,898.74
Texas
25,906
$336,331,005.00
Ohio
23,876
$303,311,426.00
Massachusetts
21,823
$281,658,401.67
Michigan
21,974
$275,466,573.00
Pennsylvania
21,550
$275,411,310.00
Florida
18,582
$268,349,530.00
Washington
18,961
$247,227,659.97
National Totals
550,188
$7,193,909,430.88
FIGURE 5 – Medicaid EP Payments Source: NLR – as of 3/7/2022
Medicaid Only – EH Payments
State/Territory
Total Pymts
Total Amount
California
1570
$782,588,145.59
Texas
1503
$531,124,624.57
Ohio
873
$228,641,060.40
Pennsylvania
715
$216,550,214.65
Iowa
624
$73,164,928.67
Florida
583
$323,199,833.17
Illinois
577
$317,918,395.38
New York
549
$411,098,513.85
Oklahoma
534
$128,943,464.41
Wisconsin
509
$132,154,696.75
National Totals
17,637
$6,624,512,724.13
FIGURE 6 - Medicaid EH Payments Source: NLR – as of 3/7/2022
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 6
Medicaid and Medicare Combined – EP Payments
State/Territory
Medcr & Medcd
EP Count
Medcr & Medcd
EP Amount
California
141,473
$1,564,134,301.74
New York
109,818
$1,183,640,370.79
Texas
89,760
$933,949,460.74
Florida
84,229
$889,036,460.80
Illinois
80,090
$826,549,081.10
Pennsylvania
80,001
$805,776,116.59
Ohio
73,026
$729,587,198.25
Massachusetts
63,383
$648,799,496.52
Michigan
62,626
$647,448,011.36
North Carolina
57,070
$579,298,012.42
National Totals
1,642,672
$17,132,165,690.80
FIGURE 7 - Combined EP Payments Source: NLR – as of 3/7/2022
Medicaid and Medicare Combined – EH Payments
State/Territory
Medcr & Medcd
EH Count
Medcr & Medcd
EH Amount
Texas
3,487
$1,728,135,233.93
California
2,962
$1,928,577,551.38
Ohio
1,791
$21,877,666,981.35
Florida
1,711
$1,341,218,405.84
Pennsylvania
1,699
$1,001,583,954.63
New York
1,472
$1,206,531,050.76
Illinois
1,411
$990,458,402.23
Iowa
1,285
$332,788,602.39
Wisconsin
1,167
$482,109,600.89
Georgia
1,159
$2,172,410,457.66
National Totals
41,308
$44,979,573,927.98
FIGURE 8 - Combined EH Payments Source: NLR – as of 3/7/2022
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 7
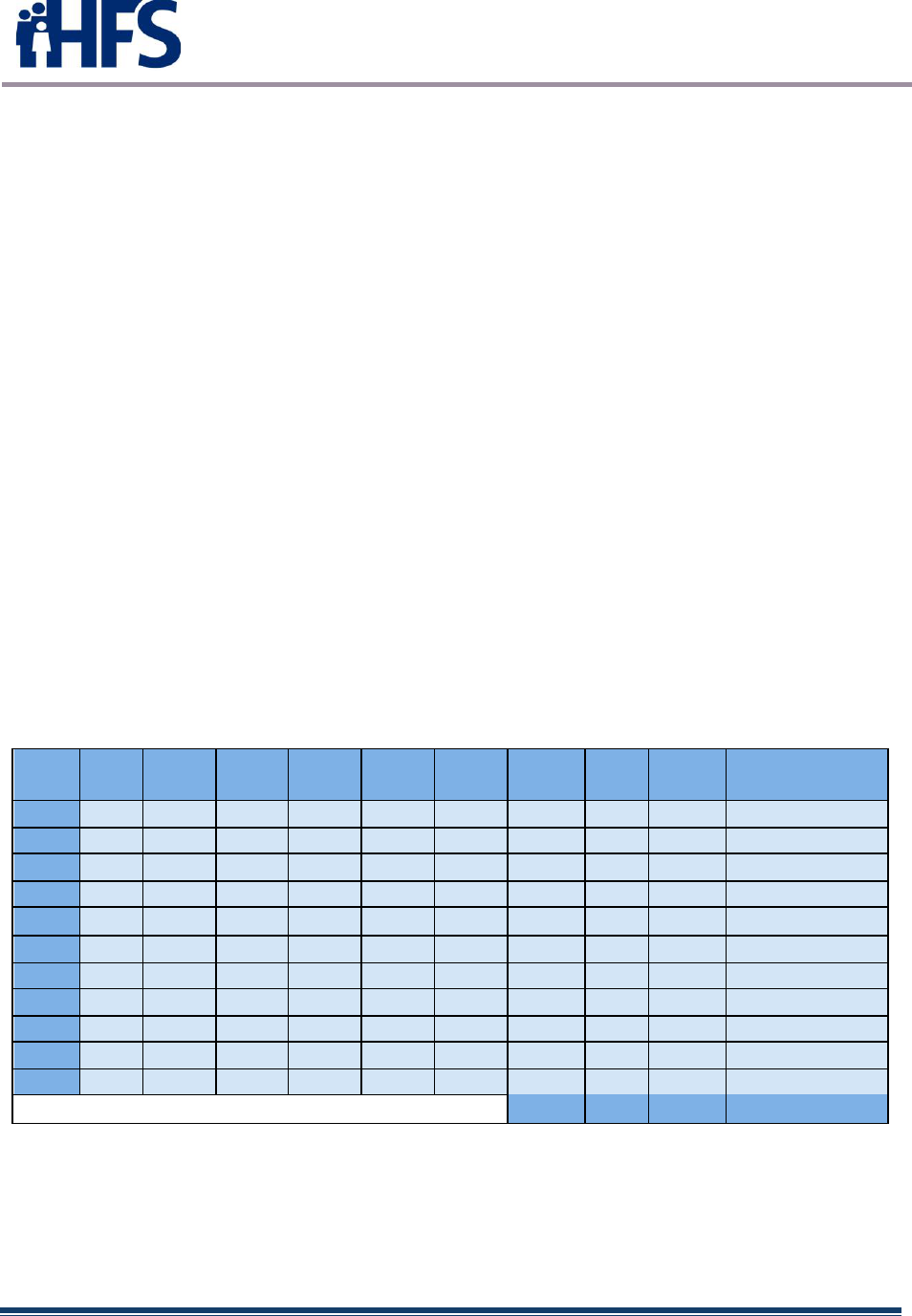
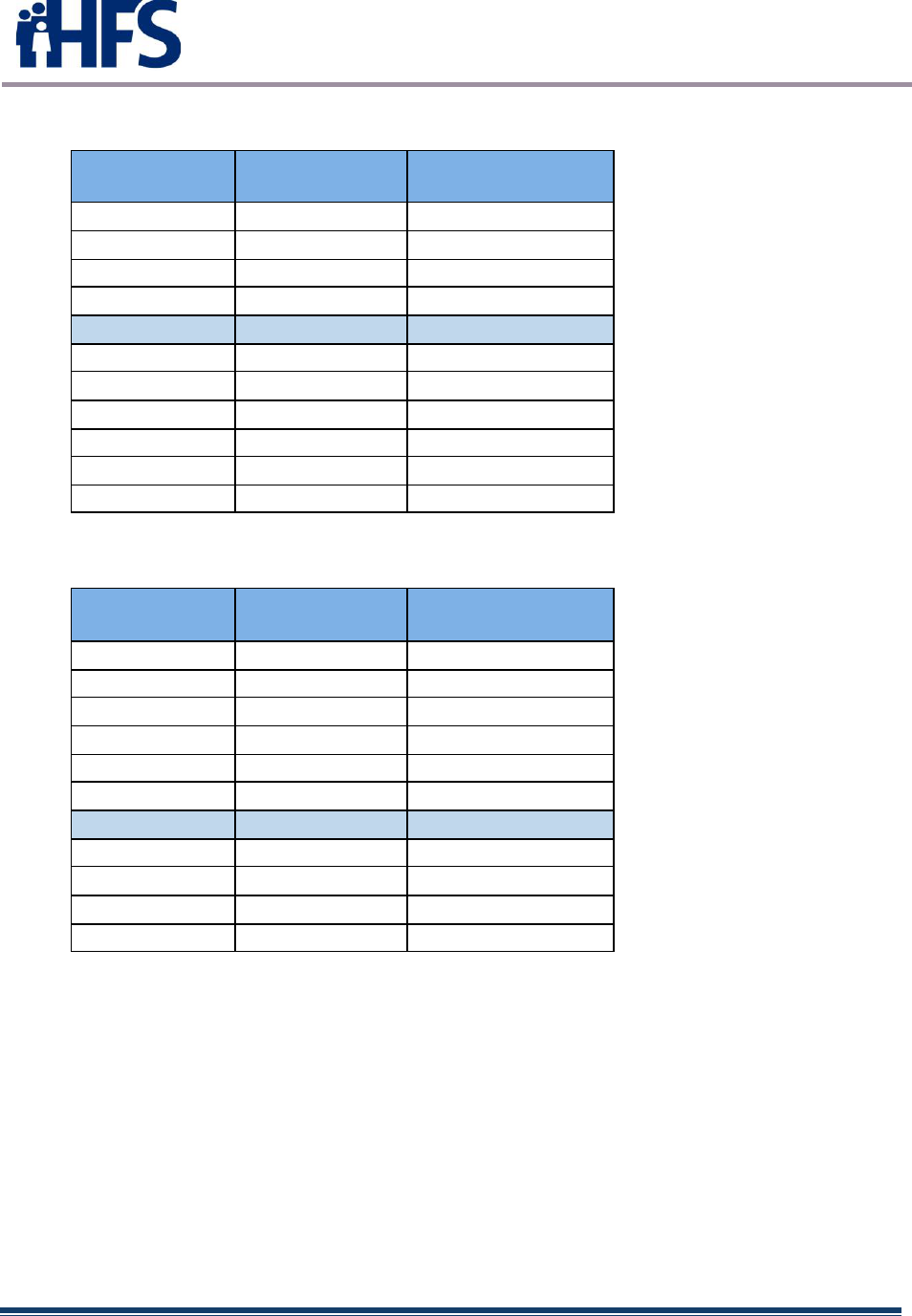
2.2.2 EHR Systems
The charts below (figures 9-10) depict the utilization of EHR Systems in effect in Illinois.
The 2011-2018 EP information was derived from various sources, including IDPH’s
MURS system and the provider. The 2019-2021 EP information was derived from paid
Promoting Interoperability providers 2019-2021. Since providers may change CEHRTs
without re-attesting, this information can never be entirely accurate; however, it does
show trends over a period of years. The first chart reflects the statistics for the EP Vendor
Systems while the second chart reflects use by EH Vendors.
FIGURE 9 EH EHRs *Data as of March 29, 2022
FIGURE 10 Hospital EHRs *Data as of March 21, 2022
EHR Vendor
(EP)
2011-
2018
Count
2011-
2018
Pctg
2019-
2021
Count
2019-
2021
Pctg
EPIC
1787
30%
1337
52%
CERNER
1126
19%
315
12%
ALLSCRIPTS
768
13%
0
0%
GE
CENTRICITY
759
13%
0
0%
NEXTGEN
547
9%
109
4%
eclinicalworks
265
4%
86
4%
ATHENA
200
3%
266
11%
OneTouch
-
0%
333
13%
OTHER
527
9%
108
4%
TOTALS
5979
2554
EHR
Vendor
(EH)
2018
Count
2018
Pctg
2021
Count
2021
Pctg
MEDITECH
48
27%
33
18%
EPIC
35
20%
68
37%
CERNER
26
15%
34
19%
CPSI
21
12%
19
10%
McKESSON
14
8%
13
7%
Medhost
-
-
9
5%
OTHER
32
18%
8
4%
TOTALS
176
184
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 8
2.3 Illinois Broadband Initiatives
Widespread broadband Internet capabilities are essential for the success of HIE
implementation. The sections below describe a number of initiatives supporting the
expansion of Internet access across the State of Illinois, enabling the healthcare
community’s ability to participate in HIE.
2.3.1 HIT/HIE Challenges in Rural Areas
2.3.1.1 Broadband Access
According to BROADBANDNOW as of November 22, 2021, Illinois is both the 6th most
populated State and the 6th highest-ranking State in terms of internet access. The best
broadband coverage in Illinois is concentrated in northeastern counties, with
comparatively less coverage in the southeast. Illinois internet users enjoy an average
download speed of 171.3 Mbps, which is similar to average speeds in top-ranked
States. Affordability data shows that 62.2% (over 7.88 million) of Illinois’ population
has access to a wired internet plan that costs equal to or less than $60 per month. This
is better than the nationwide percentage of consumers with access to the same.
2.3.1.2 HIE Concerns
Many locations do not have access to a HIE or lack awareness of the availability and
benefits of HIEs. Connection costs to HIEs can be prohibitive because of the multiple
connections required to reach multiple HIEs. Healthcare organizations like long term
care and behavioral health have had limited opportunities for connectivity subsidies and
that makes affordability among certain health care sectors more challenging.
Without a mandate or legislative requirement, creating a business case for HIE continues
to be an issue. Larger health systems have been resistant to share data outside of their
networks and affiliations. Additionally, larger EMRs like Epic have the ability to function
like an HIE now and that can reduce the need/demand for a broader based or statewide
HIE. Providers have also turned to vendor mediated exchanges such as Care
Everywhere, Commonwell, Carequality and eHealth Exchange.
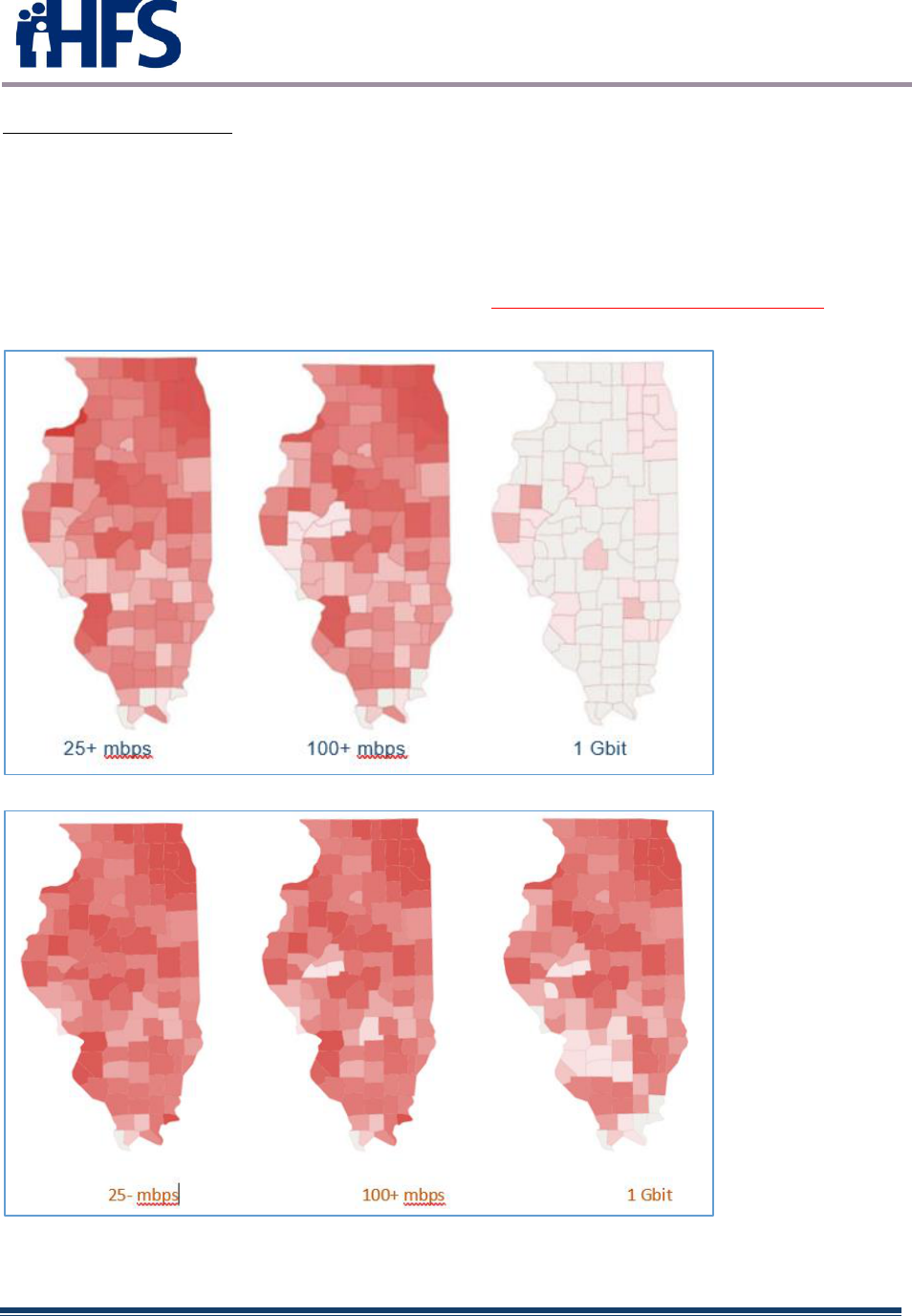
2.3.1.3 Current Broadband Coverage
There are 353 internet providers in Illinois, and over 94% of Illinoisans have access to
wired broadband with speeds of 25mbps or faster. Still, 334,000 people do not have
access to any wired providers. Another 866,000 residents have internet access, yet only
have one provider offering service at their home address. Finally, 727,000 of Illinois
residents that have internet access do not have a connection capable of even 25 Mbps
download speeds. Current gap statistics include:
High-Speed Internet Access
• 93.9% of Illinoisans have access to broadband 100mbps or faster.
• 88.1% of Illinoisans have access to 1 gigabit broadband.
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 9
Wired Internet Access
• 97.5% of Illinoisans have access to wireline service.
• 21.4% of Illinoisans have access to fiber-optic service.
• 92.6% of Illinoisans have access to cable service.
• 93.1% of Illinoisans have access to DSL service.
Illinois is rated as the 6th most connected state and averages 195.8 mbps state-wide.
More information and statistics can be found at www.broadbandnow.com/Illinois .
N ov ember 30, 2017
March 10, 2022
FIGURE 11
Illinois's Broadband: Stats & Figures BROADBANDNOW.
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 10
2.3.1.4 Broadband Grants Received
In the past decade, the State of Illinois has received a significant amount of federal
grant money to fuel the expansion of broadband infrastructure, accounting for 5% of
all federal infrastructure grants.
Additionally, the Illinois Department of Commerce and Economic Opportunity (DCEO)
has launched the ‘Connect Illinois’ initiative with the goal of increasing statewide
broadband access. Part of the initiative features a $400 million broadband grant
program. DCEO also has allocated $79.5 million in Rebuild Illinois programs,
including Fast-Track Public Infrastructure (FTPI), Public Infrastructure, Regional
Economic Development, and Shovel Ready Sites.
2.4 HIT/HIE Engaged Stakeholders
An engaged group of stakeholders has assisted HFS in efforts to increase EHR adoption
and utilization in Illinois. Public and private entities compose this stakeholder group,
each contributing to the task of improving healthcare in Illinois through the use of EHRs.
The Illinois EHR program workgroup met bi-weekly through September 2021 and
included representatives from HFS Medical Programs, HFS Inspector General, the
Illinois Department of Public Health (DPH), the Illinois Department of Human Services
(DHS), Regional Extension Centers and providers representing various hospitals,
physician practices, groups and alliances. Representatives from the Illinois Health and
Hospital association, the Critical Access Hospital Network, the Alliance of Chicago, the
Illinois State Medical Society, Advocate Health Care, and Access Community Health
Network were frequently present as well as many others. HFS updated the group on
program activities including CMS announcements, deadlines and policy changes. The
remainder of the meeting allowed providers to discuss issues and policies related to
HFS, EHR or Medicaid and Medicare. The call was open to all providers as a means to
further engage stakeholders, allowing an opportunity to voice concerns and make
suggestions.
Illinois’ alliance with the State of Michigan regarding support and maintenance of the
eMIPP application was beneficial to both states. The two states shared information on
CMS interpretations of final rules, discussed implementation strategy and shared test
scenarios and results. The result is an application that became more accurate with
regards to CMS policy, had fewer errors and cost less than it would have if each state
were functioning independently. While this partnership was very effective for the
Promoting Interoperability Program, large differences in State policy and goals for MMIS
led to a split of information on September 12, 2021. Despite the split, Illinois and
Michigan representatives of the Promoting Interoperability Program continue to share
issues and ideas with each other regarding the program.
The two Regional Extension Centers in Illinois, CHITREC and IL HITREC, were
contracted to perform outreach activities for the state. The RECs greatly enhanced the
state’s ability to communicate with providers and assist in the expansion and growth of
meaningful use. The RECs also provided HIE knowledge through their associations with
state regional health information organizations (RHIOs).

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 11
Staff from the HFS Office of the Inspector General (OIG) participated in most Illinois
Medicaid incentive program meetings. HFS has occasional meetings with OIG to discuss
auditing requirements of the program and to monitor auditing issues and audit
thresholds. All state audits will be completed by October 1, 2023.
HFS Medical Program staff met periodically with DPH staff. Information regarding Public
Health objectives and sub-measures were discussed. HFS and Public Health have
coordinated policies towards successful provider completion of meaningful measures.
As program policies and regulations evolved or changed, the communication between
the State Medicaid Agency (SMA) and DPH allowed for adapted interpretations of
program requirements.
In an attempt to promote the alignment of the Illinois HIE vendor community to healthcare
business needs, the State of Illinois concluded in 2015 that the State-run HIE, the Illinois
Health Information Exchange Authority (ILHIEA), had proven to be financially
unsustainable and infrequently utilized. The decision was made for ILHIEA to stop
offering technical HIE services in the hope that providers would direct their needs to the
private Illinois RHIO market. While ILHIEA was repurposed to support and promote
private RHIO market growth, provider commitment to existing Illinois HIE options
remained limited. As of late 2016, most IL RHIOs appear to have largely either stalled
due to limited growth achieved or appear to be in the process of closing. As a result,
providers have turned to vendor mediated exchanges such as Commonwell, Care
Everywhere, Careequality, eHealth Exchange and Epic Care Everywhere.
Illinois began a transformation of its health and human services in 2016, stating that the
transformation “puts a strong new focus on prevention and public health; pay f or value
and outcomes rather than volume and services; make evidence-based and data-driven
decisions and move individuals from institutions to community care, allowing patients to
remain more closely connected to their f amily and community.”
In May 2018, the Illinois Department of Healthcare and Family Services (HFS) received
approval of its 1115 Waiver request. This waiver includes pilots designed to better
serve Medicaid beneficiaries in need of behavioral health services. Beginning July 1,
2018, HFS, in partnership with the Department of Human Services/Substance Use
Prevention and Recovery (DHS/SUPR), implemented four substance use disorder
(SUD) specific pilots:
These pilots include Opioid Use Disorder (OUD)/SUD services delivered by providers
currently licensed by SUPR, which are not otherwise matchable expenditures under
section 1903 of the Social Security Act. Providers of Clinically Managed Residential
Withdrawal Management must have the ability to coordinate or provide Medication
Assisted Treatment (MAT) for those patients who need this regimen of care.
Implementation of a state-wide Admission, Discharge and Transfer (ADT) alerting
notification system began in 2021 to advance our care coordination objectives. The
HealthChoice Illinois ADT system has required the engagement of numerous
stakeholders as the system connects Illinois Hospitals, Long Term Care facilities,

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 12
Managed Care Organizations (MCOs) and other willing ambulatory and community
providers. The implementation has required numerous regular meetings with HFS
management, our technology vendor, State technology staff from the Department of
Innovation and Technology (DoIT) and providers around the state. At this date 182
hospitals, 463 Skilled Nursing Facilities, 6 MCOs, 13 Specialized Mental Health
Rehabilitation Facilities (SMHRF), 10 Intermediate Care Facility/Developmental
Disabilities (ICFDD) and 22 Supportive Living Facilities have been connected to the
HealthChoice Illinois ADT system.
2.5 HIT/HIE Relationships with Outside Entities
In addition to the stakeholder relationships listed above, other entities also exist with
which the Illinois Medicaid incentive payment program has a relationship. The
Department of Innovation and Technology (DoIT) is an Illinois State Agency created on
January 25, 2016.
DoIT’s mission is to empower the State of Illinois through high -value, customer-centric
technology by delivering best-in-class innovation to client agencies fostering
collaboration and empowering employees to provide better services to residents,
businesses, and visitors.
DoIT delivers statewide information technology and telecommunication services and
innovation to state government agencies, boards and commissions as well as polic y and
standards development, lifecycle investment planning, enterprise solutions, privacy and
security management, and leads the nation in Smart State initiatives. These initiatives
have resulted from an National Governor’s Association (NGA) effort to help states
identify how they can use information and communication technology (ICT) to enhance
economic development, sustainability, resilience and quality of life across urban,
suburban and rural communities—all while improving the operational efficiency of state
government. NGA is partnering with the state of Illinois, a first mover in smart states
work, and the Smart Cities Council, an association of leading companies that advise
governments across the globe.
DoIT manages the Illinois Century Network, a service that creates and maintains high
speed telecommunications networks providing reliable communication links to and
among Illinois schools, institutions of higher education, libraries, museums, research
institutions, state agencies, units of local government and other local entities providing
services to Illinois citizens.
DoIT launched the First Enterprise Financial Platform (through Enterprise Resource
Planning or ERP), a single system for finance, human resources, procurement, grants
management, asset management and other administrative functions of Illinois agencies.
There are currently 13 agencies up and running on the platform that runs ERP, with an
additional 25 agencies going live on the system in 2018. HFS continues to build a strong
relationship with DoIT as it leads the state in efforts to deliver important technological
solutions for healthcare.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 13
2.6 HIE Governance Structure
The Central Illinois Health Information Exchange (CIHIE) which serviced a region running
from the eastern center to the northeastern area of the state stopped providing services
in February of 2019. The organization explained to their health system members that
their investment in CIHIE was becoming “duplicative”. CIHIE said it still believes that
timely access to patient records minimizes wait time for treatment, reduces costly
duplication of services and supports saf er care. “However, healthcare looks different
today than it did when we began in 2009. There are now viable alternatives to exchanging
data that did not exist when CIHIE was formed.”
At the time, 26 Illinois hospitals were connected to CIHIE, with another 6 connections in
the planning stages. CIHIE also connected 20 primary and specialty care clinics, home
health and behavioral clinics in addition to over 65 long term care facilities.
Until mid-2016, HFS had a strong understanding of another RHIO, Metro-Chicago HIE
(MCHIE). This RHIO was projected to have approximately 70% of the Illinois provider
market share. MCHIE’s technical vendor, Sandlot Solutions, abruptly went out of
business in 2016, disrupting MCHIE operations. In late 2016, MCHIE ceased operations.
Providers have turned instead to vendor mediated exchanges such as Commonwell,
Care Everywhere, Careequality, eHealth Exchange and Epic Care Everywhere.
In January 2018, the Office of the National Coordinator for Health Information
Technology released the Trusted Exchange Framework and Common Agreement
(TEFCA) draft. TEFCA aims to advance nationwide interoperability through a set of
principles designed to facilitate trust among authorized participants and complement
emerging national frameworks that support exchange across multiple networks. A key
goal is to enable providers, hospitals, and other stakeholders to exchange data across
organizational boundaries. Other goals center on improving patient access to their data
and encouraging population-level data exchange.
2.7 MMIS in Current HIT/HIE Environment
Illinois is in the process of modernizing its 40+year-old Medicaid Management
Information System (MMIS) system. In modernizing the dated MMIS system, Illinois has
addressed previous challenges including support for functions such as claims processing
from providers and eligibility verification of Medicaid enrollees.
Several agencies are working together to develop an MMIS that standardizes, expedites
and simplifies processes for providers serving Medicaid clients:
• Illinois Department of Healthcare & Family Services (HFS)
• Illinois Department on Aging (IDoA)
• Illinois Department of Children & Family Services (DCFS)

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 14
• Illinois Department of Human Services (DHS)
○ Division of Substance Abuse Prevention and Recovery (SUPR)
○ Division of Family & Community Services, Bureau of Early Intervention (EI)
○ Division of Developmental Disabilities (DDD)
○ Division of Mental Health (DMH)
○ Division of Rehabilitation Services (DRS)
○ UIC Department of Specialized Care for Children (DSCC)
2.7.1 MMIS
HFS currently manages and operates the MMIS to support claims processing for the
Illinois Medicaid Enterprise. The MMIS environment includes the database subsystems
(e.g., Provider, Recipient, Reference and Prior Approval); the Hospital, Pharmacy and
NIPS claims processing subsystems; the Management and Reporting System (MARS);
the Enterprise Data Warehouse; the Pharmacy point of sale system and the web-based
applications provided in the Medical Electronic Data Interchange(MEDI) system.
2.7.2 NIPS
The Non-Institutional Practitioner Subsystem adjudicates services provided to clients by
Non-Institutional Providers such as physicians, pharmacists, optometrists, podiatrists,
medical transportation providers, clinics and suppliers of medical equipment.
2.7.3 Pharmacy
The Illinois Medicaid program covers prescription drugs, as well as some “over the
counter” (OTC) products, made by manufacturers that have a signed rebate agreement
with the federal Centers for Medicare and Medicaid Services (CMS). Some prescription
drugs and OTC products require prior approval from HFS before reimbursement.
The ILLINOIS Rx Portal is a web-based collection of tools for prescribers, pharmacies,
and HFS staff. It provides a secure interface for providers to look up participant eligibility,
view participant drug history, view drug formulary information, Preferred Drug List (PDL)
criteria, and submit and confirm Prior Authorization (PA) requests online. Prescribers are
guided through preferred or non-preferred selections, as well as potential step therapy,
dose limits, or other PDL criteria to allow them the ability to make informed drug choices.
Information is tailored to each type of user: prescriber, pharmacist, hotline staff, or state
administrator.
2.7.4 Hospital/Data Entry
The Hospital subsystem adjudicates services provided to clients by hospitals, nursing
homes, the Office of Alcohol and Substance Abuse (OASA), and state-operated long-
term care facilities.
A hospital must be enrolled for the specific category of service (COS) for which charges
are to be made.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 15
The categories of service for which a hospital may enroll are:
COS Service Definition
• 020 Inpatient Hospital Services (General)
• 021 Inpatient Hospital Services (Psychiatric)
• 022 Inpatient Hospital Services (Physical Rehabilitation)
• 024 Ambulatory (Outpatient) Hospital Services (General)
• 025 Ambulatory (Outpatient) End Stage Renal Disease Services
• 027 Ambulatory Services (Psychiatric Clinic Type A)
• 028 Ambulatory Services (Psychiatric Clinic Type B)
The standard fee-for-service categories of service assigned are:
• 001 Physician Services
• 011 Physical Therapy Services
• 012 Occupational Therapy Services
• 013 Speech Therapy/Pathology Services
• 014 Audiology Services
• 017 Anesthesia Services
• 030 Healthy Kids Services
2.7.5 MARS (Medicaid Analysis and Reporting System)
The MMIS MARS unit is responsible for the maintenance of the repository of long-term
history of paid and rejected Medicaid claims and produces hundreds of ongoing reports
of expenditures, service provision, program effectiveness, and processing statistics.
2.7.6 RPR (Recipient, Provider and Reference)
The Recipient/Provider Reference (RPR) unit maintains subsystems that support the
claims processing and reporting systems. Information on client and provider eligibility
data as well as medical treatment (procedure codes) and illness (diagnosis codes)
information is available.
The RPR unit is also responsible for many critical system interfaces to other agency
systems and to outside entities and maintains the eligibility programs that are used by
Recipient Eligibility Verification (REV) System, the Automated Voice Response System
(AVRS) and the Medical Electronic Data interchange (MEDI) system.
2.7.7 Financial Recovery and Admin Systems
The Third-Party Liability (TPL) and Technical Recovery units are responsible for the
systems used to recover funds paid by the agency for health claims and medical and
financial assistance. The Admin Systems area is responsible for the suppor t of various
programs used for Healthcare Purchasing, tape generation for daily mainframe job
streams, and support of the Systems Warehouse & Asset System (WAMS) for equipment
and commodities for HFS.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 16
2.8 MMIS To-Be
The current MMIS was fully implemented in 1982 and was primarily built to support a
fee-for-service Medicaid program. Throughout the years, HFS made many
enhancements and modifications to the MMIS; however, it is an older legacy system that
is becoming increasingly more difficult to maintain and modify. Additionally, the federal
Centers for Medicare and Medicaid Services (CMS) has since developed the Medicaid
Information Technology Architecture (MITA), a national framework to support improved
systems development and health care management.
Rather than develop a new system, Illinois obtained a fully operational, federally-certified
MMIS partnership with the State of Michigan. This cloud-based approach aimed to
decrease up-front development costs and was expected to reduce the time required for
implementation.
2.8.1 IMPACT Phase 1: eMIPP
The first phase of IMPACT included the launch of the Electronic Health Records Medicaid
Incentive Payment Program (eMIPP), which provided incentive payments to eligible
professionals and hospitals to adopt, implement, upgrade or demonstrate meaningful
use of certified electronic health records (EHR) technology. Illinois began issuing
incentive payments in 2012; the eMIPP system entered production on November 18,
2013. Incentive payments continued through 2021. eMIPP was moved to Cloud
technology in October 2016 as part of the joint MMIS effort with the State of Michigan.
On September 12, 2021, eMIPP was relocated again to an Amazon Cloud environment
(AWS) as the joint effort with Michigan ended. The eMIPP system continues to be
operational and is currently necessary to complete program auditing requirements.
2.8.2 IMPACT Phase 2: Provider Enrollment
In July 2015, providers seeking to serve Medicaid clients were required to enroll and
revalidate through the new IMPACT web portal. Paper enrollment applications or updates
were replaced by the on-line system and email has become the primary method for
provider communication.
Existing Medicaid providers enrolled in the current legacy MMIS were required to
revalidate their information in IMPACT. Subsequently, providers who deliver services
through Medicaid waiver programs, including providers previously not required to enroll
in MMIS, were required to enroll in IMPACT beginning in 2016.
On September 12, 2021, the Provider Enrollment component of IMPACT was relocated
to an Amazon Cloud environment (AWS) as the joint effort with Michigan ended.
2.8.3 Later Phases of IMPACT: PBMS and Full Implementation

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 17
In 2017, IMPACT launched the new Illinois Rx Portal Pharmacy Benefits Management
System (PBMS). The ILLINOIS Rx Portal is part of the Illinois MMIS system upgrade and
gives prescribers and pharmacies quick and secure web-access for processing and
managing pharmacy benefits including:
• Viewing participant eligibility
• Submitting prior authorizations (PAs)
• Checking the status of submitted PA requests
• Viewing preferred drug list (PDL) criteria
• Viewing drug formulary information
The new system gave users alternatives to phone and fax for submitting PAs and
following up on PA status.
Prescribers and pharmacies must be enrolled and approved in IMPACT to access the
ILLINOIS Rx Portal. Once they are an approved provider, they receive an e-mail with the
instructions for accessing the Portal.
On March 30, 2021, HFS signed a 4-year contract with CNSI to replace core elements
of its legacy MMIS with a more modern MMIS. The contract requirements include:
• The “Core: must be c ap able o f ret aining elig ibility inf ormation o f ind ividuals covered b y
the several healthcare plans of the Department and adjudicating claims f or services
provided under those health care plans.
• The “Core” must support Managed Care programs f or members, cost avoidance, and
other demands f or payment, payment reconciliation, and mandatory reporting.
• IMPACT Core must be designed and implemented in a manner that ensures it will
successfully complete Health and Human Services (HHS)/Centers f or Medicare and
Medicaid Services (CMS) certification.
The contract also continues ongoing support for IMPACT Provider Enrollment and the
IMPACT eMIPP application (auditing support\system support for the Promoting
Interoperability program).
2.9 HIT/MITA Coordination
HFS contracted Cognosante to perform a MITA State Self -Assessment (MITA SS-A) for
the Medicaid Information Technology Architecture (3.0). The May 2017 SS-A describes
the utilization of shared technology and business processes to advance Illinois’
healthcare transformation. The transformation aims to achieve its mission of providing
quality healthcare coverage at sustainable costs for the people, families, and
communities of Illinois.
Illinois is in the process of modernizing its 40+ year-old MMIS, and other systems that
comprise its Medicaid Enterprise. In 2013, HFS entered an Intergovernmental Agreement
(IGA) with the state of Michigan’s Department of Health and Human Services (MDHSS)
to begin a feasibility study to determine the viability and practicality of a shared Medicaid
Enterprise between the two states. The resulting IMPACT project was a multi-phase

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 18
initiative to deliver to HFS a state-of-the art federally certified MMIS through a cloud-
enabled service as well as Medicaid Enterprise modules for:
• Provider Enrollment (PE)
• Reference and Prior Approval
• Management and Reporting (MARS)
Although the agreement with Michigan ends June 30, 2022, the IMPACT functionality
listed above will continue on an Amazon Cloud environment.
The guiding principles established for this assessment were aligned with those
documented in the Illinois HFS 2015 annual report, completed in March of 2016:
• Beneficiaries should receive the right care, at the right time, at the right cost
• Care should be holistic – integrating the physical and mental health needs of
beneficiaries
• Care should be evidence-based to deliver the best quality at the lowest cost
• Pay for what works to improve and maintain health and stop paying for what
doesn’t work
• Transform health care to a system focused on prevention and keeping
beneficiaries healthy
• Prevent chronic disease whenever possible, coordinate care to improve quality of
life and reduce chronic care costs
• Enable seniors and people with disabilities to live in their homes or community-
based settings, instead of a higher-cost setting like a nursing home
HFS has a multi-pronged strategy with numerous initiatives to address healthcare
challenges across the State’s Medicaid Enterprise. The overarching strategies are:
• Facilitate integration and decrease system fragmentation
• Automate repeated manual tasks and processes, where feasible
• Reduce processing time of requests for services
• Improve care planning and delivery
2.9.1 Summary of Key Findings
The report found that HFS was operating at an “As Is” MITA Maturity Level of 1 across
the MITA business areas. Most the capability scores operated at a Level 1 and a few
areas at a Level 2, with most reliant on fragmented systems and manual processes.
While technology improvement projects, such as Health-e-Illinois Plus (HEAplus),
provided significant capability improvements in some business areas, HFS was found to
have manual data entry and fragmented processes across programs and business areas.
HFS will focus future development on automation and implementing standard data and
processes; however, many of the MITA Level 3 capabilities still lack national standard
definitions. For this reason, HFS seeks to standardize and automate to the fullest extent
of MITA Level 2 and will explore MITA Level 3 standards as they are developed and
adopted by CMS.
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 19
2.9.2 Common Themes Emerging From the SS-A
Subject matter experts across the different business areas identified several areas where
current operations would benefit from improvements such as standard data storage,
exchanges of data, and the way business processes are shared and completed across
the enterprise.
There are several underlying themes found to provide both a foundation for decision-
making and a challenge to the Illinois Medicaid Enterprise’s ability to meet and exceed
the targeted MMLs identified by the SMEs.
2.9.3 Conclusions
Several key HFS projects achieved the objectives from its 2009 MITA SS-A. However,
some key capabilities must still be met to fully move business, technical, and information
capabilities to higher MMLs. Limited resources, funding, staff shortages and managing
the many new state and federal initiatives have been key constraints in successful
completion of projects. However, HFS is intent to fully utilize federal funding
opportunities to complete the projects and project planning initiatives on its To Be
Roadmap.
On a scale of MML 1 to 5, the Illinois Medicaid Enterprise, in large part, was assessed
at Level 1 with a goal to be at Level 2, and in some cases Level 3, within a 5-year
timeframe. Of the six projects included in the “To Be” Roadmap, the IMPACT project is
currently in process. As HFS completes the improvements identified in the roadmap, the
net effect is that the “To Be” items identified in HFS’ M ITA Maturity Capability Matrix will
become the new “As Is”. Ongoing assessment cycles should ensure the appropriate
business process and technical capability documentation remains current and
establishes the new “To Be” Maturity Levels. This will form the foundation for subsequent
projects, streamline planning and support the new methodology chosen for the Medicaid
Enterprise.
2.10 SMA Activities Influencing the EHR Incentive Program
2.10.1 Health Transformation Collaboratives
On March 8, 2021, HFS announced the Healthcare Transformation Collaboratives
program. As outlined in Public Act 101-650 and SB 1510, the program is designed to
improve healthcare outcomes, reduce healthcare disparities, and realign resources in
distressed communities throughout Illinois. In particular, the program seeks to increase
access to community-based services, preventive care, obstetric care, chronic disease
management, and specialty care in these communities.
The legislation states “During State fiscal years 2021 through 2027, the hospital and
health care transformation program shall be supported by an annual transformation
funding pool of up to $150 million pending federal matching funds, to be allocated during
the specified fiscal years for the purpose of facilitating hospital and health care
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 20
transformation”. This investment will fill healthcare gaps and focus on underlying health
conditions in areas high on the federal Centers for Disease Control and Prevention's
social vulnerability index scale, communities that have been disproportionately affected
by the COVID-19 pandemic and areas served by critical access and safety net hospitals,
including rural parts of the state.
On July 1, 2021, Governor JB Pritzker announced $94.3 million to be awarded in the
state’s inaugural round of Healthcare Transformation Collaboratives funding. HFS would
administer the awards to eight innovative partnerships across the state, “ with the goal of
reorienting healthcare in Illinois to reduce healthcare inequities, improve health
outcomes, address social determinants of health, and remedy persistent d ifficulty for
underserved communities to access quality healthcare.”
At the time of the announcement, two additional collaboratives were listed as being
advanced for further consideration and potential funding. One of these, the Medicaid
Innovation Collaborative, was later approved, bringing the total of funded collaboratives
to nine. The nine awardees that comprised the first round of funding are:
Chicago North Side Collaborative: A proposal to mitigate barriers to specialty care and
increase health equity among the communities it serves.
Participating Entities:
Swedish Hospital
Erie Fam ily Health Centers
Heartland Health Centers
Hamdard Healthcare
Asian Human Services Family Health Center
Howard Brown Health
Medical Express Ambulance Service, Inc. d/b/a MedEX Ambulance Service
Collaborative Bridges: A plan to improve behavioral health and other health
outcomes and reduce healthcare costs by creating an unprecedented continuity of care
between hospital and community.
Participating Entities:
Community Counseling Centers of Chicago
Habilitative Services, Inc.
Humboldt Park Health
Hartgrove Hospital (UHS)
The Loretto Hospital
East St. Louis Health Transformation Partnership: A proposal to affect large scale
realignment of the health delivery system and improve the life circumstances of those
living in the East St. Louis Metro Area.
Participating Entities:
Touchette Regional Hospital
SIHF Healthcare
SIU School of Medicine
Hoyleton Youth and Family Services
Centene
Memorial Medical Group
ConferMed Weitzman Institute
Washington University
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 21
Comprehensive Behavioral Health Center
Zade, Inc
Integrated Hub: A collaborative to enhance quality of care for adult Medicaid
beneficiaries with behavioral health, substance use disorder, and physical health
needs.
Participating Entities:
Egyptian Health Department
Eldorado Rural Health Clinic
Gallatin County Wellness Center
Harrisburg Medical Center
Ferrell Hospital
Southern Illinois Healthcare
Fairfield Memorial Hospital
SIU Multicultural Center
Medicaid Innovation Collaborative: Addressing systemic obstacles and technology
gaps that individuals and technology gaps that individuals and families face in
accessing quality health care.
Participating Entities:
OSF Healthcare
Aunt Martha ’s Health Ce nter
Chestnut Family Health Center
Heartland Health Service
Eagle View Community Health System
Mile Square Health Center
Supportive Reentry Network Collaborative: A model approach to care coordination
and social determinants of health for men and women released from incarceration
returning to Cook County.
Participating Entities:
Safer Foundation
Heartland Alliance Health
Cook County Health
Healthcare Alternative Systems, Inc. (HAS)
KAM Alliance
Transforming Reentry Services/MWPM
Get To Work Illinois
Smart Policy Works
Legal Council for Health Justice
South Side Healthy Community Organization: A collaborative driven by community
input and dedicated to fundamentally advancing healthcare access and better health
outcomes for Chicago's South Side residents.
Participating Entities:
St. Bernard Hospital
Advocate Aurora Healthcare
Beloved Community Family Wellness Center
Chicago Family Health Center
Christian Community Health Center
Friend Family Health
Jackson Park Hospital and Medical Center
Near North Health
Roseland Hospital
St. Bernard Hospital
Sinai Chicago
South Shore Hospital Corporation
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 22
TCA Health
The University of Chicago Health System
55
th
& Pulaski Health Collaborative: A collaboration with an ‘all-in’ approach to
improve access to a wide range of healthcare services and improve the health and
wellness of individuals and the entire community.
Participating Entities:
UI Health Physician Group (UIPG)
Mile Square Health Center
Alivio Medical Center Primary
University of Illinois College of Applied Sciences Depts of Physical Therapy, Occupational Therapy and
Nutrition
West Side Health Equity Collaborative: A plan to increase convenient access to
culturally responsive healthcare, supporting the unique and changing socio-economic
needs of individuals and families.
Participating Entities:
Access Community Health Network
Ann & Robert H. Lurie Children's Hospital of Chicago
Bobby E. Wright Comprehensive Behavioral Health Center, Inc
Cook County Health
Habilitative Systems, Inc
Humboldt Park Health
The Loretto Hospital
Medical Home Network
Rush University Medical Center
Sinai Chicago
West Side United
On October 6, 2021, HFS announced that applications for the second round of Healthcare
Transformation Collaboratives funding were being accepted. The deadline for the fiscal year
2022 round of Healthcare Transformation Collaboratives funded ended November 19, 2021,
and public comment period ended December 20, 2021.
2.10.2 Behavioral Health Transformation
Illinois began a transformation of its health and human services in 2016, stating that the
transformation “puts a strong new focus on prevention and public health; pay for value
and outcomes rather than volume and services; make evidence-based and data-driven
decisions and move individuals from institutions to community care, allowing patients to
remain more closely connected to their family and community.”
In May 2018, the Illinois Department of Healthcare and Family Services (HFS) received
approval of its 1115 Waiver request. This waiver includes pilots designed to better
serve Medicaid beneficiaries in need of behavioral health services. The 1115 SUD
waiver approval period is from July 1, 2018, through June 30, 2023.
Beginning July 1, 2018, HFS, in partnership with the Department of Human
Services/Substance Use Prevention and Recovery (DHS/SUPR), implemented four
substance use disorder (SUD) specific pilots:
• Residential/Inpatient SUD Treatment in an IMD.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 23
• Case Management to individuals with an SUD that qualify for diversion into treatment from the
criminal justice system.
• Peer Recovery Support Services.
• Clinically Managed Residential Withdrawal Management for individuals with SUD.
These pilots include Opioid Use Disorder (OUD)/SUD services delivered by providers
currently licensed by SUPR, which are not otherwise matchable expenditures under
section 1903 of the Social Security Act. Providers of Clinically Managed Residential
Withdrawal Management must have the ability to coordinate or provide Medication
Assisted Treatment (MAT) for those patients who need this regimen of care.
In the first three years of the 1115 SUD demonstration (July 1, 2018, through June 30,
2021) there were an estimated:
• 8000 individuals who received treatment through the SUD residential IMD Pilot.
• 2300 individuals who were enrolled in SUD case management services.
• 107 individuals enrolled in Peer Recovery Support Pilot.
• 61 individuals enrolled in the Clinical Withdrawal Management Pilot.
2.10.3 Illinois Health and Human Services Innovation
(
HHSi2)
The Illinois Health and Human Services Innovation Incubator (HHSi2) is a program
office within the Illinois Governor’s Office of Management & Budget. HHSi2 partners
with HFS, DHS, the Department on Aging, Department of Children & Family Services,
Department of Veterans’ Affairs and IDPH, and is supported by DoIT. HHSi2 seeks to
drive innovation and improve the delivery of health and human services programs
throughout the state.
2.10.3.1 ISIP – Illinois Shared Interoperability Platform
The Illinois Shared Interoperability Platform (ISIP) is the cornerstone of HHSi2’s
mission. Approved by the Centers for Medicare and Medicaid Services (CMS) and
United States Department of Agriculture’s Food and Nutrition Service (FNS), ISIP is
funded via a 90/10 federal match.
The goal of ISIP is to provide coordinated and collaborative service delivery by
establishing an interoperable environment for stakeholders of Health & Human
Services (HHS) programs, which will integrate data from disparate sources and provide
a comprehensive 360-degree view of the full complement of services a specific person
and their respective family or household receives across all Illinois HHS agencies.
ISIP will enable State agencies to securely access more accurate and reliable data
across the HHS enterprise to support better decision making and improve the delivery
of critical services to those in need.
2.10.3.2 ISIP – Program Activities

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 24
• ISIP installation has been completed in all environments. There are now seven
data source systems that have been profiled and added to ISIP:
o Statewide Automated Child Welfare Information System (SACWIS) Data
Warehouse
o Electronic Community Care Program Information System (eCCPIS)
o Early Intervention (EI)
o Child Care Management System (CCMS)
o Integrated Eligibility System (IES -SNAP and TANF data only)
o CyberVet
o Offender 360
Requirements are being collected to prepare for inclusion of Women Infants and
Children (WIC) data in ISIP.
• A pilot was conducted with the Department of Children & Family Services’
(DCFS) State Central Register and Child Protection teams to cleanse addresses
and de-duplicate records, which will improve mailability of correspondence,
reduce rework, improve the accuracy of person records, and enhance the
agency’s ability to ef fectively serve children and f amilies.
• Collaborative use cases began with DHS and Department on Aging to increase
senior adult awareness of and enrollment in Women, Infants, and Children
(WIC) and Supplemental Nutrition Assistance Program (SNAP).
• Collaboration is continuing with Departments of Veterans’ Affairs, Corrections
and Aging on a use case to prevent duplication of services to senior adults.
• HHSi2 was asked to partner with the Illinois Commission to End Hunger, the
Illinois Commission on the Elimination of Poverty and DHS to leverage the
benefits of ISIP in support of Code for America’s initiative to “transf orm the
social safety net by utilizing human-centered technology” particularly improved
SNAP service delivery and digital pathways to WIC.
• Installation and preliminary testing of Informatica Enterprise Data Catalog (EDC)
and Axon Data Governance solutions in development and production
environments has been completed. EDC and Axon are AI-powered tools that use
machine learning to scan and catalog data assets across the enterprise to help
agencies better understand their data assets and locate data more effectively.
• Development has been completed concerning the ISIP Target Operating Model,
Organizational Change Management Playbook and the Risk Management Plan.
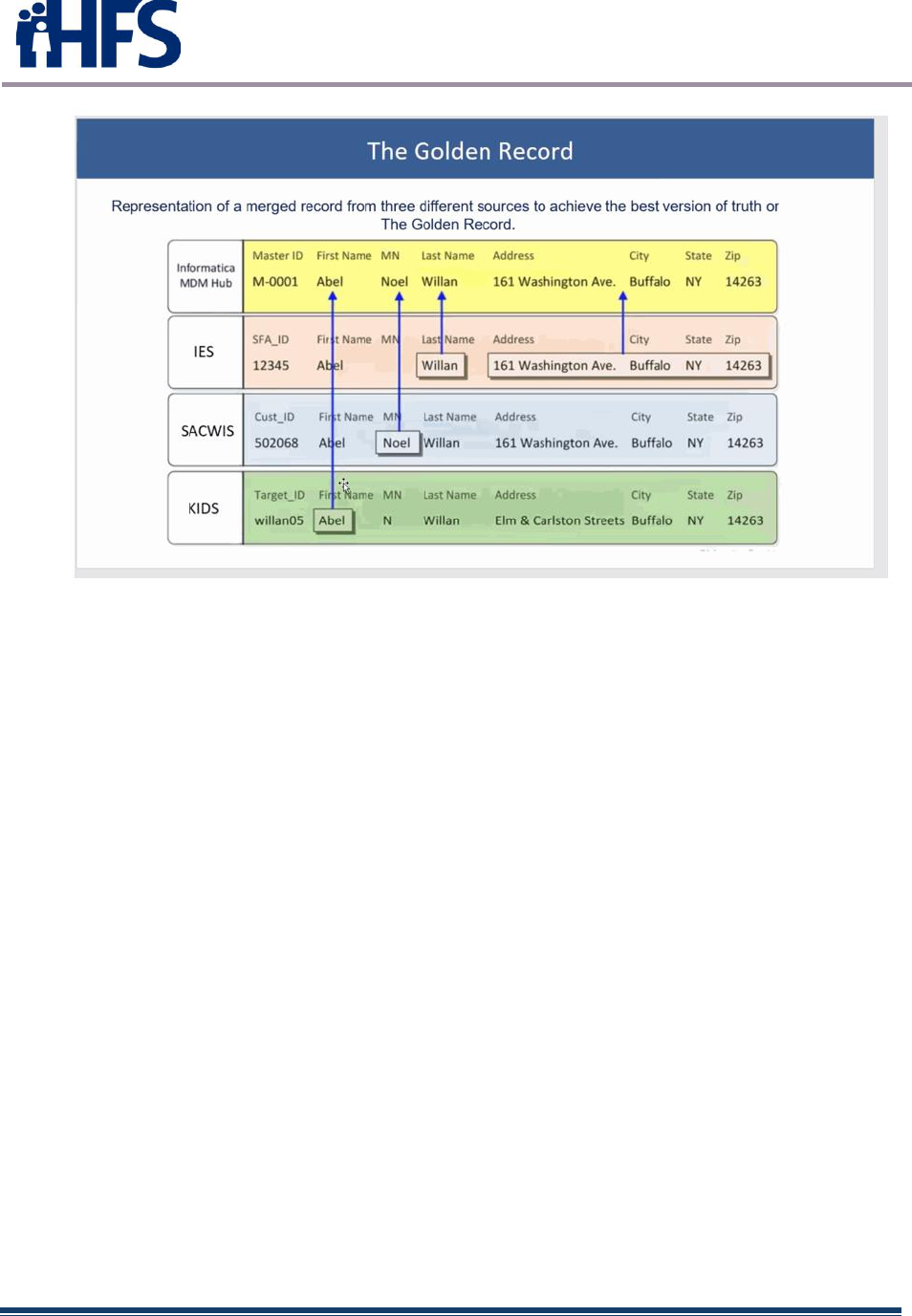
• Informatic MDM, Data Quality, Customer 360, PowerCenter and Address Doctor
tools were installed.
• The ISIP System Security plan was developed. The plan complies with
Minimum Acceptable Risk Standards for Exchanges (MARS-E) to safeguard data
from unauthorized access.
• Data profiling was conducted, and data connections established to ISIP for IES
(DHS data only), eCCPIS (Aging) and SACWIS (DCFS) data warehouse.
• Design and configurations of the MDM Hub, Data Quality and Customer 360
interface established the golden record.
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 25
Figure 12 – Golden Record
2.10.3.3 ISIP – Use Cases and Related Projects
HHSi2’s goal is to improv data quality and interoperability to help agencies improve the
critical services they deliver to those in need. To advance this goal and demonstrate
the business value of ISIP, HHSi2 is collaborating with the Governor’s Of fice and other
state agencies to develop use cases including but not limited to the following:
• Department of Corrections
Reduce recidivism by identifying the services ex-offenders need before being
released from a correctional facility (e.g., Medicaid, SNAP) to ensure they
receive appropriate support (including behavioral treatment) for successful
re-entry.
• Department of Children and Family Services
Provide investigative and hotline staff with more timely information improve
the safety and well-being of children, as well as more comprehensive
information to help ensure investigator safety.
• Department on Aging
Protect high-risk senior adults by providing the Department with more
accurate and complete information to ensure they receive the right services,
including correctional system involvement and veterans’ data to prevent
duplication of benefits.
• Governor’s Office of Early Childhood Development & Illinois Longitudinal Data
System

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 26
Support cross-agency initiatives to match early childhood data across
education and health and human services agencies to better understand the
needs of “low income” and “at risk” children and how to more ef fectively
allocate resources to assist them.
• Department of Juvenile Justice
To support youth who are released from juvenile detention facilities by
ensuring the availability of essential benefits to reduce behavioral and
physical health risks that could lead to recidivism.
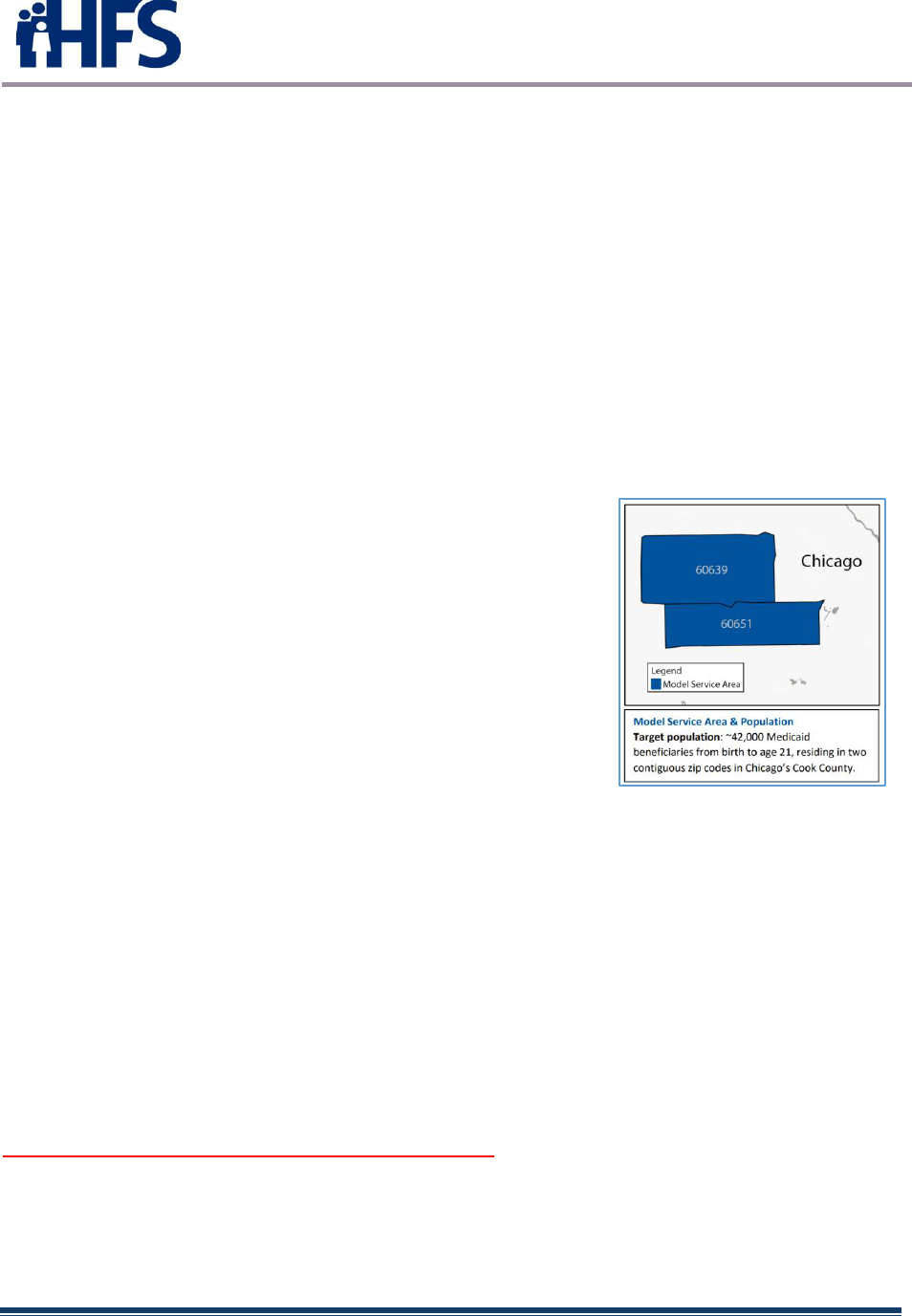
2.10.4 Integrated Care for Kids (InCK)
The Integrated Care for Kids (InCK) Model is a child-centered local service delivery
and state payment model that aims to reduce expenditures and improve the quality of
care for children under 21 years of age covered by Medicaid through prevention, early
identification, and treatment of behavioral and physical health needs. Some programs
also include Children’s Health Insurance Program (CHIP) benef iciaries and pregnant
woman over age 21 who are covered by Medicaid. The model empowers states and
local providers to better address these needs, as well as the impact of opioid addiction
through care integration across all types of healthcare providers.
Almost $126 million in InCK Model funding was awarded to the states and
organizations below for the 7-year Model launched in early 2020. The awards
included two awards to Illinois organizations – Egyptian Public & Mental Health
Department and Lurie Children’s.
2.10.4.1 Egyptian Public & Mental Health Department
Maximum Award Amount Over 7 Years: $15,666,736
Model Goals: Egyptian Health Department, an
integrated local public health department and
behavioral health agency, leads Village InCK. Village
InCK Health Department will use an integrated services
team called “i-Hub” as a central access point f or care
coordination. Village InCK is also designed to reduce
costs for emergency department visits, 80 percent of
the Medicaid population. In order to achieve this goal,
Egyptian inpatient psychiatric care, and residential
inpatient psychiatric care and residential substance use
disorder (SUD) services.
Figure 13 - Egyptian
Egyptian Health Department seeks to reduce expenditures through education, mobile
crisis response services, and increased engagement in SUD prevention, treatment, and
recovery services, respectively. Village InCK will serve children and adolescents in
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 27
five contiguous rural counties that have higher rates of poverty than state and national
averages.
Highlights: Egyptian Health Department estimates that approximately 500-700 of its
7,900 Village InCK attributed children will have higher levels of need and will require
services commensurate with their higher levels of need. Key services for the subset of
individuals requiring higher levels of need include mobile crisis response, wellness
coaches (for those with medically complex or chronic health conditions), medical
telehealth specialty services, integrated case management with mobile crisis response,
peer support, respite, in-home community support team services follow up, and a
family support program.
2.10.4.2 Ann & Robert H. Lurie Children’s Hospital of Chicago
Maximum Award Amount Over 7 Years: $16,000,000
Model Goals: All Hands Health Network (AHHN) is led
by Lurie Children’s, a major pediatric hospital with
extensive community partnerships throughout Chicago.
Lurie Children’s aims to expand access to quality
primary care, specialty care, and behavioral health
services while building care coordination and service
integration capacity. AHHN is designed to adapt and
synthesize existing resources where possible, improve
care coordination for those served by Medicaid
managed care organizations (MCOs), and build on
existing Medicaid initiatives, namely the new Integrated
Health Home state plan amendment.
Figure 14 - Lurie Children’s H ospital
Highlights: Service Integration Coordinators (SICs) will work directly with families and
children to facilitate assessment screenings, identif y children’s needs, and connect
them to the appropriate services. Lurie Children’s will assign SICs to providers based
on geography. SICs are expected to spend the majority of their time in schools and
health centers. AHHN will support integrated coordination between SICs and MCOs as
well as the expansion of Lurie Children’s collaborative model of care inf using
behavioral health support across community partners. AHHN will also support training
and referral assistance for primary care providers, expand the trauma-informed
Parenting Support program, and extend telehealth capabilities.
2.10.5 Electronic Visit Verification (EVV)
Section 12006(a) of the 21st Century Cures Act mandates that states implement EVV
for all Medicaid personal care services (PCS) and home health services (HHCS) that
require an in-home visit by a provider. This applies to PCS provided under sections
1905(a)(24), 1915(c), 1915(i), 1915(j), 1915(k), and Section 1115; and HHCS
provided under 1905(a)(7) of the Social Security Act or a waiver.
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 28
The current requirement mandated a compliance date of January 1, 2020, for all
personal care services, and January 1, 2023, for all home health services. However,
HFS requested and received a one-year federal extension of the January 1, 2020,
implementation date. The Department currently estimates implementations for all
personal care services in 2022.
The federal requirements describe certain data points that must be collected
electronically, but each state creates their own EVV system. Illinois will determine
how we will gather, and report data used within EVV.
The purpose of implementing EVV is to support Illinois’ goal to improve Medicaid
program integrity, safeguard against fraud and abuse, improve program oversight,
and comply with new federal requirements.
Services impacted under EVV include:
• Personal Care Services (PCS): Individuals receiving personal support in the home
throug h Illinois’ Home and Co mmunity Based Services waiv ers, inc lud ing:
o Persons with Disabilities waiver
o Persons with Traumatic Brain Injury waiver
o Persons with HIV/AIDS waiver
o Persons who are Elderly Waiver
o Adults with Developmental Disabilities Waiver
o Children and Young Adults with Developmental Disabilities Support Waiver
o Children and Young Adults with Developmental Disabilities Residential Waiver
• Home Health Care Services (HHCS): Individuals receiving home health services
through the Medicaid State Plan
Providers subject to the first round of EVV include: personal assistants, personal
support workers and homemakers.
Data points EVV must capture:
• Type of service performed
• Individual receiving the service
• Date of the service
• Location of service delivery
• Individual providing the service
• Time the service begins and ends
Illinois is in the final stages of procuring a vendor who will implement, train and provide
technical support for an EVV system for the Illinois Medical Assistance Programs. The
main goal is to improve Medicaid program integrity by achieving the following objectives:
• Reduce overpayments and claim errors.
• Saf eguard against waste, fraud, abuse, inefficiency, and duplication.
• Improve oversight of provider perf ormance, benef iciary access, care coordination and
transitions, and program expenditures and utilization.
• Develop a system that will accommodate and overcome limited internet access in rural
areas.
• Ensure compliance with approved service plans and prior authorizations .
• Monitor the receipt, timeliness, and completeness of authorized Medicaid home-based
services.
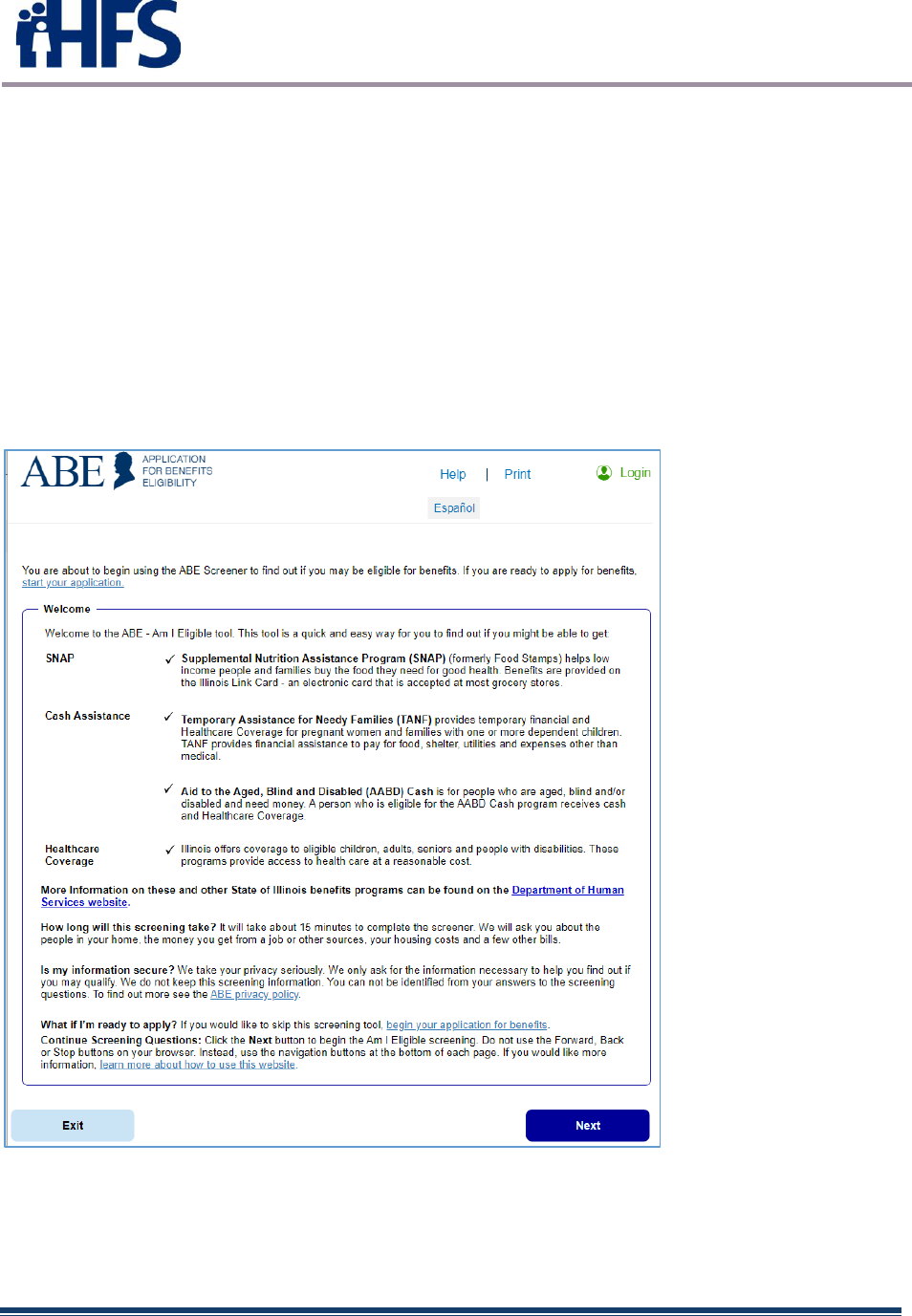
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 29
2.10.6 Integrated Eligibility System (IES)
The Integrated Eligibility System (IES) determines Eligibility for the Illinois Department
of Healthcare and Family Services Medical Programs and the Illinois Department of
Human Services SNAP, income, and other public assistance programs. IES consists of
two main applications: the Application for Benefits Eligibility Portal (ABE Portal) and the
Worker Portal. The ABE Portal is a public facing online application for benefits and a
client case management system. The Worker Portal is a caseworker Intake and Service
Coordination System that uses a Corticon Rules Engine to determine eligibility. The
current system provider is Deloitte Consulting LLP (“Deloitte”) and the provider contract
is held and managed by the Illinois Department of Healthcare and Family Services (HFS).
The Deloitte contract is expected to end in October 2022.
Application for Benefits Eligibility (ABE) Screener
Figure 15 – ABE screener
HFS administers the State’s medical programs including Medicaid, Comprehensive
Health Insurance Program (CHIP), and State health benefit programs while the Illinois
Department of Human Services (DHS) administers TANF and SNAP programs. The
Illinois Department of Innovation and Technology (DoIT) is responsible for all aspects of

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 30
the State’s technology f or Executive Branch agencies. DoIT currently houses and
maintains the infrastructure environment for IES.
Teams of employees from DoIT, HFS, DHS, and the system provider are involved in
activities to improve the infrastructure, application, and related databases with focus on
two primary goals: 1) SNAP application and redetermination timeliness objective of 90%,
and 2) timely processing of medical applications and renewals. This requires both
infrastructure upgrades as well as correction of application defects and new
enhancements.
An IES Steering Committee (Committee) exists to provide strategic-level direction and
set priorities for IES program activities. Members of the Committee include the Secretary
of DoIT, Secretary of DHS and Director of HFS and senior executives from each of those
agencies.
In October of 2013 Phase I of the IES was implemented. This implementation consisted
of the ABE online application for benefits and the functional areas of the Worker Portal
needed for Intake disposition of those online applications. These dispositions, client
demographics, and client case information were integrated into the remaining legacy
system. The legacy system remained the system of record, and at the time all issuance,
redeterminations, case coordination, and interfaces resided within the legacy system. In
October of 2017 Phase II of the IES System was implemented and IES became the
system of record for Medical, SNAP and income assistance programs. This
implementation consisted of several additional modules for ABE, including the Provider
Portal and the Manage My Case portal. All Medical, SNAP, and Cash dispositions,
issuances, redeterminations, case coordination, overpayment and supplemental SNAP
modules, realtime verification interfaces, Batch interfaces, online and batch forms were
implemented in the worker portal. Additionally, several modules were added to the
Worker Portal such as Appeals and the TANF Work Verification system.
The State has recently issued a Request for Proposal which seeks professional services
to establish a Program Management Office (PMO) that assists the State’s executive
leadership in managing and overseeing its efforts to meet pandemic -related
programmatic changes and increasing system demands to the Illinois Integrated
Eligibility System (IES).
The DoIT RFP attempts to secure a PMO as an emergency procurement under the
Gubernatorial Disaster Proclamation due to the spread of the Coronavirus Disease
(COVID 19). Due to COVID 19, there have been multiple pandemic-related programmatic
changes and increasing system demands upon IES. The State requires a vendor that
can quickly establish a program management team, develop and execute a plan to
effectively and efficiently complete priority requirements, and maintain IES operational
demands including technical refresh of IES. The State will evaluate the proposals
received and select one vendor to provide a PMO for a period not to exceed two years,
which includes a transition to a longer-term PMO established through a separate
competitive solicitation.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 31
2.10.7 Illinois Medicaid Program Advanced Cloud Technology (IMPACT)
The IMPACT initiative is a multi-agency ef f ort that modernizes the Department’s 40+
year-old MMIS which was built to support a fee-for-service Medicaid program. The MMIS
supports claims processing for the HFS medical assistance programs.
HFS currently manages and operates the MMIS to support claims processing for the
Illinois Medicaid Enterprise. The MMIS environment includes the database subsystems
(e.g., Provider, Recipient, Reference and Prior Approval); the Hospital, Pharmacy and
NIPS claims processing subsystems; the Management and Reporting System (MARS);
the Enterprise Data Warehouse; the Pharmacy point of sale system and the web-based
applications provided in the Medical Electronic Data Interchange(MEDI) system.
The current MMIS was fully implemented in 1982 and was primarily built to support a
fee-for-service Medicaid program. Rather than developing a new system, Illinois is
developing a cloud based MMIS called IMPACT.
IMPACT Phase 1 - eMIPP
The first phase of IMPACT included the launch of the Electronic Health Records
Medicaid Incentive Payment Program (eMIPP), which provides incentive payments to
eligible professionals, eligible hospitals and critical access hospitals to adopt,
implement, upgrade or demonstrate meaningful use of certified electronic healt h
records (EHR) technology.
The eMIPP program accepted attestations and paid incentive payments through
2021. The program continues through September 30, 2023, primarily to complete
auditing requirements.
IMPACT Phase 2 – Provider Enrollment
Beginning in July 2015, providers seeking to serve Medicaid clients have enrolled and
revalidated through the new IMPACT web portal. Paper enrollment applications or
updates are no longer being accepted, and email has become the primary method for
provider communication.
Existing Medicaid providers enrolled in the current legacy MMIS w ere required to
revalidate their information in the new IMPACT system during a 6-month revalidation
period between August 2015 and January 2016. Subsequently, providers who deliver
services through Medicaid waiver programs —including providers who have previously
not been required to enroll in MMIS— were required to enroll in IMPACT beginning in
2016.
IMPACT future: PBMS and Full Implementation
In 2017, IMPACT launched a new Pharmacy Benefits Management System
(PBMS). More information about the PBMS can be found at ILLINOIS Rx Portal.
On March 30, 2021, HFS signed a 4-year contract with CNSI to replace core elements
of its legacy MMIS with a more modern MMIS. The contract requirements include:
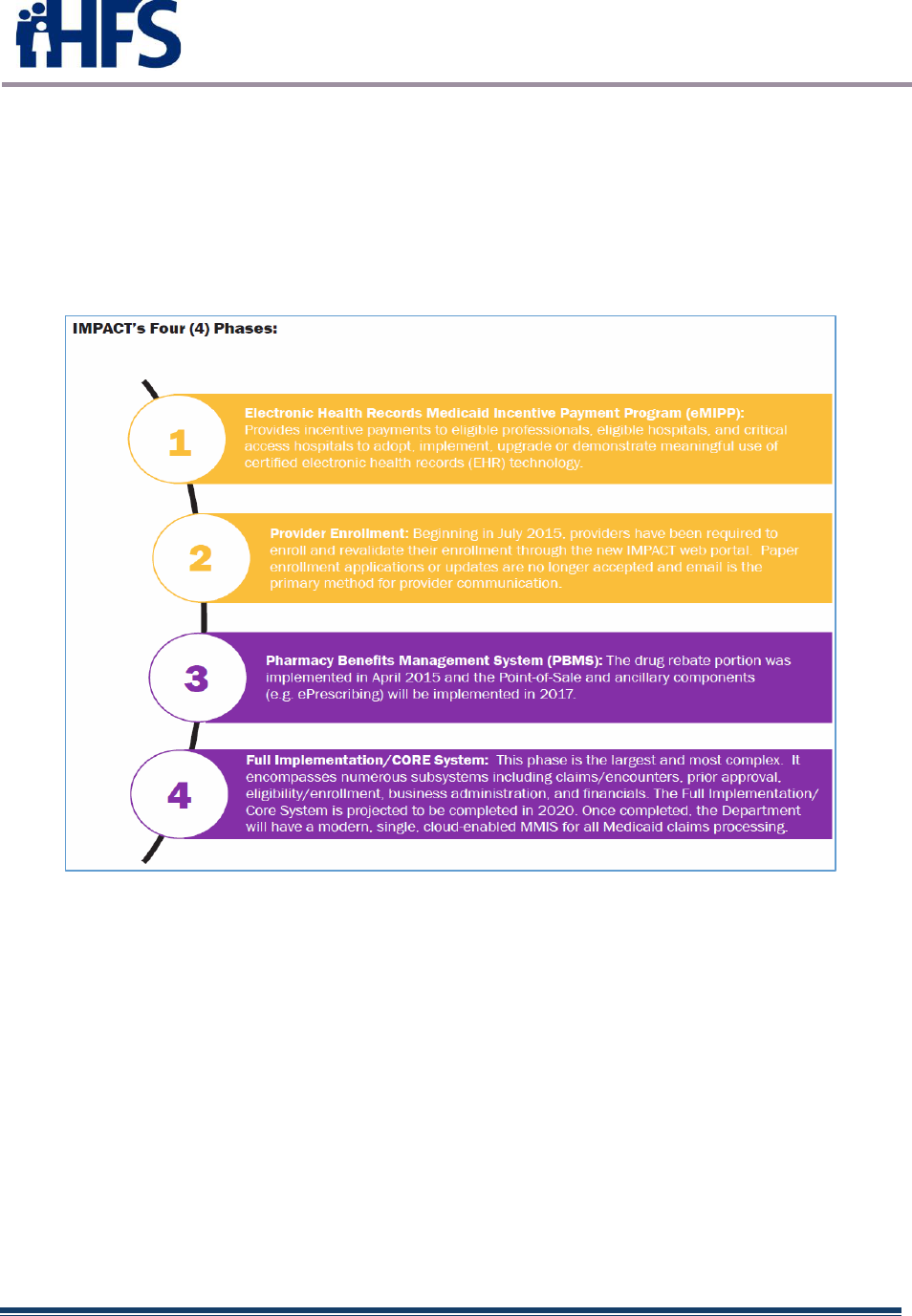
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 32
• The “Core: must be c ap able o f ret aining elig ibility inf ormation o f ind ividuals covered b y
the several healthcare plans of the Department and adjudicating claims f or services
provided under those health care plans.
• The “Core” must sup p ort Manag ed Care p ro g rams f or memb ers, co st avo idance, and
other demands f or payment, payment reconciliation, and mandatory reportin g.
• IMPACT Core must be designed and implemented in a manner that ensures it will
successfully complete Health and Human Services (HHS)/Centers f or Medicare and
Medicaid Services (CMS) certification.
FIGURE 1 6 – Impact Phases
2.10.8 HealthChoice Illinois ADT
2.10.8.1 HealthChoice Illinois ADT design and development
In May of 2019, Illinois engaged a consulting firm (Health Management Associates) to help restart
the ADT (Admit-Discharge-Transfer) services project and update the project plans to implement
a state-wide ADT system that would support and align with the Medicaid program’s priorities for
care coordination. Implementation of the ADT system began in April 2021, with onboarding
beginning in late spring of 2021.
HFS selected Collective Medical Technologies (CMT), A PointClickCare Company, through
competitive bid, to implement the Illinois ADT platform. CMT has the largest care post-acute
network coverage with 70% market share across 22,000+ skilled nursing and long-term care
facilities, and 3,000+ hospitals across the country.
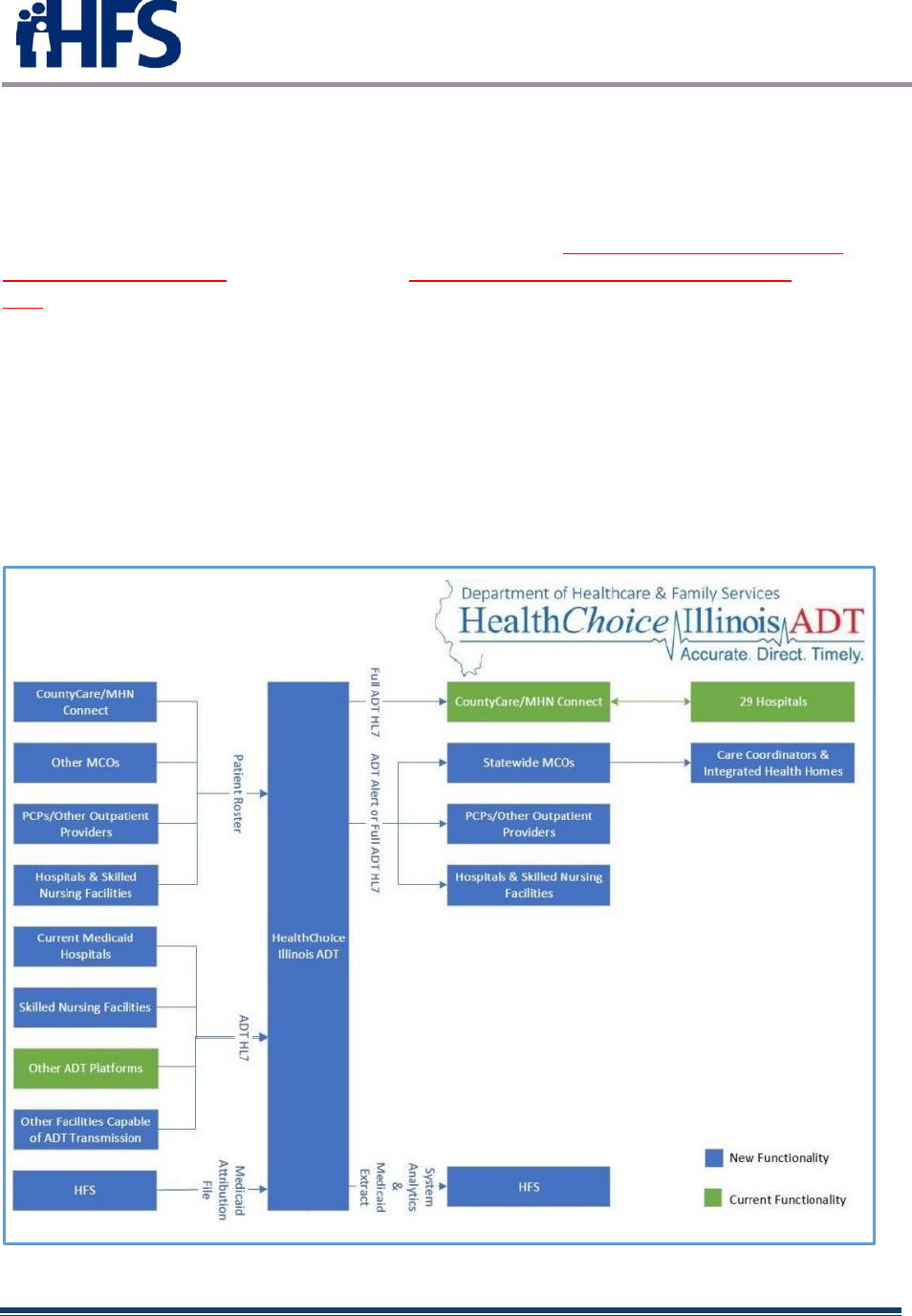
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 33
HFS and CMT’s statewide technology platform will facilitate the real-time transmission of HL7
formatted messages from hospitals, skilled nursing facilities and other institutions and notify
community providers of patient admissions, discharges and transfers to improve care
coordination and quality.
The functionality of this technology platform supports Illinois’ 2021-24 Comprehensive Medical
Programs Quality Strategy and aligns with the CMS Interoperability and Patient Access Final
Rule requirements that hospitals send electronic notifications of admissions, discharges and
transfers to a patient’s care team.
2.10.8.2 HealthChoice Illinois ADT implementation
All hospitals and EHR-capable skilled nursing facilities that are enrolled in the IMPACT system
to serve Medicaid participants are required to transmit electronic notifications of admissions,
discharges, and transfers for Medicaid participants in an HL7 format to the HFS technology
platform. MCOs, hospitals, and other providers may subscribe to the ADT notification service
to receive real-time data for their Medicaid members/patients.
Figure 17 – HealthChoiceIllinois ADT
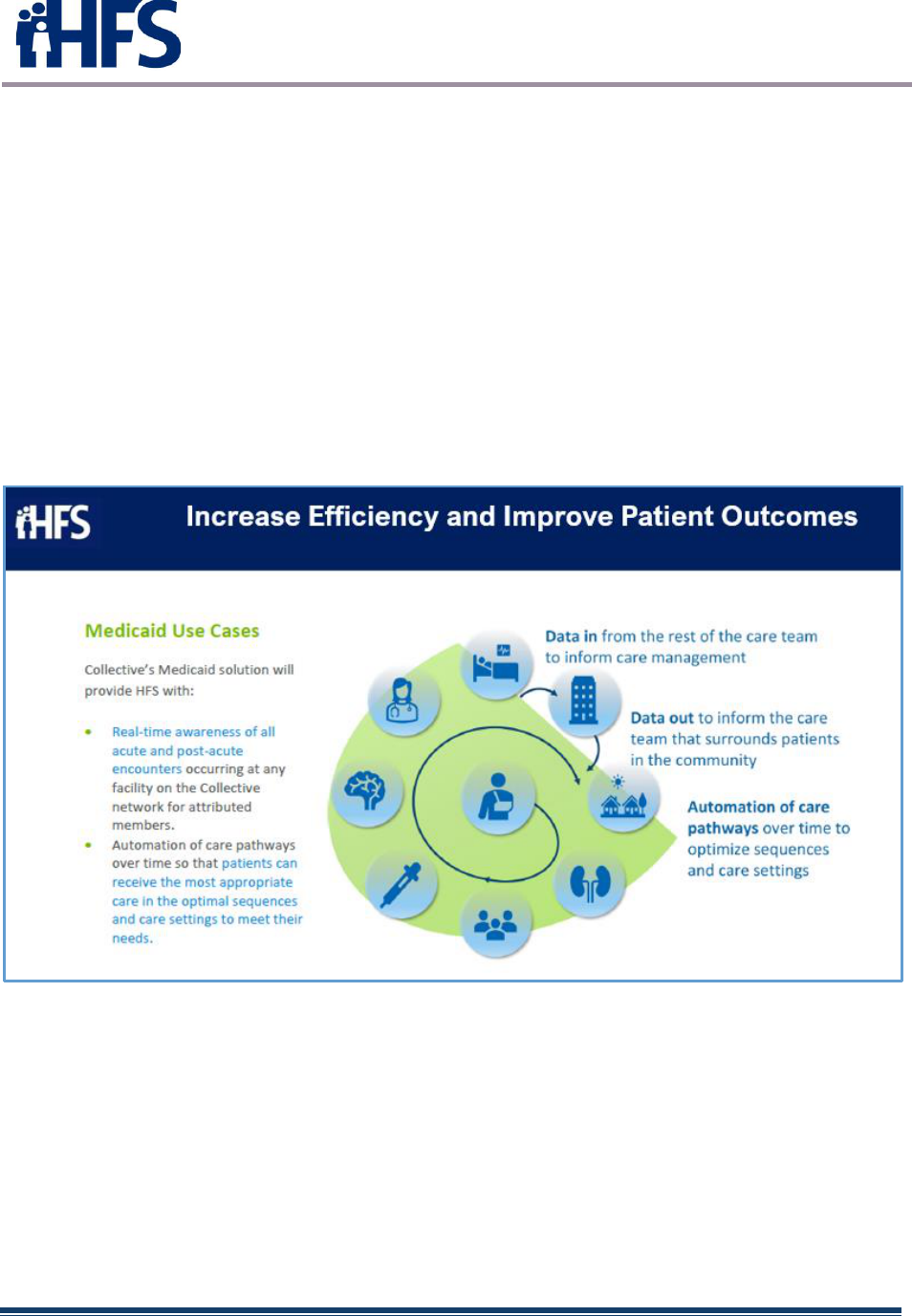
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 34
Since the HealthChoice Illinois ADT system became operational in the spring of 2021, 182
hospitals, 463 Skilled Nursing Facilities, 6 MCOs, 13 Specialized Mental Health
Rehabilitation Facilities (SMHRF), 10 Intermediate Care Facility/Developmental
Disabilities (ICFDD) and 22 Supportive Living Facilities have been onboarded and are
contributing HL7 ADT notification data.
2.10.8.3 Comprehensive Medical Programs Quality Strategy
In addition, Illinois’ Comprehensive Medical Programs Quality Strategy includes goals for
improving care coordination, using evidence-based interventions to reduce health disparities,
deploying technology, and increasing data integration. The ADT system directly supports
those critical quality goals and leverages best practices for sharing timely information to
enable effective care coordination.
Figure 18 – Improve Patient Outcomes
2.10.8.4 HealthChoice Illinois ADT future
When the majority of onboarding providers is complete, HFS will be able to start analyzing the
HL7/ADT data. HFS foresees numerous possibilities to assist/improve Agency program.
Some of these possibilities include:
• Third Party Liability – Provider encounter insurance information.
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 35
• Williams & Colbert - Assist legislation regarding member eligibility for community-based
services by tracking discharge dispositions information and discovering when patients
leave without the recommendation of the attending physician.
• Claims Information – Match encounter events with claims information in EDW.
• Diagnosis Data Trends – Assess diagnosis data trends (drug-related morbidity for
opioid and heroin use; gastro-intestinal illness, specific admissions related to COVID-19
or other diseases); see regional trends showing health disparities and health equity.
• Incentive Programs – HFS could create incentive programs for providers who meets
certain data metrics. HL7 notifications could be used to verify the providers are meeting
the required thresholds.
• The Gravity Project - The Gravity Project seeks to identify data elements and
associated value sets to represent SDOH information documented in electronic health
records (EHRs) across four clinical activities: screening, diagnosis, goal setting, and
intervention activities.
• Crisis Line Hotline - All HFS-contracted Managed Care Organizations (MCOs) and
Managed Care Community Networks (MCCNs) with contracts serving children utilize the
CARES line for the purposes of centralized intake and localized dispatch for children in
mental health crisis.
• Sepsis Project – In current CMT Sepsis project implementations, for every facility using
CMT’s event notification and care collaboration platform – which includes emergency
departments, ambulatory practices, skilled nursing facilities, behavioral health clinics and
approximately 1,000 hospitals – at no charge, CMT is rolling out notification functionality
that identifies patients with a history of sepsis so that care teams may more quickly
intervene to address these patients’ unique needs.
• Opioid and Substance Use Disorder Support & Prescription Drug Monitoring –
Connect patient utilization and prescription histories across care settings to flag patients
at risk for substance use disorder and collaborate with providers and other resources on
the path to recovery.
• Value-based Care Optimization - Improve transitions of care and reduce readmissions
by identifying at-risk patients and collaborating in real-time with hospitals, skilled nursing
facilities, home health and other post-acute providers to support and track these patients'
post-discharge.
• Behavioral Health Integration – Achieve better patient outcomes for those struggling
with mental or behavioral health concerns with groundbreaking consent functionality for
real-time communication between providers across the healthcare spectrum.
• Workplace Violence Prevention - Take control of workplace safety by receiving
immediate notifications whenever a patient with a history of or risk for violence—
including physical assault, verbal threats, theft, sexual assault, and self-harm—presents.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 36
• ED Optimization – Increase efficiency and improve patient outcomes by minimizing
unnecessary ED utilization, streamlining care, and increasing cost savings with access
to patient histories and care guidelines integrated directly into existing workflows.
Additional HL7 data HFS may incorporate in the future includes:
• Continuity of Care Document (CCD) – The CCD is an HL7 XML standard adopted for
the exchange of electronic clinical records.
• Labs & Imaging – HL7 Observation Result (ORU) messages contain information about
a patient’s clinical observations and is used in response to an order generated in a
clinical system (HL7 Order Entry (ORM) message). ORU messages are most commonly
used for EKG student, lab results, imaging studies and medical interpretations.
• Rx RDE – An HL7 Pharmacy/Treatment Encoded Order (RDE) message is used to send
orders to a pharmacy or medication dispensing system.
• Scheduling - HL7 Scheduling Information Unsolicited (SIU) messages are used to
exchange patient appointment schedule information between clinical and administrative
systems.
• Other – Many other HL7 notification possibilities exist, including those messages
assisting with “physician notes” and billing data.
2.11 State Laws or Regulations
2.11.1 Healthcare Transformation Collaboratives
On March 8, 2021, HFS announced the Healthcare Transformation Collaboratives
program. As outlined in Public Act 101-650 and SB 1510 , the program is designed to
improve healthcare outcomes, reduce healthcare disparities, and realign resources in
distressed communities throughout Illinois. In particular, the program seeks to increase
access to community-based services, preventive care, obstetric care, chronic disease
management, and specialty care in these communities.
With support from federal matching funds, Illinois will invest $150 million into
collaboratives that fill healthcare gaps and focus on underlying health conditions in areas
high on the federal Centers for Disease Control and Prevention's social vulnerability
index scale, communities that have been disproportionately affected by the COVID-19
pandemic and areas served by critical access and safety net hospitals, including rural
parts of the state.
2.12 Interstate HIT/HIE Activities
The HealthChoice Illinois ADT system allows ADT notifications to be shared with other
States where appropriate. The HealthChoice Illinois ADT system will immediately
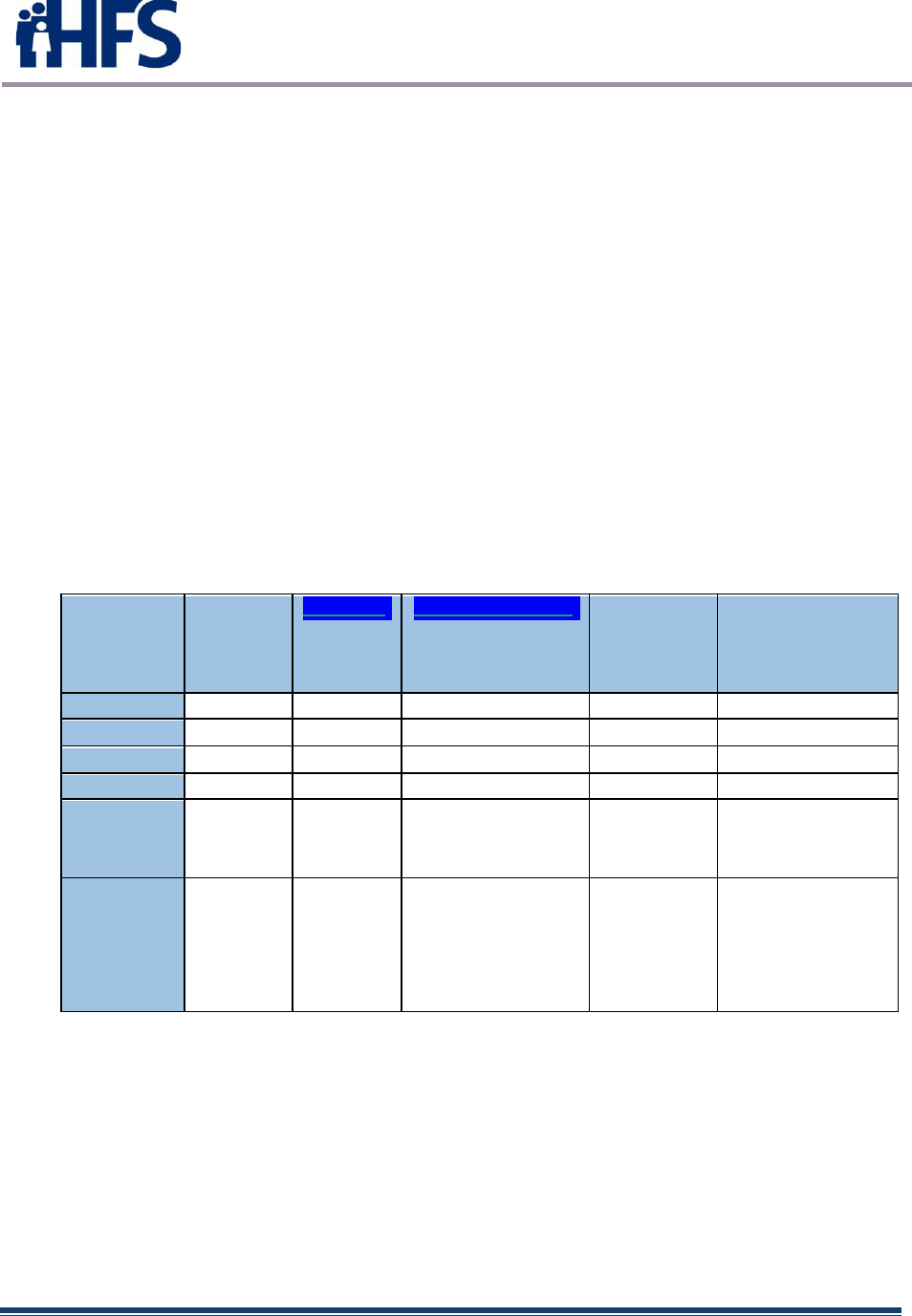
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 37
incorporate Medicaid patients’ ADT notifications f or patients presenting at out -of-state
locations in the CMT network. This connectivity allows for real-time care coordination to
occur across state lines. Future HL7 notifications may involve more advanced file types,
such as those related to labs, prescriptions and imaging.
The Illinois Prescription Monitoring Program (PMP) also allows for interstate
connectivity, as reviews of patient precriptions includes data from other states due to
connections between PMP systems.
The PMP is working with the surrounding states to establish the process for compliance
with section 1944(f)(2) of the Social Security Act. Missouri currently does not have a
state-wide PMP; however, IL PMP is integrating with providers in the St. Louis County
area and providing as much data to the users as possible. Kentucky and Illinois have
been piloting the RxCheck system which breaks down the data barriers of interstate data
sharing. Wisconsin is requiring certain fields within the query from Illinois. Illinois
providers are being educated as to these required fields necessary to send in the
request, for example, DEA number of the requesting provider must accompany the query
request.
ILLINOIS CONNECTIVY TO CONTIGUOUS STATES
Contiguous
State
Exchange
PMP data
with IL?
RxCheck?
PMPInterconnect?
Other
Method or
Contract
information
Comments
Indiana
Y
Y
Iowa
Y
In Prog
Y
Kentucky
Y
Y
Y
Michigan
Y
Y
Missouri
Y
St. Louis county only
St. Louis
county is
connected
Missouri PMP not yet
operational
Wisconsin
Y
In Prog
Y
Some restrictions on
RxCheck queries. WI
connected to
RxCheck. IL not
sharing data with them
(via RxCheck) yet.
Figure 19
2.13 Public Health Interoperability Status
To complete the Promoting Interoperability Program Public Health objective during
attestation, providers had several options. The options below were available via the DPH.
The Illinois Prescription Monitoring Program (PMP) is hosted by DHS as an agent of
DPH. The Stage 3 options continue to be available to the Medicare Promoting
Interoperability Program (for Eligible Hospitals).

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 38
Immunization Reporting
• I-CARE currently accepts immunization data from providers in HL7 2.3.1 and 2.5.1
• Testing and ongoing submission of data from EPs, EHs and CAHs for Meaningful Use is
underway
• Immunization Reporting: I-CARE will accept Stage 3 MU standards on/after January 1,
2017 (Bi-directional exchange QBP/RSP and capacity to receive NDC Codes using HL7
2.5.1 r1.5 plus Addendum)
Electronic Laboratory Reporting (ELR)
• I-NEDSS currently accepts ELR data from hospital laboratories in HL7 2.5.1
• Testing and ongoing submission of data from EHs and CAHs for Meaningful Use is
underway
Syndromic Surveillance Reporting (updated 6/30/17)
• IDPH currently accepts syndromic surveillance data from Eligible Hospitals
• Stage 2 included Emergency department data only in HL7 2.5.1
• Stage 3 includes Emergency department, inpatient and urgent care type visits
• Illinois will accept syndromic surveillance data from EPs in an urgent care setting only
• IDPH Syndromic Surveillance Data Element List
Electronic Case Reporting (eCR) (updated 6/30/17). For Stage 3 reporting only, beginning
1/1/2018
• IDPH will accept HL7 standard, electronic Initial Case Reports (eICR) from Eligible
Hospitals and Eligible Providers (prioritized format:
http://www.hl7.org/implement/standards/product_brief.cfm?product_id=408)/
HL7 membership login may be required.
• IDPH will accept certified electronic case reports that follow the 2015 edition test
methods. (https://www.healthit.gov/policy-researchers-implementers/2015-edition-te...)
• To register intent, a provider MUST HAVE certified eCR capabilities at the time of their
registration.
• To register intent to submit eCR data to IDPH, please click here:
https://redcap.dph.illinois.gov/surveys/?s=KR7KEHCLT9
Specialized Registry Reporting – Stage 2 only
• Illinois Prescription Monitoring Program
Cancer Reporting
• The Illinois State Cancer Registry currently accepts cancer case information from
providers using the HL7 CDA, Release 2
• Testing and ongoing submission of data from EPs for Meaningful Use is underway
• Stage 2 – as specialized registry.
• Stage 3 - as public health registry

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 39
3 HFS TO BE LANDSCAPE
3.1 HIT Goals and Objectives
3.1.1 HIE and Public Health Goals
At the end of the 2016 program year, new providers could no longer enroll in the EHR
Incentive Program. After the 2021 program year, providers could no longer attest for the
Medicaid Promoting Interoperability Program. Illinois’ 2021 Environmental scan
reported several interesting facts, detailed below:
3.1.1.1 Environmental Scan Highlights
• Over 75% of respondents indicated that the Medicaid PI program encouraged or
supported their adoption of CEHRT. And nearly 72% of respondents said the
incentive payments were worth the effort for the adoption, implementation, or
upgrade of EHR technology.
The top four ways adoption of a CHERT has improved practices is:
o Decrease in medication errors 64%
o Improved patient throughput 60%
o Improved efficiency in reporting 60%
o Improved referral process 57%
• Those participating in the Medicaid PI program are more likely to share
information electronically, 74% of all 2021 respondents compared to 83% of
those in the Medicaid PI program.
• In 2011, 61% of Illinois providers had an EHR in place, compared to 100% of
practices surveyed in 2021.
• An increasing number of providers indicate having a process in place to receive
ADT notifications, 55% in 2016 compared to 70% in 2021. 89% of respondents
indicate these notifications come directly from the hospital with 90% of those
notifications coming via Fax.
• Organizations participating in a HIE increased from 32% (2016) to 51% (2021).
Of those participating in a HIE, 36% used Care Everywhere and 36% were using
an EHR option.
• The three biggest challenges for hospitals to getting external data is:
o Conflicting information from different doctors
o Different state rules/regulations
o Too much data from other doctors

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 40
• Half of respondents currently receive ADT notifications. Of those that do not
currently receive ADT notifications, 15% are unable to receive them and 85%
say hospitals do not send electronic notification despite 77% of hospitals
reporting they have a process to send them.
The 2021 Environmental scan is provided in Appendix A below. There are many more
similar assessments included in the environmental scan.
3.1.1.2 HealthChoice Illinois ADT
Beginning in 2021, Illinois implemented the HealthChoice Illinois ADT program. An RFP
was awarded to Collective Medical Technologies (CMT) on November 24, 2020. The
contract between HFS and CMT was signed February 25, 2021. The vendor was charged
with securing a software as a service (SaaS) state-wide Admission, Discharge and
Transf er (ADT) Notification System (“System”) . All Illinois hospitals and EHR system-
capable Long-Term Care (LTC) facilities connect and contribute Medicaid ADT
notifications to this centralized system, named the HealthChoice Illinois ADT system.
Real-time Medicaid ADT notifications are delivered to System subscribers at appropriate
hospitals, LTCs, and Illinois Medicaid Managed Care Organizations (“MCOs”). Among
other quality improvements and cost savings strategies, the ability to send and receive
ADT notifications will assist the community of care givers to improve care transitions,
leading to a reduction in unnecessary hospital and Emergency Department/Emergency
Room admissions and readmissions.
Following the ADT notification implementation, HFS will focus on developing capabilities
such as sharing notifications across state borders, ensuring advanced file types may be
shared, and ensuring data sharing f or Illinois citizens with or without Medicaid insurance
occurs.
3.1.1.3 Attestations and Payments
Payment statistics for Illinois providers participating in the Medicare and Medicaid EHR
Incentive programs are shown in the tables below. Yearly attestation totals for the Illinois
Medicaid EHR Incentive Program increased on average of approximately 20% for the
years 2012-2015. For 2016, a significant increase was realized in the number of EP AIU
attestations (last program year to attest for year 1) and a slight increase experienced in
the number of EP MU attestations. After 2016, since new providers could no longer begin
their attestations, the numbers started to drop for EPs. Eligible Hospitals had completed
their attestations by 2017.
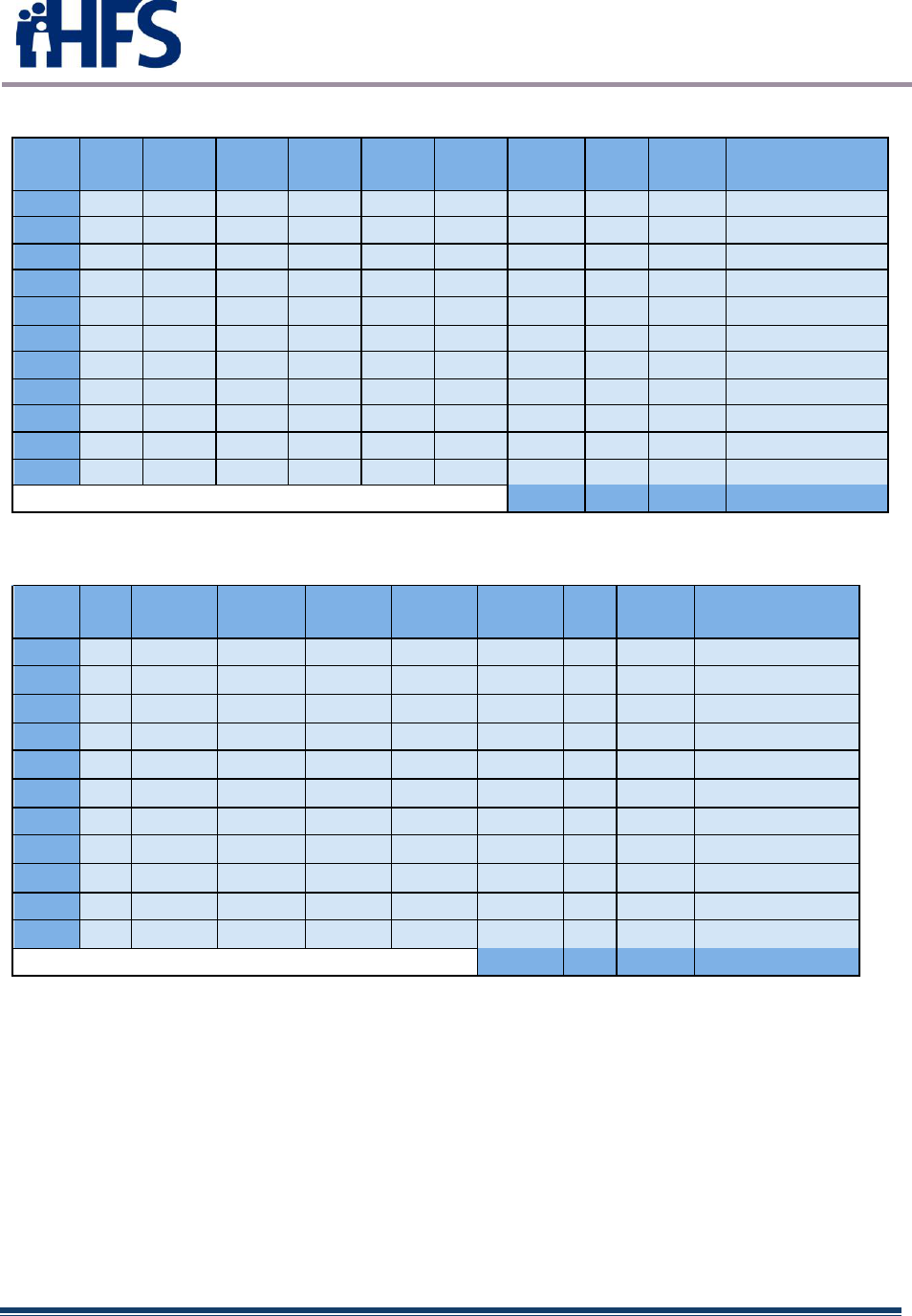
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 41
Eligible Professionals
YEAR
AIU
MUYR1
MUYR2
MUYR3
MUYR4
MUYR5
MUYR6
MU
TOTAL
Payment
Amount
2011
2156
0
0
0
0
0
0
0
2156
$45,411,269.00
2012
1678
34
554
0
0
0
0
588
2266
$40,654,098.41
2013
1429
46
1475
451
0
0
0
1972
3401
$47,462,602.00
2014
1034
178
967
1129
288
0
0
2562
3596
$45,832,016.00
2015
994
183
1084
852
868
196
0
3183
4177
$50,220,858.00
2016
1270
163
813
800
708
737
170
3391
4661
$57,220,858.00
2017
0
0
739
604
639
506
545
3033
3033
$25,746,154.00
2018
0
0
172
624
533
559
452
2340
2340
$19,855,811.00
2019
0
0
103
84
274
194
223
878
878
$7,457,324.00
2020
0
0
75
101
122
237
162
697
697
$5,913,168.00
2021
0
0
17
70
103
120
205
515
515
$4,366,168.00
Figure 20
TOTAL
27720
350,140,326.41
Eligible Hospitals
YEAR
AIU
MUYR1
MUYR2
MUYR3
MUYR4
MUYR5
MU
TOTAL
Payment
Amount
2011
58
34
0
0
0
0
34
92
$91,409,021.00
2012
35
22
67
0
0
0
89
124
$97,558,896.30
2013
12
10
78
65
0
0
153
165
$89,429,620.88
2014
3
0
23
77
14
114
117
$29,659,809.59
2015
0
0
5
21
16
0
42
42
$5,879,666.50
2016
0
0
2
6
3
1
12
12
$937,143.00
2017
0
0
0
2
0
0
2
2
$50,365.00
2018
0
0
0
0
0
0
0
0
$0.00
2019
0
0
0
0
0
0
0
0
$0.00
2020
0
0
0
0
0
0
0
0
$0.00
2021
0
0
0
0
0
0
0
0
$0.00
Figure 21
TOTAL
554
$314,924,522.27

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 42
3.2 SMA IT System Architecture
In 2013, it was announced that Illinois would join Michigan in employing a shared MMIS
platform. The first phase of the project, Electronic Medicaid Incentive Payment Program
(eMIPP) went live for Illinois in November 2013. In July of 2015, the Provider Enrollment
(PE) phase of the project was implemented.
HFS currently manages and operates the Illinois legacy MMIS. The Illinois legacy MMIS
meets all certification requirements as set forth by CMS in the State Medicaid Manual,
Part 11 – Medicaid Management Information System. The MMIS was fully implemented
in 1982 and was primarily built to support a fee-for-service Medicaid Program. Through
the years, HFS has made many enhancements and modifications to the current MMIS.
However, it is an older legacy system that has become increasingly difficult to maintain
and modify. HFS, therefore, embarked on a structured planning project to identify needed
functionality and explore the best alternatives to acquire and operate a new MMIS.
In March 2012, Illinois was approached by the State of Michigan to discuss the “state
sharing” option f or the new MMIS. It was determined Illinois and Michigan would benefit
financially in the Operations and Maintenance Phase (post implementation) such that
costs normally borne by the State (25%) would be shared with Michigan, and both states
would share in enhancement efforts and costs. In addition, subsequent design,
development and implementation (DDI) efforts to maintain compliance with future federal
regulations would also be shared between both states. Michigan would extend its MMIS
to accommodate Illinois’ claim volumes.
The State of Michigan undertook the replacement of its MMIS in 2005. The system was
put into production use in 2009 and was certified by CMS in 2011 with no def ects. The
system is MITA and HIPAA compliant and meets the Seven Conditions and Standards
set forth by CMS. Michigan has started the ICD-10 compliance project and expects to
complete that effort according to the federally mandated deadlines. The system is
scalable and can be extended to accommodate Illinois’ Medicaid claim volumes and
business practices without diminishing the State of Michigan’s Medicaid program
objectives.
The State of Michigan conceived taking its current MMIS through a refinement process
to transform into a service that can be offered to other states. This private cloud MMIS
service will be known as Medicaid Management Information System as a Service or
MaaS.
Per the definitions provided by the National Institute of Standards and Technology (NIST)
in Special Publication 500-292 entitled “NIST Cloud Computing Reference Architecture,”
the envisioned MaaS implementation will be a multi-tenant (community), private cloud.
The services of the MaaS could be provided to multiple states from a cloud service
infrastructure that is dedicated solely to delivering the MaaS.
States would use the service in a largely as-is manner, and instead of following a
traditional DDI process, a Configuration Conversion and Deployment (CCD) process will

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 43
be conducted. This model represents considerable savings in terms of time and cost
over the DDI approach of a traditional MMIS installment.
The Illinois HFS entered into an Intergovernmental Agreement (IGA) with the State of
Michigan Department of Health and Human Services (MDHHS) on December 12, 2012
to determine the feasibility of the viability and practicality of a shared MMIS Enterprise
between the two states. Prior to the IGA, Illinois and Michigan signed a Memorandum of
Understanding on August 20, 2012, entering into formal planning discussions about
MaaS under an IGA.
HFS submitted requests for enhanced FFP through Planning Advanced Planning
Document Updates (PAPDUs) and As Needed Planning Advanced Planning Document
Updates (AN-PAPDUs). The Illinois Core MMIS PAPD included three projects:
• Electronic Data Warehouse Implementation
• MMIS Core Planning Activities
• Provider Enrollment (PE) Implementation
On July 1, 2020, MDHHS and HFS agreed to amend the IGA to pursue
closeout/shutdown of the shared MMIS project. As of September 2021, MDHHS and
Illinois completed the majority of the project closeout activities and transferred the Illinois
Provider Enrollment and eMIPP modules and data from the Michigan infrastructure to
Illinois’ new MMIS inf rastructure, an Amazon Web Services Cloud-based architecture.
Remaining closeout activities, which include the conversion of the Single Sign-On
product MiLogin to ILLogin via Okta, are expected to complete by June 30, 2022.
Illinois signed a four-year contract with CNSI on March 25, 2021, to complete the
implementation of remaining IMPACT components (Core) and to continue support for the
existing components (PE and eMIPP). CMS approved the contract, which includes
support for core claims processing, encounter data processing, managed care
coordination and CNSI’s Fast Healthcare Interoperability Resources (FHIR) based
interoperability solution.
3.2.1 Provider Enrollment System Project
The IMPACT project is a three-phase initiative to deliver to HFS the MDCH state-of-the-
art federally certified MMIS through a cloud-enabled service. The first phase, Electronic
Health Record (EHR) - electronic Medicaid Incentive Payment Program (eMIPP), was
completed in November 2013. The second phase, completed in July 2015, was the
implementation of the Provider Enrollment System. The third phase is the full
implementation of a cloud enabled MMIS, referred to as the Cloud Enablement Phase
scheduled for full completion in 2020.
The Provider Enrollment System was initially implemented as a stand-alone system and
is integrated with existing HFS legacy MMIS. The implementation was the first step
toward the full cloud enabled MMIS for the State of Illinois.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 44
3.2.2 Enterprise Data Warehouse (EDW) Project
Illinois will implement the Enterprise Data Warehouse (EDW) Project in parallel with the
MMIS implementation activities. The EDW Project, although included in the PAPDU and
approved by CMS as a pre-MMIS implementation activity, is considered a separate sub-
project that includes:
• Analysis and implementation of the EDW Reports and Queries
• Design and data analysis of the Michigan MMIS / Illinois EDW environment
• Governance and security planning for the Illinois EDW
• Metadata analysis of the Michigan EDW
• Extending the Informatica and Teradata Illinois EDW platform with test
environments that can support the new MMIS implementation
• Establishing the telecommunications connectivity from the Michigan Data Center
to the Illinois Data Center for EDW transmissions and test data transmissions
• Implementation of the EDW Data Analytics Platform
• Fraud and abuse detection analytics
The Department of Health & Human Services, Office of Inspector General (OIG) has
developed a series of fraud and abuse detection analytics based on fee-for-service /
provider-based criteria. As the provider enrollment data will change substantially upon
migration to the Michigan MMIS and as Integrated Care models are introduced into the
EDW, these analytics will need to be reviewed and modified based on changes to the
EDW to accommodate the new MMIS data structures.
An initial set of federal reports were migrated to the EDW environment in January 2012
as part of IL-Mar Phase 1. More of the federal non-financial reports will be migrated to
the EDW environment as part of IL-Mar Phase 2. This will continue the standardization
of all federal reporting onto the IL-MAR/Informatica based platform within the Illinois
EDW environment.
3.2.3 Background and Purpose
The State of Illinois has embarked on a project to replace its existing MMIS. The current
legacy MMIS system is maintained and operated by the State. It was fully implemented
in 1982 and was built to support a fee-for-service Medicaid program. It currently serves
approximately 3.15 million customers and over 62,000 providers, and it processes 88.8
million claims per year, for a total in excess of $13.18 billion.
3.2.4 Cloud Approach
Cloud-based technology allows multiple consumers to share a hardware and software
operating model while maintaining segregation of data and business rules. A single cloud
computing infrastructure can serve many clients more efficiently. Multiple subscribers
can leverage a single computing infrastructure more efficiently by requiring fewer
servers, less duplicative system administration staff and consolidated networking

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 45
services. Each subscriber merely pays for a share of the overall services instead of
requiring a completely duplicative computing environment.
IMPACT has already successfully implemented eMIPP and Provider Enrollment on the
Michigan infrastructure. The final phase is the full implementation of a cloud enabled
MMIS Core.
Cloud implementation of an existing successful MMIS will provide a system capable of
meeting the requirements of state customers with varying needs. This will result in a
system that can be customized or configured more easily for future states wishing to use
this shared model. A more open and configurable system allows for faster and more
simplified onboarding of future states. If additional states subscribe to the cloud model,
shared savings through leveraging existing systems and resources will allow for reduced
implementation and operating costs to states as well as CMS. Changes in policy can be
programmed into a single system and potentially applied to several subscribing state
workflow models with a single vendor development effort.
Example Cloud-Enabled Model
FIGURE 2 2 – Cloud Model
DEG
Exchange Gateway
Storage
SAN & NAS
Monitoring
Hardware
Servers
Shared Infrastructure Services
Software
Licensing
Telecom
Networking Disaster Recovery
Web Phone Mobile Notifications Dashboard
Shared Mediation Layer
Dynamic binding/routing, access control, metering, auditing
FileNet
Document Repository
EDI
Validation & Translation
Credentialing
Provider
Siebel
CRM
Shared Common Services
Cognos
Reporting
Interfaces
File Exchanges
RuleIT
Grouper
ClaimsSure
Business Layer
App Instance - Tenant A App Instance- Tenant B
Database Layer
IaaS
PaaS
Tenant B
Tenant B
Tenant B
Tenant A
Tenant A
Tenant A
Tenant A
Tenant - B
SaaS
COTS /
Shared DB
Presentation Layer
Tenant A
Tenant - B
Core Functions Core Functions
Configurable
Module
Tenant Specific
COTS
eMIPP / Add-On
Module
Tenant Specific
Features
Configurable
Module
Tenant Specific
COTS
eMIPP / Add-On
Module
Tenant Specific
Features
Code ManagementInfrastructure and Services Management
Single Sign-On

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 46
3.3 Governance Structures
HIEs have not fared well in Illinois. The Central Illinois Health Information Exchange
(CIHIE) which serviced a region running from the eastern center to the northeastern area
of the state stopped providing services in February of 2019. The organization explained
to their health system members that their investment in CIHIE was becoming
“duplicative”. At the time, 26 Illinois hospitals were connected to CIHIE, with another 6
connections in the planning stages. CIHIE also connected 20 primary and specialty care
clinics, home health and behavioral clinics in addition to over 65 long term care facilities.
Until mid-2016, HFS had a strong understanding of another RHIO, Metro-Chicago HIE
(MCHIE). This RHIO was projected to have approximately 70% of the Illinois provider
market share. MCHIE’s technical vendor, Sandlot Solutions, abruptly went out of
business in 2016, disrupting MCHIE operations. In late 2016, MCHIE ceased operations.
Providers have turned instead to vendor mediated exchanges such as Commonwell,
Care Everywhere, Careequality, eHealth Exchange and Epic Care Everywhere.
In January 2018, the Office of the National Coordinator for Health Information
Technology released the Trusted Exchange Framework and Common Agreement
(TEFCA) draft. TEFCA aims to advance nationwide interoperability through a set of
principles designed to facilitate trust among authorized participants and complement
emerging national frameworks that support exchange across multiple networks. A key
goal is to enable providers, hospitals, and other stakeholders to exchange data across
organizational boundaries. Other goals center on improving patient access to their data
and encouraging population-level data exchange.
The HealthChoice Illinois ADT implementation has gone very well as 182 hospitals, 463
Skilled Nursing Facilities, 6 MCOs, 13 Specialized Mental Health Rehabilitation Facilities
(SMHRF), 10 Intermediate Care Facility/Developmental Disabilities (ICFDD) and 22
Supportive Living Facilities have been connected to the HealthChoice Illinois ADT
system. This program has reestablished provider confidence in the State to understand
the types of systems that are needed to connect healthcare entities. The State, with
the help of HITECH funding, encouraged participation by reimbursing providers for their
startup connectivity costs. A similar (MES funded) program in the future could help
bring in another large quantity of providers. The MES funding will also target returning
ADT notifications to contributing providers. HFS, in conjunction with sister agencies
DPH and DHS, hopes to expand the HL7 notifications available by the system to include
lab results and Rx notifications.
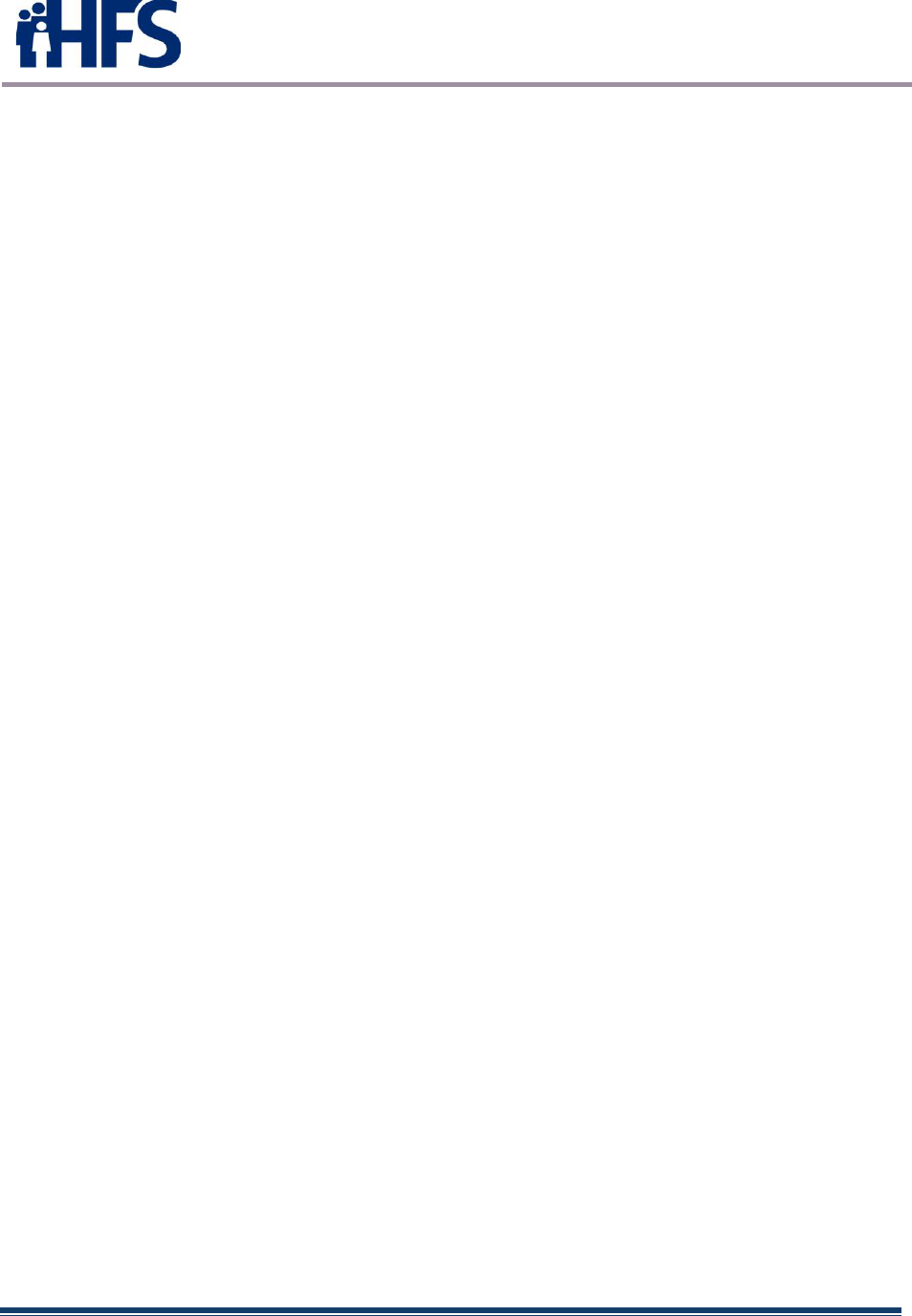
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 47
4 ADMINISTRATION AND OVERSIGHT
4.1 Promoting Interoperability Program Status
Attestations for the Illinois Medicaid Promoting Interoperability Program were taken from 2011
through 2021. In this timeframe 27,720 payments were made for 9,339 unique eligible
professionals totaling over $350.1 million. Between 2011 and 2017, 554 payments were made
to 174 unique eligible hospitals totaling over $314.9 million. All 2021 attestations have been
paid.
Besides incentive payments, HITECH funding provided for:
Public Health Registries – Staffing and equipment for the Illinois Department of Public
Health and the Illinois Department of Human Services to increase providers on-boarded to
the following public health registries:
• I-CARE (Illinois Immunizations Registry)
• I-NEDSS (Illinois Disease Surveillance System\Electronic Lab Reporting (ELR))
• ISSS (Illinois Syndromic Surveillance System)
• ISCR (Illinois State Cancer Registry)
• PMP (Prescription Drug Monitoring Program)
Prescription Drug Monitoring Program – In addition to funding for DHS staffing and
equipment, HITECH and the SUPPORT ACT provided additional funding for on-boarding,
allowing 600+ systems to be connected at reduced cost to the provider. The PI program
assisted with payment of the Prescription system vendor which implemented a plan to
connect with the various EHR vendors used by the providers.
HealthChoice Illinois ADT – HITECH funding assisted with vendor costs and
reimbursements to providers for some connection costs. These funds greatly increased the
number of providers onboarded since July 1, 2021.
At this time, no funding replacements for HITECH have been made for these projects. HFS
anticipates requesting MES funding or additional SUPPORT ACT funding for these projects in
the future. Any requests will include outcome measures as outlined in revised CMS processes.
4.2 Audit Status
Illinois has completed over 1650 audits covering the 2011-2019 program years (as of February 10,
2021). Illinois needs to complete audits for program years 2017-2021. A schedule has been
outlined by HFS Office of the Inspector General (OIG) to complete the audits in FFY2023.
Completion of these audits is the main reason for Illinois’ continued HITECH funding request for
FFY2022-FFY2023.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 48
An updated audit plan, which included updates subsequent to Stage 3 legislation – including
end-of-program considerations was approved by CMS in a letter received on May 20, 2021.
The approval was retroactive to March 24, 2021.
4.3 Remaining Illinois Medicaid Promoting Interoperability Activities
Anticipated activities for the Illinois Medicaid Promoting Interoperability Program for FFY2022-
FFY2023 include the following:
• Complete any necessary IAPD or SMHP requests to CMS
• Complete 2021 Meaningful Use Annual Report by May 30, 2022.
• Complete program audits for program years 2017-2021.
• Maintain eMIPP system, including making enhancements as necessary, for auditing use
through September 30, 2023.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 49
5 EHR INCENTIVE PROGRAM AUDIT STRATEGY
The revised Audit Plan was submitted to federal CMS for approval on March 24, 2021.
This audit plan brings the program up to date through Stage 3 legislation and includes
end of program considerations. This standalone document was approved by CMS on
May 20, 2021 – retroactive to the March 24, 2021, date.

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 50
6 HIT ROADMAP
6.1 Pathway to post-HITECH operations
HFS recently completed the 2021-2024 Comprehensive Medical Program Quality
Strategy, which lays out the purpose, objectives, mission and goals of Medical Programs.
The Quality Strategy is discussed below (section 6.1.1) to give a perspective on HFS’
future vision.
During operation of the Illinois Medicaid Promoting Interoperability Program, Illinois kept
the HITECH and MES funding streams separate. The SUPPORT ACT was introduced
to HITECH staff and was used with regard to the Prescription Drug Monitoring Program
run by DHS. The SUPPORT ACT funding was presented as an MES request, as directed
by CMS. All other aspects of the program requested only HITECH funding. As
discussed in section 4.1, programs that received HITECH funding included:
• Public Health Registries
• Prescription Drug Monitoring Program
• HealthChoice Illinois ADT
HFS has no current plans to request MES to follow HITECH f unding in early FFY2022.
However, there may be opportunities to request MES funding with regard to each of
these programs. Discussions with these Agencies have only occurred as possibilities
for additional funding and have not been solidified. Some examples of these
opportunities are also discussed below.
6.1.1 Comprehensive Medical Programs Quality Strategy
HFS has defined a Quality Framework within the 2021-2024 Comprehensive Medical
Programs Quality Strategy:
6.1.1.1 Purpose
The Illinois Department of Healthcare and Family Services (HFS) developed a
transformative person-centered, integrated, equitable Comprehensive Medical Programs
Quality Strategy (Quality Strategy) designed to improve outcomes in the delivery of
healthcare at a community level. The Quality Strategy provides a framework to
accomplish HFS’ mission.
6.1.1.2 Objectives
Our transformation puts a strong new focus on equity, prevention, and public health; pays for
value and outcomes rather than volume and services; proactively uses analytics and data to drive
decisions and address health disparities; and works to move individuals from institutions to the
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 51
community in an effort to keep individuals in the least restrictive environment and to keep them
more closely connected with families and communities.
Figure 23 Equity
6.1.1.3 Mission
HFS is committed to improving lives by addressing social and structural determinants of health,
by empowering customers to maximize their health and well-being, and by maintaining the highest
standards of program integrity on behalf of Illinoisans. HFS is committed to making equity the
foundation of quality improvement.
6.1.1.4 Goals
Better Care
1. Improve population health.
2. Improve access to care.
3. Increase effective coordination of care.
Healthy People/Healthy Communities
4. Improve participation in preventive care and screenings.
5. Promote integration of behavioral and physical healthcare.
6. Create consumer-centric healthcare delivery system.
7. Identify and prioritize reducing health disparities.
8. Implement evidence-based interventions to reduce disparities.
9. Invest in the development and use of health equity performance measures.
10. Incentivize the reeducation of health disparities and achievement of health equity.
Affordable Care
11. Transition to value- and outcome-based payment.
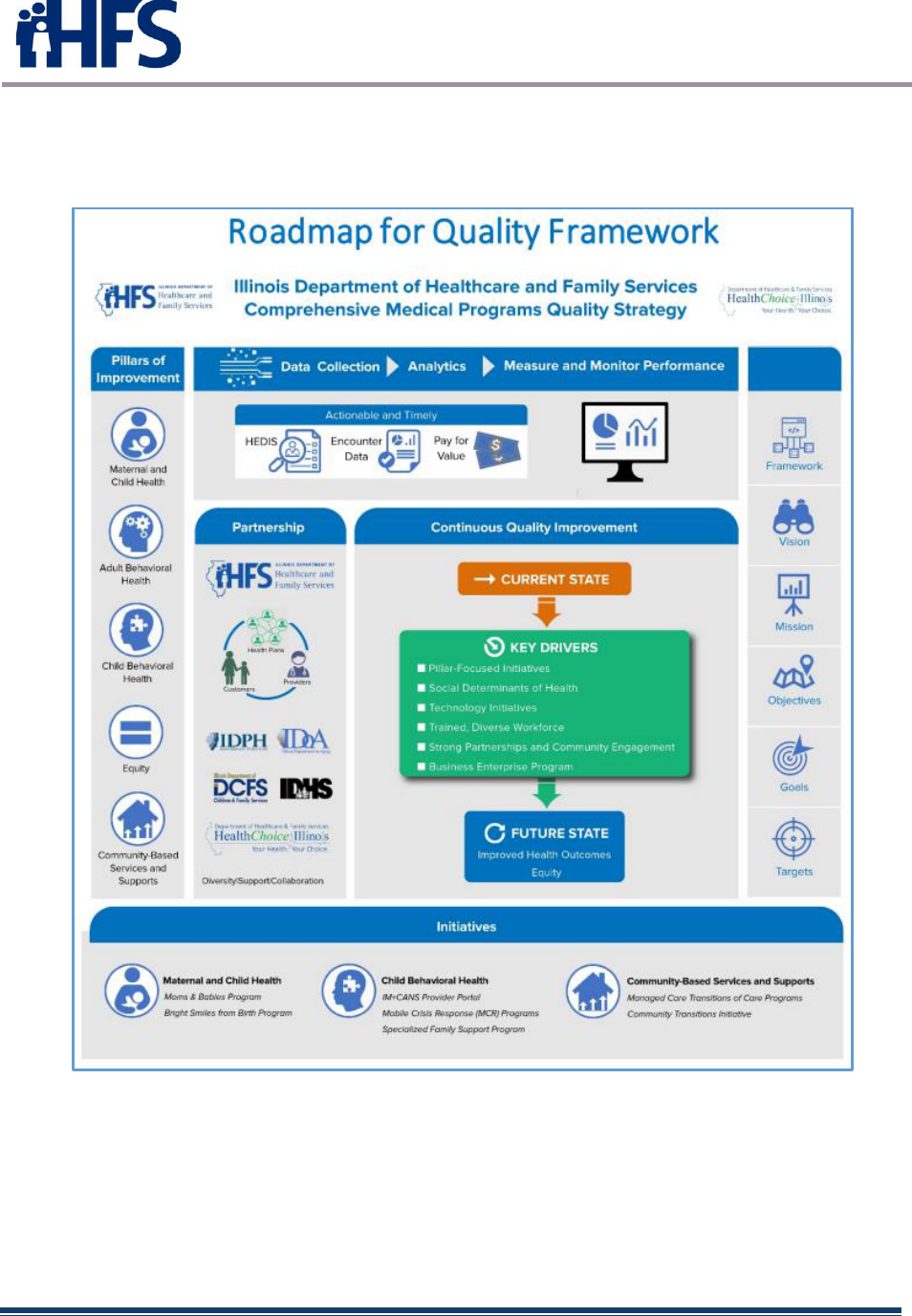
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 52
12. Deploy technology initiatives and provide incentives to increase adoption of
electronic health records (EHRs) and streamline and enhance performance reporting,
eligibility and enrollment procedures, pharmacy management, and data integration
Figure 24 – Roadmap forQuality Framework
6.1.1.5 Vision for Improvement – Program Goals
The vision for improvement and program goals are inclusive of the populations served by
Medicaid, including women and infant health, consumers with behavioral health needs,
consumers with chronic conditions, and healthy children and adults with a central focus on health
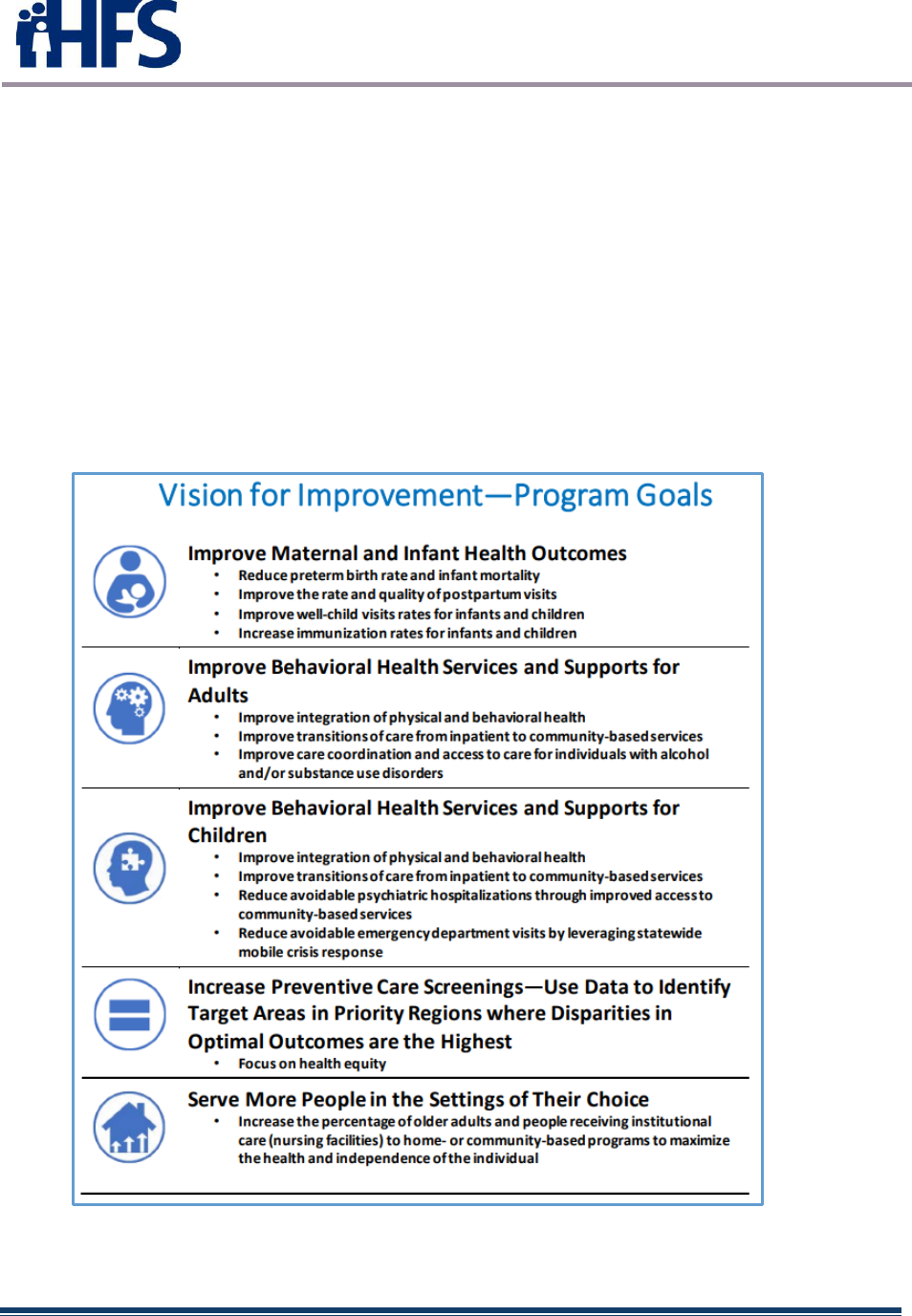
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 53
equity. The HFS Quality Strategy framework prioritizes equity across all program goals as the
ultimate aim for improvement efforts by analyzing data to strategically pinpoint improvement
needs.
As the framework demonstrates, HFS is committed to making equity the foundation of everything
it does. HFS defines equity as providing every employee, individual, community, or population
what is needed to succeed, so everyone can reach their full potential by examining differences in
outcomes for various populations and working to mitigate negative impacts. In the pursuit of
equity, HFS will identify appropriate equity tools to assess the effectiveness of its programs. A
key component of equity is incorporating enterprises that are culturally competent with the
capability of mitigating challenges across the continuum of healthcare, including the social and
structural determinants of health. The State of Illinois’ Business Enterprise Program is an integral
part of addressing equity, and the goals of the program will be incorporated in how quality is
measured.
Figure 25 – Vision for Improvement Goals

State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 54
6.1.2 HealthChoice Illinois ADT
HFS implemented its “Provider Reimbursement Plan” for potential ADT contributors with
some success in 2021. Because the reimbursement deadline coincided with the end
of HITECH funding on September 30, 2021, some providers did not make the deadline.
If HFS were to enact a similar program using MES funding, we could expand on our
growing list of ADT contributors. The HealthChoice Illinois ADT project could also be
assisted with MES funding directed towards
• Inception of data to contributor EHR systems
• Vendor payments
• Tableau reporting development/analytics/expansion
• EDW storage, analytics and other considerations
• Portal access expansion
• Other Agency program integration to ADT (PMP, ELR)
• Quality Strategy staffing, data analytics, metrics development
• Staffing to assist with any of the above
HFS would pair such requests with outcome measure expectations as directed by CMS.
6.1.3 Prescription Drug Monitoring Program
HFS could assist DHS’ Prescription Drug Monitoring Program with MES or SUPPORT
ACT funding. Funding possibilities could include:
• Integration with ADT (follow-ups for ED visits involving prescriptions, etc.)
• Continued connectivity of State EHR systems to PMP
• PMP Vendor payments assisting with integration of ADT or PMP connectivity.
• Staffing to assist with any of the above
6.1.4 Public Health
HFS could assist DPH with MES or SUPPORT ACT funding. Funding possibilities could
include:
• Integration with ADT
o ORU HL7 messages (Observation Result)
o ORM HL7 messages (Order Entry)
o Rx RDE HL7 messages (Pharmacy/Treatment Encoded Order)
o SIU HL7 messages (Scheduling Information Unsolicited)
o Continuity of Care Documents
o Duplication of information on hospitals
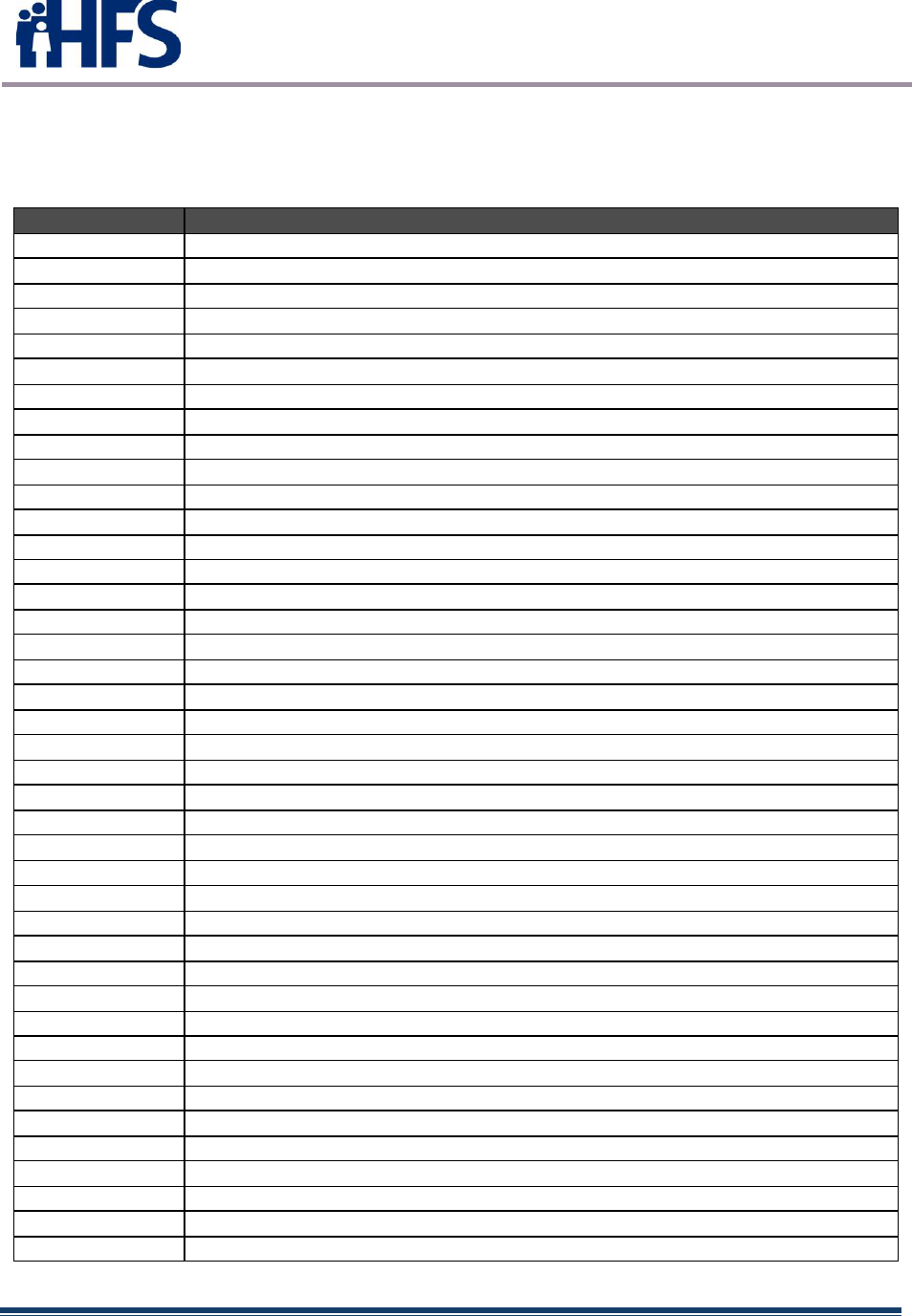
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 56
APPENDIX B: LIST OF ACRONYMS
The following acronyms are used throughout this document:
Acronym
Definition
AIU
Adopt, Implement or Upgrade
ABCD III
Assuring Better Child Health and Development III
ABP
American Board of Pediatrics
ACA
Patient Protection and Affordable Care Act
ACO
Accountable Care Organization
ADHD
Attention Deficit Hyperactivity Disorder
ADT
Admit Discharge Transfer
AHS
Automated Health Systems
AHRQ
Agency for Healthcare Research and Quality
ALJ
Administrative Law Judge
AOA
American Optometric Association
AOBP
American Osteopathic Board of Pediatrics
AR
Accounts Receivable
ARRA
American Recovery and Reinvestment Act
AVRS
Automated Voice Response System
BCHS
Bureau of Comprehensive Health Services
BCP
Bureau of Claims Processing
BFO
Bureau of Fiscal Operations
BHIP
Behavioral Health Integration Project
BIP
Broadband Initiatives Program
BMC
Bureau of Managed Care
BMCHP
Bureau of Maternal and Child Health Promotion
BMI
Body Mass Index
BMI
Bureau of Medicaid Integrity
BPRA
Bureau of Program and Reimbursement Analysis
BRDA
Bureau of Rate Development and Analysis
BRFSS
Behavioral Risk Factor Surveillance System
BTOP
Broadband Technology Opportunities Program
CAH
Critical Access Hospital
CAI
Community Anchor Institutions
CBHA
Community Behavioral Healthcare Association
CCN
(Federal) CMS Certification Number
CDC
Centers for Disease Control and Prevention
CDPH
Chicago Department of Public Health
CFR
Code of Federal Regulation
CH&P
Community Health and Prevention Services
CHESS
Chicago Health Event Surveillance System
CHIP
Children’s Health Insurance Program
CHIPRA
Children's Health Insurance Program Reauthorization Act
CHITREC
Chicago Health Information Technology Regional Extension Center
CHPL
Certified HIT Product List
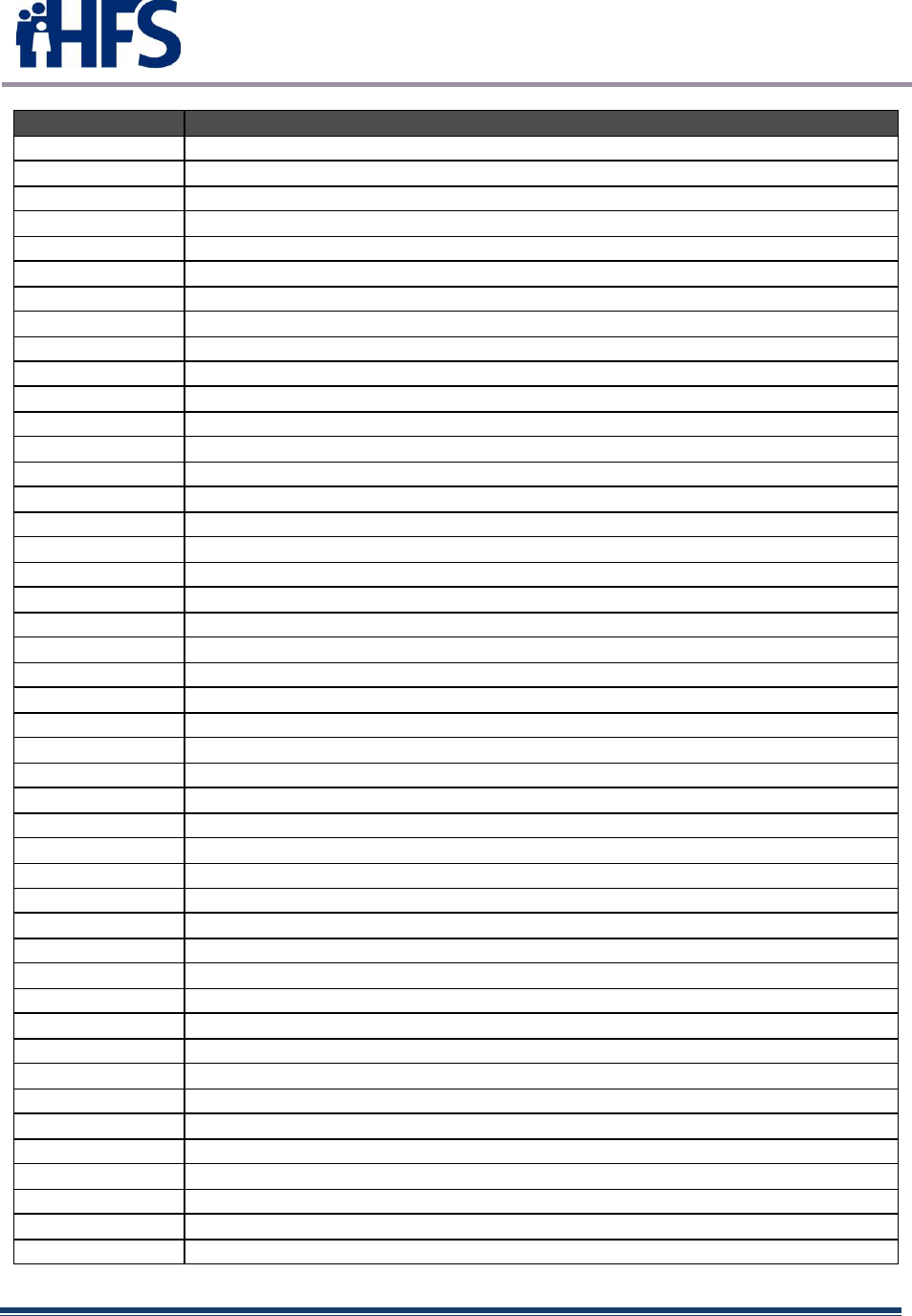
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 57
Acronym
Definition
CLIA
Clinical Laboratory Improvement Amendments
CMT
Collective Medical Technologies
CMS
Centers for Medicare & Medicaid Services
(Federal) CMS
Centers for Medicare & Medicaid Services
(Illinois) CMS
Illinois Department of Central Management Services
CQM
Clinical Quality Measure
DATA
Dekalb Advancement of Technology Authority
DCEO
Illinois Department of Commerce and Economic Opportunity
DCFS
Illinois Department of Children and Family Services
DHS
Illinois Department of Human Services
DMP
Division of Medical Programs
DPH
Illinois Department of Public Health
DPSQ
Division of Patient Safety and Quality
DRA
Deficit Reduction Act
ECC
Electronic Claims Capture
ECP
Electronic Claims Processing
ED
Emergency Department
EDW
Enterprise Data Warehouse
EFT
Electronic Funds Transfer
EH
Eligible Hospital
EHR
Electronic Health Record
EMR
Electronic Medical Record
EP
Eligible Professional
EVE
Eligibility Verification and Enrollment
EVV
Electronic Visit Verification
FFP
Federal Financial Participation
FFS
Fee-for-Service
FONSI
Finding of No Significant Impact
FQHC
Federally Qualified Health Center
FTP
File Transfer Protocol
HCCN
Health Center Controlled Network
HEDIS
Healthcare Effectiveness Data and Information Set
HFS
Illinois Department of Healthcare and Family Services
HHCS
Home healthcare services
HIE
Health Information Exchange
HIPAA
Health Insurance Portability and Accountability Act
HISPC
Health Information Security and Privacy Collaboration
HIT
Health Information Technology
HITEC
Health Information Technology Extension Center
HITECH
Health Information Technology Economic and Clinical Health Act
HITPO
Health Information Technology Project Office
HL7
Health Level Seven
HMA
Health Management Associates
HMO
Health Maintenance Organization
HRSA
Health Resources and Services Administration
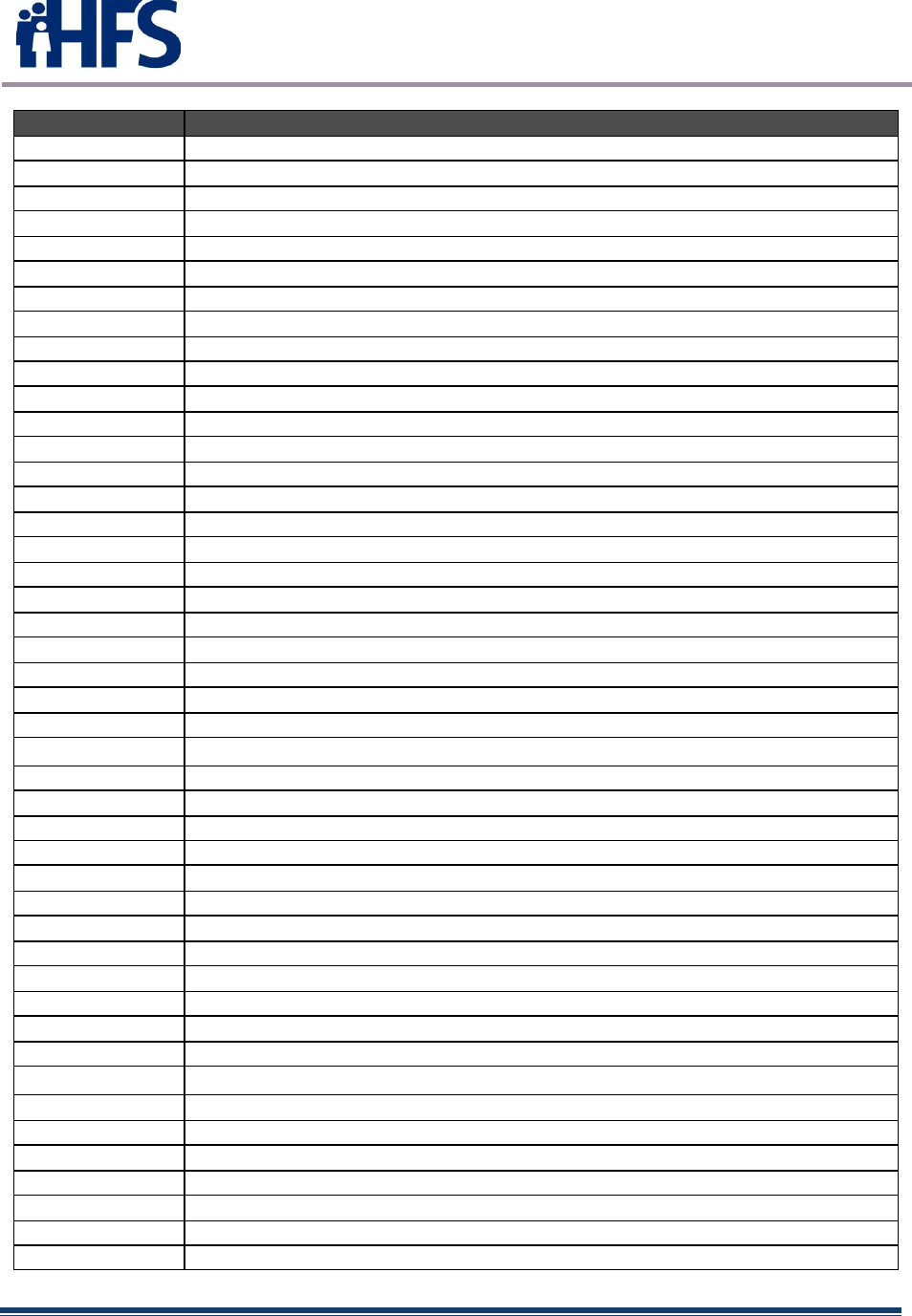
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 58
Acronym
Definition
IAPD
Implementation Advance Planning Document
IAPDU
Implementation Advance Planning Document Update
IARF
Illinois Association of Rehabilitation Facilities
IBPO-EC
Illinois Broadband Opportunity Partnership for East Central Illinois
ICAHN
Illinois Critical Access Hospital Network
I-CARE
Illinois Comprehensive Automated Immunization Registry Exchange
ICD-10-CM
International Classification of Diseases, 10th Revision, Clinical Modification
ICD-10-PCS
International Classification of Diseases, 10
th
Revision, Procedural Coding System
ID
Identification
IDOT
Illinois Department of Transportation
IDPH
Illinois Department of Public Health
IDVA
Illinois Department of Veterans Affairs
IHA
Illinois Hospital Association
IHE
Integrating the Healthcare Enterprise
ILCS
Illinois Compiled Statutes
ILHIE
Illinois Health Information Exchange
IL-HITREC
Illinois Health Information Technology Regional Extension Center
I-NEDSS
Illinois National Electronic Disease Surveillance System
I/P
Inpatient
IRHN
Illinois Rural HealthNet
IRS
Internal Revenue Service
ISMS
Illinois State Medical Society
IT
Information Technology
LAN
Local Area Network
LIS
Low-Income Subsidy
LOINC
Logical Observation Identifiers Names and Codes
LTACH
Long-term Acute Care Hospital
LTC
Long-Term Care
MAC
Medicaid Advisory Committee
MAR
Management and Administrative Reporting
MARS
Management and Administrative Reporting Subsystem
MCO
Managed Care Organization
MDS
Minimum Data Set
MDW
Medical Data Warehouse
MEDI
Medical Electronic Data Interchange
MFCU
Medicaid Fraud Control Unit
MIPPA
Medicare Improvements for Patients and Providers Act
MITA
Medicaid Information Technology Architecture
MMCE
Medicaid Managed Care Entity
MMIS
Medicaid Management Information System
MPD
Master Provider Directory
MPI
Master Patient Index
MSIS
Medicaid Statistical Information System
MSP
Medicare Savings Programs
MTA
Medical Trading Area
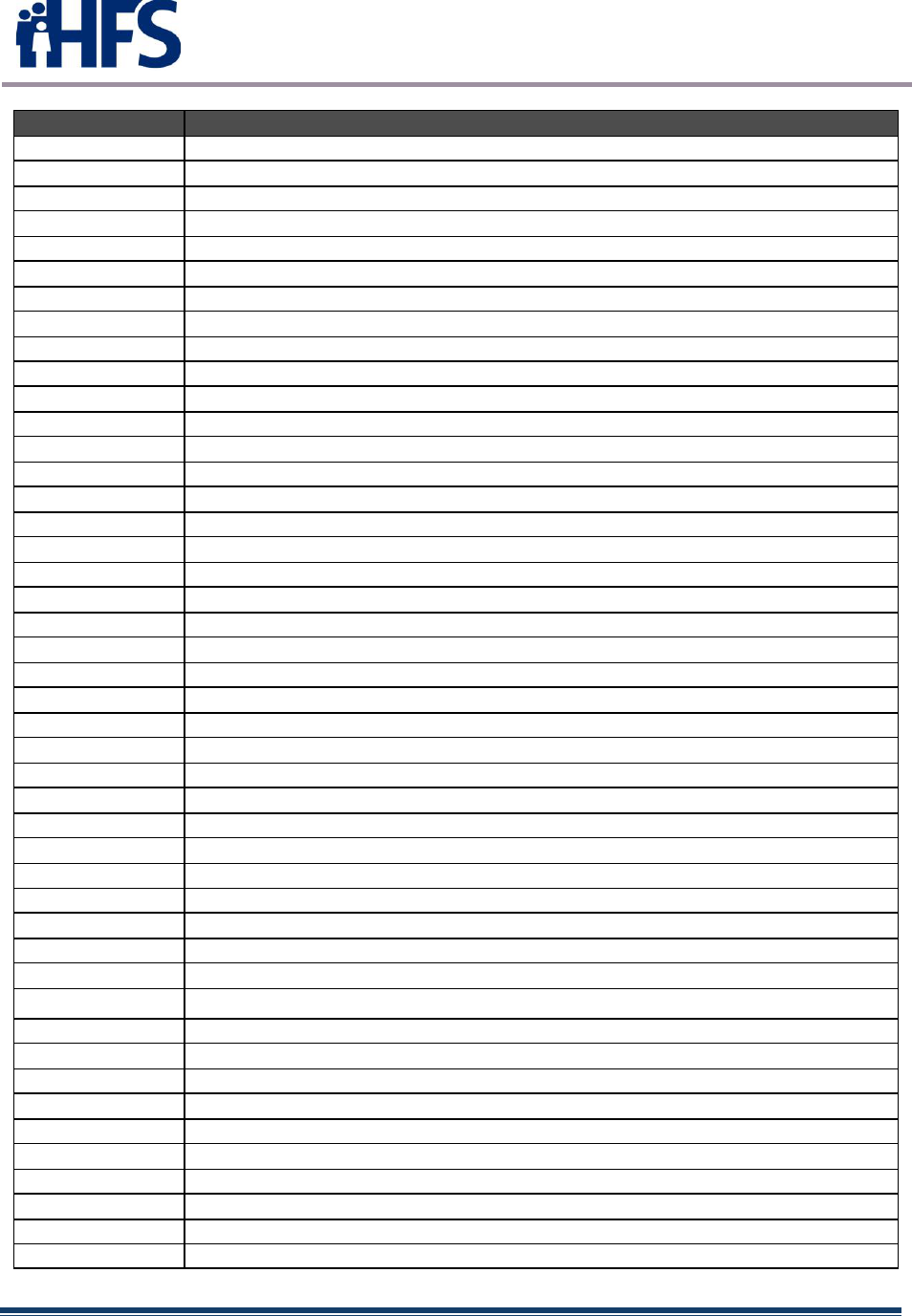
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 59
Acronym
Definition
MTG
Medicaid Transformation Grant
MU
Meaningful Use
NCQA
National Committee for Quality Assurance
NCPDP
National Council for Prescription Drug Programs
NHIN
Nationwide Health Information Network
NICU
Neonatal Intensive Care Unit
NIU
Northern Illinois University
NPI
National Provider Identifier
NPPES
National Provider and Plan Enumeration System
NTIA
National Telecommunications and Information Administration
OGC
Office of General Counsel
GOHIT
Illinois Governor’s Office of Health Information Technology
OIA
Office of the Internal Auditor
OIG
Office of the Inspector General
OIS
Office of Information Systems
OME
Otitis Media with Effusion
ONC
Office of the National Coordinator for Health Information Technology
O/P
Outpatient
OSF
Order of Saint Francis
PA
Physician Assistant
PAAS
Programmatic Administrative Accounting System
PBM
Pharmacy Benefit Manager
PCCM
Primary Care Case Management
PCI
Partnership for a Connected Illinois
PCP
Primary Care Provider
PCS
Procedure Coding System; also Personal Care Services
PDMP
Prescription Drug Monitoring Program
PHSA
Public Health Services Act
PICU
Pediatric Intensive Care Unit
PIP
Provider Incentive Payment
POS
Place of Service
PPCP
Priority Primary Care Provider
PPU
Provider Participation Unit
PQRS
Physician Quality Reporting System
PRS
Policy Review System
R&A
Registration and Attestation System
REC
Regional Extension Center
REV
Recipient Eligibility Verification
RHC
Rural Health Clinic
RHIO
Regional Health Information Organization
RLS
Record Locator Service
ROI
Return on Investment
RPR
Recipient/Provider Reference subsystem
RUGS
Resource Utilization Groups
RUS
Rural Utility Service
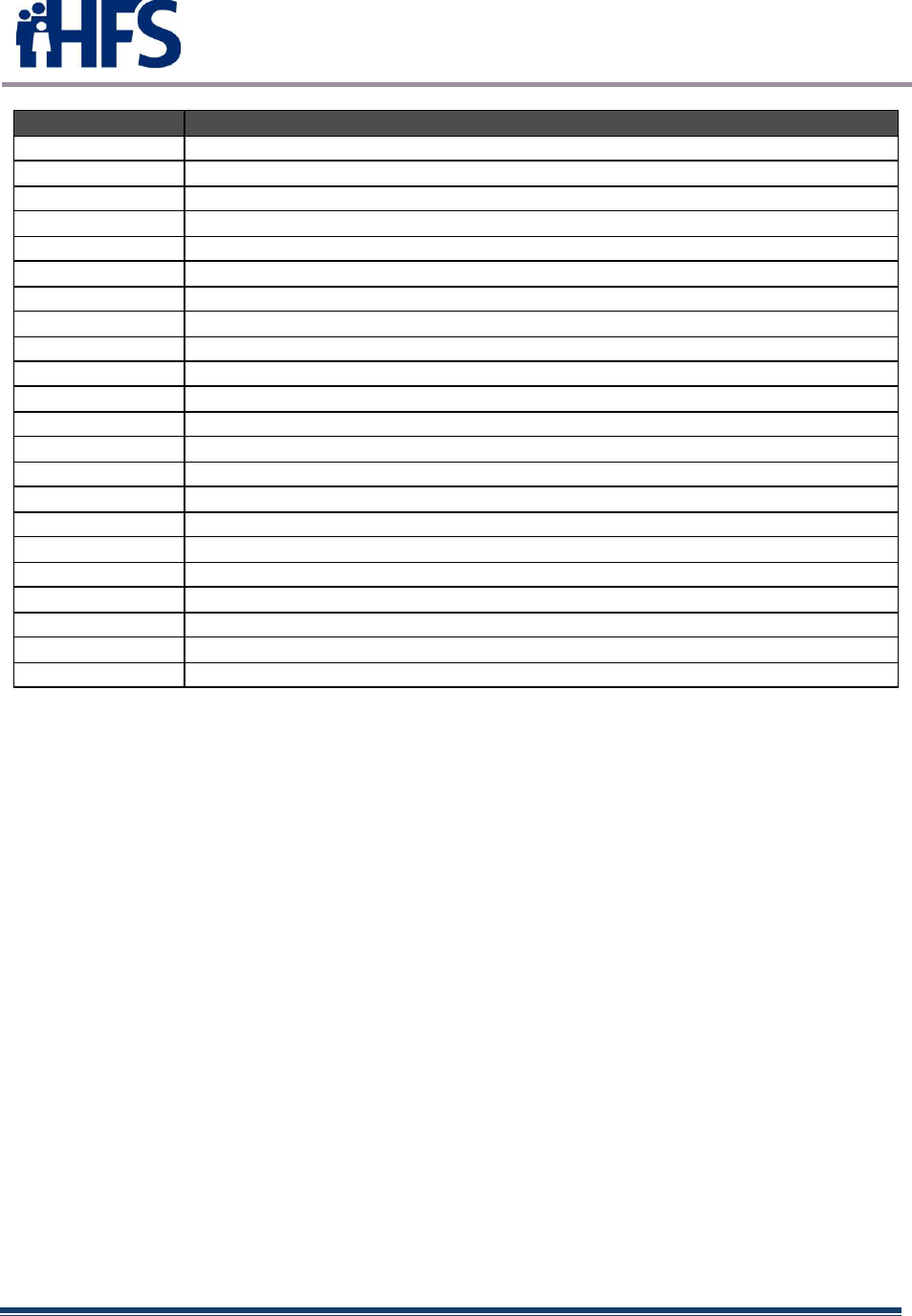
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 60
Acronym
Definition
SAMHSA
Service Administration of Mental Health and Substance Abuse
SAMS
Statewide Accounting Management System
SBDD
State Broadband Data and Development
SEIU
Service Employees International Union
SHARP
Strategic HIT Advanced Research Project
SHIECAP
State Health Information Exchange Cooperative Agreement Program
SHIP
State Health Improvement Plan
SMA
State Medicaid Agency
SMD
State Medicaid Director
SMHPU
State Medicaid Health Information Technology Plan Update
SNOMED
Systematized Nomenclature of Medicine-Clinical Terms
SS-A
State Self-Assessment
SSN
Social Security Number
TIN
Taxpayer Identification Number
TPL
Third-Party Liability
SUR
Surveillance and Utilization Review
UC
Urbana-Champaign
UC2B
UC Big Broadband
UDS
Uniform Data System
US DHHS
United States Department of Health and Human Services
USDA
United States Department of Agriculture
XML
Extensible Markup Language
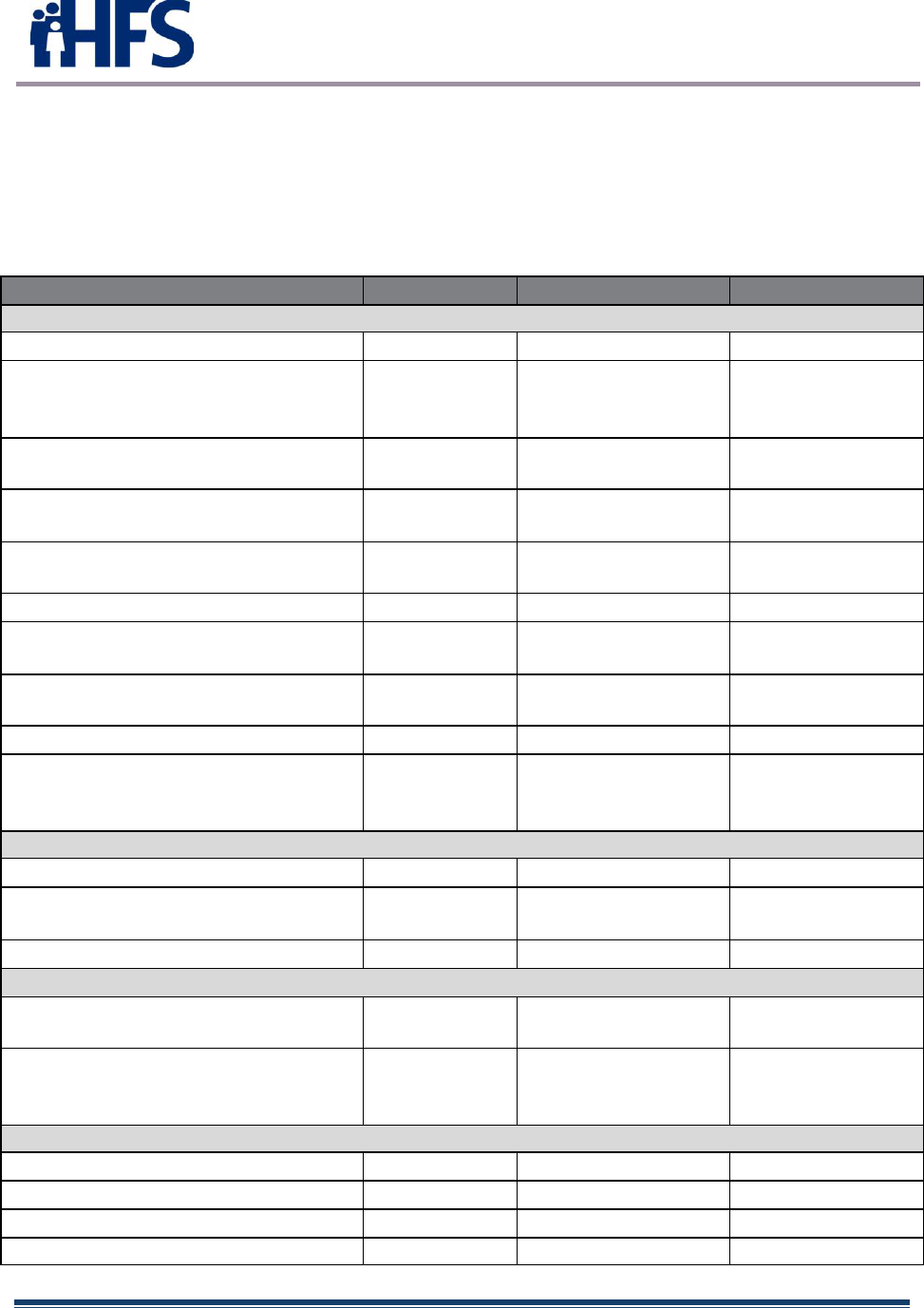
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 61
APPENDIX C: EHR INCENTIVE PROGRAM TASKS
The following table contains the task list for the continued evolution of the EHR Incentive Program.
Remaining tasks are shown in red.
Task list
Activity
Start Date
End Date
Status
PROJECT PLANNING TASKS COMPLETED
Implemented HITPO
10/2010
01/2011
Complete
Contracted with a vendor, Cognosante
(f/k/a Fox Systems), to assist in SMHP and
IAPD development
4/23/2010
5/03/2010
Complete
Developed State’s Incentive Payment Vision
Statement
2/04/2011
3/23/2011
Complete
Conducted EHR Assessment – Medicaid
Providers (Environmental Scan)
8/01/2010
11/30/2010
Complete
Conducted EHR Assessment – Non-
Medicaid Providers (Environmental Scan)
11/01/2010
11/30/2010
Complete
Developed EHR Business Gap Analysis
10/28/2010
12/23/2010
Complete
Developed SMHP to administer incentive
payments for EHR meaningful use
12/1/2010
4/7/2011
Complete
Completed the MITA SS-A Update relating
to PIP program implementation
7/20/2010
10/01/2010
Complete
Submitted Draft SMHP to federal CMS
4/7/2011
4/7/2011
Complete
Received comments from federal CMS;
revised SMHP addressing comments;
resubmitted to federal CMS
6/8/2011
7/1/2011
Complete
Provider Incentive Program (PIP) Implementation
Submit IAPD for federal CMS approval
7/21/2011
7/21/2011
Complete
Develop Policy and Procedures required to
support the PIP program
9/17/2010
10/19/2010
Complete
Define requirements for the system solutions
6/1/2011
7/1/2011
Complete
IAPD/SMHP
Submit revised SMHP to federal CMS for
approval, and annually thereafter
1/20/2012
Ongoing
Ongoing
Provide updated IAPD as necessary
throughout the implementation and
administration of the PIP program
1/20/2012
Ongoing
Ongoing
EHR Incentive Program Implementation
Complete system specifications
8/31/2011
12/31/2011
Complete
Launch Illinois EHR Incentive Pgm website
Complete
Establish new policies for the program
9/17/2010
10/19/2010
Complete
Establish program procedures
9/17/2010
10/19/2010
Complete
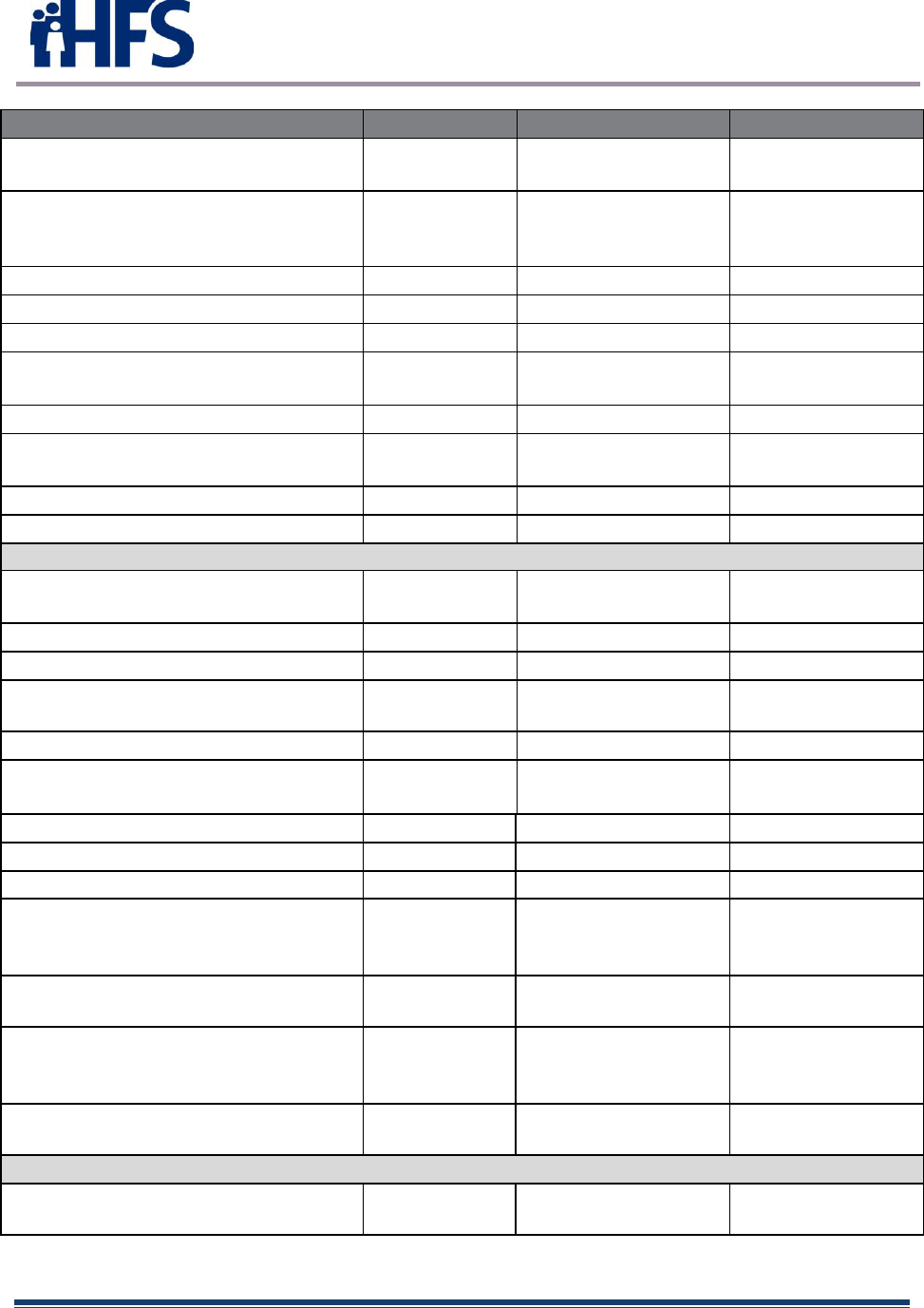
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 62
Activity
Start Date
End Date
Status
Finalize Illinois Rules revisions required for
the PIP program
9/17/2010
1/31/2011
Complete
Execute outreach and communication plan
to support PIP program awareness in
provider community and within HFS
10/20/2010
11/30/2021
Compete
Implement System Updates
7/01/2011
9/30/2011
Complete
Test State/Federal R&A System Interface
Complete
Program Launch
09/2011
09/2011
Complete
Begin Accepting Attestations
Aug 2012 (EH)
Dec 2012 (EP)
Aug-2012 (EH)
Dec 2012 (EP)
Complete
Begin Issuing EHR Incentive Payments
March 2012
March 2012
Complete
Continued EHR Incentive Payments
(Adopt/Implement/Upgrade [A/I/U])
March 2012
12/31/2021
Complete
Audit Process Begins (first audits conducted)
August 2012
August 2012
Complete
Audits updated for Stage 2
4/1/2016
10/11/2016
Complete
Coordinate PIP Program for Phase 2 – Stage 1 Meaningful Use / Year 2 and Year 3 Payments
Conduct Stakeholder discussions on shared
HIE projects
1/20/2012
8/31/2012
Complete
CMS review and approval of MU Screens
4/5/12
2/20/2013
Complete
Define Stage 1 MU requirements
10/1/2012
12/31/2012
Complete
Complete system upgrades to collect, store,
and report on MU measures.
11/1/2012
2/28/2013
Complete
Conduct MU User Acceptance Testing
11/01/2012
2/28/2013
Complete
Accept Provider Stage 1 MU Attestations
Dec 2012 (EH)
Mar 2013 (EP)
Dec 2012 (EH)
Apr 2013 (EP)
Complete
Phase 1 of eMIPP implementation
7/8/2013
11/18/2013
Complete
Phase 2 of eMIPP implementation
11/26/2013
03/28/2014
Complete
Flex rule implementation in eMIPP
10/5/2014
10/31/2014
Complete
Implement Modifications to Stage 1 and
Stage 2 (2015-2017)\Stage 3 Final rule in
eMIPP for 2015-2016 program years
10/1/2015
10/31/2015
Complete
Implement requirements of 2017 IPPS final
rule in eMIPP
8/15/2016
12/15/2016
Complete
Implement Modifications to Stage 1 and
Stage 2 (2015-2017)\Stage 3 Final rule in
eMIPP for 2017 program year
6/3/2016
3/29/2017
Complete
Implement requirements of 2017 OPPS final
rule in eMIPP
11/1/2016
12/15/2016
Complete
Tasks To Be Undertaken
Implement requirements of 2018 IPPS final
rule in eMIPP
9/4/2017
1/1/2018
Complete
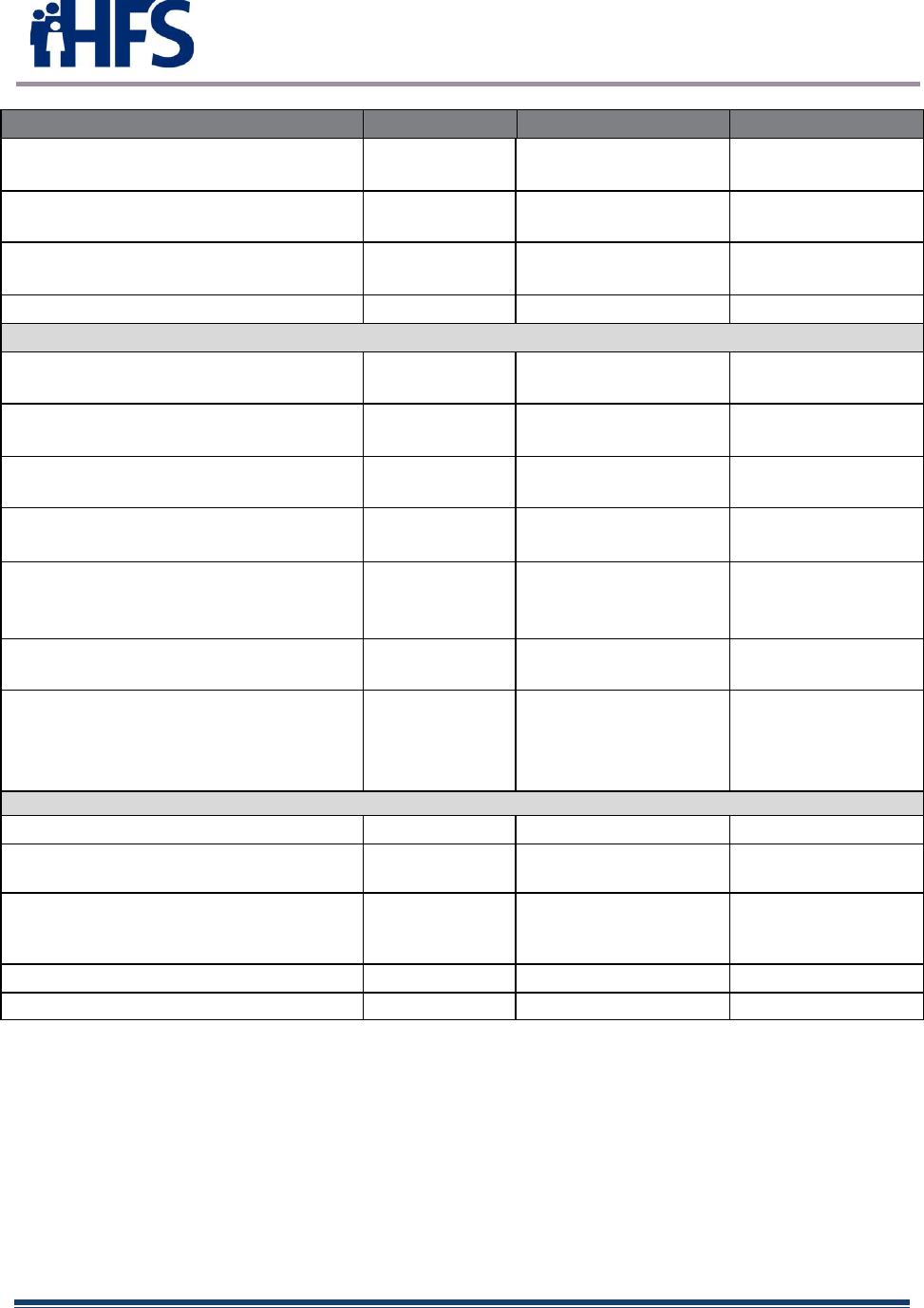
State Medicaid Health Information
Technology Plan Update (SMHPU)
March 30, 2022 Page 63
Activity
Start Date
End Date
Status
Implement modifications to 2018 QRDAIII
Implementation Guide
9/4/2017
1/1/2018
Complete
State determination of MU and tracking of
MU
1/20/2012
12/31/2021
Complete
Develop State’s Vision for MU and Clinical
Data
1/20/2012
12/31/2021
Complete
Quarterly system updates to eMIPP
Complete
ADT Tasks
Vendor shall provide to HFS a written
implementation plan
3 weeks after
contract execution
4/30/2021
Complete
Vendor shall provide to HFS a written
training plan
6 weeks after
contract execution
3/15/2021
Complete
Vendor shall provide written security risk
assessment
1 month after
contract execution
5/25/2021
Complete
Vendor shall provide first quarterly status
report
3 months after
contract execution
Hospitals: 5/10/2021
LTC: 8/2/2021
Complete
Vendor shall ensure that all MCOs are
connected and actively receiving ADT
notification from the system
12 months after
contract execution
10/27/2021
Complete
Vendor shall ensure Web portal is
implemented
5 months after
contract execution
2/25/2021
Complete
Vendor shall ensure that all Vendor
developed system reports to be used by HFS,
MCOs and ambulatory/community
providers are implemented
7 months after
contract execution
3/1/2022
Complete
Post Attestation Closeout Tasks
Ongoing Post-Payment Audits
August 2012
August 30, 2023
Ongoing
Complete 2022-2023 IAPD
5/7/2022
5/7/2022
Submitted to CMS
3/24/2022
Complete 2022 SMHP
1/1/2022
3/31/2022
Scheduled for
submittal by
3/31/2022
Complete 2021 MU Annual Report
4/1/2022
5/30/2022
On schedule
Complete 2023 IAPD
5/7/2023
Not initiated

